Malocclusion
Incorrect bite formation leads to permanent injury to the mucous membranes of the mouth and tongue. As a result, the muscle organ swells and increases in size. Due to constant biting, teeth marks are left on the sides of the tongue.
The disease can be cured only after correcting the malocclusion. To do this, the doctor selects a design to straighten the dentition. For minor violations, patients are prescribed to wear orthodontic plates, trainers, and silicone trays. In case of more serious pathology, the defect is corrected using braces. The course of treatment can take from 3 months to 2 years.
Treatment of desquamative glossitis
Desquamative glossitis does not belong to the category of dangerous diseases with serious consequences. Many parents, seeing that their son or daughter’s tongue is peeling off, panic, fearing that such changes in the mucous membrane could develop into oncological tumors. These fears are completely unfounded. Desquamative glossitis never develops into cancer.
If geographic tongue is a secondary symptom of another, underlying disease, treatment should be comprehensive.
To eliminate discomfort, itching and burning on the mucous surface of the tongue, painkillers can be used. In order to save yourself from discomfort, you must definitely exclude from your diet all spicy, salty, sour, too hot and cold foods.
- Antiseptic rinsing of the mouth is necessary several times a day. For this purpose, special disinfectant medications are used, which are prescribed by the doctor.
- An oil bath gives an excellent effect. You can take sunflower, corn or olive oil, which is heated in a water bath for 20-25 minutes.
- A thorough sanitation of the oral cavity is carried out - timely treatment of carious teeth, gum diseases, systematic cleaning.
- Taking multivitamin complexes will be an effective addition to the course of treatment. But in no case should you choose them yourself - you should definitely consult with a specialist.
Adult men and women are recommended to give up many bad habits - smoking, frequent consumption of strong alcoholic drinks, as well as sweets and other foods with a lot of sugar.
Folded tongue
This is a congenital anomaly in which the tongue is excised by longitudinal and transverse folds, wavy, uneven at the edges. As a rule, the disease is accompanied by an increase in the size of the organ and its thickening; teeth marks can be seen on the sides. Usually the pathology is asymptomatic and does not cause discomfort; pain and inflammation can appear after infectious diseases, with the development of stomatitis or glossitis.
The folded tongue requires good hygienic care, since bacterial plaque easily accumulates in the cracks and creates a convenient environment for the proliferation of pathogenic bacteria. Such a disease is incurable; therapeutic procedures are necessary only when stomatitis and glossalgia develop.
Diagnosis of geographic tongue
As mentioned above, the diagnosis of desquamative glossitis of the tongue is not difficult and may well be based on a visual examination of the oral mucosa. Diagnosis of desquamative glossitis is aimed at identifying the answer to the question - why the tongue may peel off, and is carried out in several ways:
- The first thing that is necessary for a correct diagnosis of the pathology is an examination of the mucous membrane of the tongue to identify characteristic whitish spots and grooves, and a consultation with a dentist.
- A very important place in the diagnosis of desquamative glossitis is occupied by interviewing the patient - his complaints of discomfort, itching and burning in the tongue area. Of course, when diagnosing the disease in young children, this point can be skipped.
- All diseases in the medical history of each individual person must be taken into account.
- If desquamative glossitis is suspected, general blood, stool and urine tests, as well as all other necessary laboratory tests, must be taken.
Liver diseases
In people suffering from serious liver diseases (viral hepatitis, cirrhosis of the liver), the tongue has a characteristic appearance - the mucous membranes are red, hyperemic, the surface is smooth, glossy, the papillae are smoothed. Often such symptoms are accompanied by swelling of the organ and an increase in its size, as a result of which the edges are constantly bitten by the teeth, forming wavy sides.
Among the additional external symptoms, patients note the appearance of spider veins, xanthomatous plaques, and erythema (redness) of the palms on the surface of the skin. Patients complain of pain in the right hypochondrium, nausea, vomiting, indigestion and stool disorders.
The disease must be treated by a general practitioner, infectious disease specialist, surgeon or oncologist.
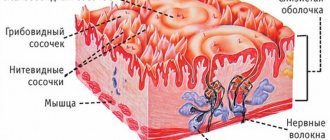
Other diseases of the tongue. Scalloped tongue (K14.8)
Scalloped (toothed tongue) - a change in the shape of the tongue, in which its edges acquire a round-toothed or scalloped outline. Often combined with macroglossia Macroglossia is a pathological enlargement of the tongue; observed as a developmental anomaly or in the presence of a chronic pathological process in the tongue or swelling of the tongue.
Notes
from this subcategory :
– “Other diseases of the lips and oral mucosa” – K13 – “Geographic” tongue” – K14.1 – “Atrophy of the papillae of the tongue” – K14.4 – “Hypertrophy of the papillae of the tongue” – K14.3
– “Congenital macroglossia” – Q38.2
– “Other congenital anomalies of the tongue” – Q38.3
This subcategory includes: scalloped tongue. The following clinical conditions also belong to this code K14.8 and are described under the same code, but in different cards for ease of diagnosis:
All the clinical conditions described above, as a rule, are complications of some pathology. Thus, the code of this subheading should be used as a complication of any underlying disease or as a code for a concomitant pathology. The code can be used as a code for the underlying disease only in case of a preliminary diagnosis.
Description:
As a rule, it has a chronic course. Acutely occurs with swelling of the tongue due to various reasons. When the cause of the swelling is eliminated, it also quickly disappears.
Mobile application “MedElement”
Download the application for ANDROID / for iOS
Mobile application “MedElement”
Download the application for ANDROID / for iOS
The reason for the change in the shape of the tongue is high pressure on the tissue of the tongue, for example during bruxism. Bruxism is involuntary, uncontrolled by consciousness, clenching and grinding of teeth at night (sometimes during the day). It is observed more often in childhood and young age, the habit of sucking the tongue to the teeth, and increased size of the tongue.
In this case, the contours of the teeth are imprinted on the edge of the tongue in the form of oval impressions, which are sometimes bordered by a white, raised scalloped ridge. A serrated tongue may be associated with a distinct white line on the buccal mucosa.
A scalloped tongue can be observed in the following diseases and conditions: – damage to the temporomandibular joint (instability of the lower jaw); – systemic diseases (acromegaly, amyloidosis and others); – hereditary diseases (Down’s disease and others); – hypothyroidism; – parafunctional disorders (bruxism and others); – swelling of the tongue due to other reasons; – may be associated with sleep apnea syndrome due to tongue hypertrophy;
– can be observed in healthy individuals.
Note A scalloped tongue is often described as a specific marker of gastrointestinal disease, for example, sphincter of Oddi dysfunction or some kind of colitis. There is no clear evidence supporting this approach to the etiology of this condition.
For example, in a large cohort study, tongue lesions (not only scalloped tongue) were found: - in diabetes mellitus - in 29.03%; – with hypertension – in 28.63%; – for heart and vascular diseases – in 25.15%; – for hematological diseases – in 17.54%; – for liver diseases – in 23.86%; – for other gastrointestinal diseases – in 22.38%; – in 20.69% of cases, changes in the tongue were associated with tumors. No specific correlations were identified between the type of systemic pathology and the nature of the tongue lesion. The scalloped tongue was the rarest find.
Sign of prevalence: Rare
A scalloped tongue is rare. In a large population study (Hungary, 1995-1999), among 5034 patients with systemic diseases, scalloped tongue was detected in approximately 1.5% of cases (5th place out of 6 different tongue pathologies identified).
According to some studies, the incidence of scalloped tongue in children is almost two times lower than in adults.
This fact confirms the assumption that the prevalence of oral lesions increases with age, which may be associated with prosthetics and other dental care.
discomfort at the edges of the tongue; discomfort on the tip of the tongue; burning along the edges of the tongue; teeth marks on the edges of the tongue; teeth marks on the tip of the tongue; macroglossia The main complaints with a scalloped tongue are discomfort and a slight burning sensation along the edges of the tongue (sometimes).
On examination, the tongue is usually enlarged; On the side surfaces there are imprints corresponding to the teeth. Scalloping of both edges is usually observed, but it may be present only on one side or limited to the part of the tongue that is directly pressed against the teeth.
A scalloped tongue may be associated with the following symptoms:
– anemia, unexplained weight loss, fatigue (indicate possible hypersplenism; Hypersplenism is a combination of an enlarged spleen with an increase in the number of cellular elements in the bone marrow and a decrease in formed elements in the peripheral blood.); - weight gain, lethargy, chills and other symptoms (may indicate hypothyroidismHypothyroidism is a thyroid insufficiency syndrome characterized by neuropsychiatric disorders, swelling of the face, limbs and torso, bradycardia); – pain, discomfort when eating spicy and hot foods, bad breath and other symptoms that may indicate an oral infection; – sleep apnea syndrome Apnea – temporary cessation of breathing, which may indicate macroglossia Macroglossia – pathological enlargement of the tongue; observed as a developmental anomaly or in the presence of a chronic pathological process in the language.
There is no need to diagnose a scalloped tongue other than visual inspection. High-resolution digital photography is useful for assessing process dynamics.
The patient should be referred to a general practitioner. When combining a scalloped tongue with macroglossia, see the subsection “Hyperptrophy of the tongue.”
There are no specific laboratory tests to confirm or refute the diagnosis. Any identified deviations indicate an etiologically significant or concomitant pathology.
In all cases, various tests for infections are useful (syphilis, tuberculosis, actinomycosis Actinomycosis is a chronic infectious disease of humans and animals caused by actinomycetes and characterized by granulomatous damage to tissues and organs with the development of dense infiltrates, the formation of abscesses, fistulas and scars) and, if indicated, genetic tests for congenital diseases.
A scalloped tongue is differentiated from glossitis and tongue atrophy. Complications of a scalloped tongue include: – decubital (bedsore, traumatic) ulcers of the tongue;
– infection of damaged edges with the development of glossitis.
Treatment for scalloped tongue is aimed at eliminating the underlying etiological cause. As symptomatic therapy, the installation of acrylic screens (splints, mouthguards) and consultations with a psychologist (for parafunctional disorders) are of great importance. If there is a pronounced reaction to food, a diet excluding hot, spicy, hard foods is indicated.
Patients usually need consultations with a general practitioner/pediatrician. Consultations with other specialists (neurologist, endocrinologist, otolaryngologist, speech therapist, gastroenterologist) may also be necessary.
A scalloped tongue in itself is not a life-threatening condition. The prognosis is determined by the underlying disease.
Primary prevention has not been developed.
Secondary prevention comes down to preventing infection and consists of careful oral hygiene.
- “Effects of surgical reduction of the tongue” Ueyama Y, Mano T, Nishiyama A, Br J Oral Maxillofac Surg, No. 37(6), 1999
- “Epidemiologic survey of tongue lesions and analysis of the etiologic factors involved” Voros-Balog T, Dombi C, Vincze N, Banoczy J.
, Fogorvosi Szemle journal, No. 92(5), 1999 - “Glossoptosis (posterior displacement of the tongue) during sleep: a frequent cause of sleep apnea in pediatric patients referred for dynamic sleep fluoroscopy” Donnelly LF, Strife JL, Myer CM, Am J Roentgenol., No. 175(6), 2000
- “Glossoptosis-apnea syndrome in infancy” Cozzi F, Pierro A.
, Pediatrics, No. 75(5), 1985 - “Hypoglossal nerve palsy” Ivan WC Tsui, David PN Chan, Hong Kong Med J, vol. 15, No. 3, 2009
- “Mandibular distraction osteogenesis for pediatric airway management” Miloro M., J Oral Maxillofac Surg., No. 68(7), 2010
- “Myasthenia gravis – a rare presentation with tongue atrophy and fasciculation” J. Burch, C. Warren-Gash, V. Ingham, M.
Patel, D. Bennett, KR Chaudhuri, Age and Aging journal, No. 35, 2006 - “Oral mucosal lesions in a representative cross-sectional study of aging Germans” Reichart PA, Community Dent Oral Epidemiol., No. 28(5), 2000
- “Surgical correction of the enlarged tongue” Taher A., The Internet Journal of Head and Neck Surgery, vol.
3, №1, 2008 - “Pierre Robin sequence - an early diagnostic sign of Stickler syndrome (clinical case)” Muzychina A.A., Maleeva I.A., “Medical and social problems of the family”, v. 17, no. 3-4, 2012
If you are not a medical professional:
- By self-medicating, you can cause irreparable harm to your health.
- The information posted on the MedElement website and in the mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: a therapist’s guide” cannot and should not replace a face-to-face consultation with a doctor. Be sure to contact a medical facility if you have any illnesses or symptoms that concern you.
- The choice of medications and their dosage must be discussed with a specialist. Only a doctor can prescribe the right medicine and its dosage, taking into account the disease and condition of the patient’s body.
- The MedElement website and mobile applications “MedElement (MedElement)”, “Lekar Pro”, “Dariger Pro”, “Diseases: a therapist’s reference book” are exclusively information and reference resources. The information posted on this site should not be used to unauthorizedly change doctor's orders.
- The editors of MedElement are not responsible for any personal injury or property damage resulting from the use of this site.
Source: https://diseases.medelement.com/disease/%D0%B4%D1%80%D1%83%D0%B3%D0%B8%D0%B5-%D0%B1%D0%BE%D0% BB%D0%B5%D0%B7%D0%BD%D0%B8-%D1%8F%D0%B7%D1%8B%D0%BA%D0%B0-%D1%84%D0%B5%D1% 81%D1%82%D0%BE%D0%BD%D1%87%D0%B0%D1%82%D1%8B%D0%B9-%D1%8F%D0%B7%D1%8B%D0%BA -k14-8/13637
Vitamin deficiency
If there is a lack of vitamins B and D in the human body, the surface of the tongue dries out, cracks, becomes inflamed, becomes coated, and bad breath appears.
When an allergic reaction to vitamins occurs, the muscular organ swells, and dents from the teeth are clearly visible on its lateral surfaces. With a lack of vitamin B₃, the organ cracks, painful sensations appear, and a burning sensation occurs while eating. If an infection occurs, an acute inflammatory process develops, purulent ulcers form, and the person’s well-being worsens. To treat the disease, it is necessary to compensate for the lack of vitamins in the body.
Geographical language in adults - photo
See the next topic on our website: Kamistad - instructions for use. We will tell you in detail how and in what dosages to apply the gel to painful areas of the mouth of a child who has begun to teethe.Read about analogues of the Kamistad anesthetic gel here.
A clear clinical picture of desquamative glossitis allows a specialist to establish the correct diagnosis after a visual examination.
A number of laboratory examinations are carried out:
- Bacteriological culture of a smear taken from inflamed areas.
- PCR. Allows you to detect the presence of pathogenic flora by its DNA.
- Linked immunosorbent assay.
- A scraping for treponema to rule out syphilis infection.
- Cytological analysis.
- Analysis of stool to determine oviworms.
Basic principles of therapy
During therapy, the patient must adhere to some rules that will help speed up recovery.
These recommendations include:
- Thorough cleaning of the oral cavity, excluding damaged tongue tissue.
- Rinse your mouth with antiseptic solutions after each meal.
- Consumption of crushed foods.
- Refusal of hot, spicy and salty foods.
- Taking vitamin complexes.
Drug treatment
The drugs Furacilin, Miramistin and Chlorhexidine (0.05%) are suitable for treating the affected areas.
For painful symptoms, painkillers Lidocaine and Trimecaine are used. To prevent tissue atrophy, hydrocortisone ointment or Prednisolone in the form of a gel is prescribed.
Preparations containing vitamin C, for example, rosehip oil, can speed up the regeneration of damaged tissues. Vitamin A can be used for the same purpose.
Fibrin plaque that forms on the tongue during desquamative glossitis is removed with a cotton swab dipped in proteolytic enzymes or using applications. After cleaning the tongue, the oral cavity is treated with antiseptics.
Among the antibiotics prescribed for geographic tongue in adults, the following should be highlighted:
- Suprax. Dosage for adults: 400 mg per day. Duration of therapy is up to 10 days.
- Doxycycline. On the first day it is prescribed at a dosage of 200 mg. On other days, 100 mg per day.
- Tetracycline. Used for bacterial and fungal pathogens. For adults, the drug is prescribed at a dosage of 250 mg. Reception is carried out every 6 hours.
- Rocephin. Prescribed to adults for intravenous or intramuscular administration, 1-2 g per day.
Traditional medicine
Folk remedies can be used to combat the disease only after consultation with a dentist. Self-medication can make the situation worse.
After the doctor's permission, the following is carried out:
- Irrigation of the mouth with herbal solutions. To prepare the product, mix oak bark, chamomile, calendula and plantain leaves in equal proportions (10 g of each ingredient). The solution prepared from these plants has anti-inflammatory and regenerating properties.
- Rinsing your mouth with a soda solution. For this, 1 tsp. soda is dissolved in 1 glass of warm boiled water.
- Resorption of honey. The product is kept in the mouth until completely dissolved.
- Lubricating the tongue with propolis. The product has a strong wound healing effect.
- Taking a decoction of mint and eucalyptus. The drink is taken orally for severe pain on the surface of the tongue.
Folk remedies for desquamative glossitis are used to strengthen the immune system and restore damaged areas after the acute stage of the pathology.
For this purpose, tincture of echinacea or ginger and herbal tea (chamomile, lemon balm, St. John's wort) are taken internally.
Geographic tongue in adults is easily diagnosed by visual examination of the oral cavity. The examination is supplemented with a number of tests to identify the causative agent of the pathology. Only after determining the cause of desquamative glossitis can an effective treatment regimen be drawn up, including the use of antibacterial and antifungal agents, immunomodulators, enzyme preparations and folk remedies.
Hypothyroidism
This disease is caused by a malfunction of the thyroid gland. The pathology is manifested by swelling of the tongue with characteristic marks of teeth on its surface. Patients are inactive and find it difficult to talk due to dry mouth. There is a sensation of a foreign object in the mouth, the tongue becomes tangled.
External symptoms of the disease include a yellow tint to the skin, swelling of the face, increased hair loss, deterioration of memory and intellectual abilities, disruption of the digestive tract, and disorders of the genitourinary system. Hypothyroidism is treated by an endocrinologist.
Causes of a serrated tongue
A jagged tongue is not dangerous, and it is not a disease in itself, but a condition that is a consequence of other pathologies or diseases. The most common causes of a serrated tongue are:
Swollen tongue or macroglossia
“When your tongue swells, becomes too large for your mouth, puts pressure on your teeth and they leave their imprints on the sides of the tongue” [newsmax.com], edges become jagged .
A swollen tongue can be a consequence of allergies (in particular, angioedema), certain diseases and pathological processes: amyloidosis, hypothyroidism, tongue cancer, wounds and ulcers, scarlet fever, etc. Dehydration can also cause a swollen tongue and dry mouth.
Hypothyroidism
Thyroid hormone deficiency, which occurs due to underactive thyroid glands (hypothyroidism), can interfere with normal functioning of the body because “thyroid hormones regulate the way we use energy—metabolism—and without enough of these hormones, many body functions are significantly slowed down.” medicalnewstoday.com].
Additionally, if you produce little or no thyroid hormone, your face and tongue may become swollen. “When the face is severely swollen, swollen eyelids, thickened lips, and a swollen tongue may occur” [www.ito-hospital.jp]. And such a tongue is one of the reasons for the appearance of unevenness and jagged edges.
The most significant thyroid diseases for the appearance of a serrated tongue are Hashimoto's disease, thyroiditis and congenital hypothyroidism.
In addition to a jagged and swollen tongue, other symptoms develop with these pathologies:
- fatigue and general weakness;
- hoarseness of voice;
- hair thinning;
- dry skin;
- tendency to constipation;
- muscle pain;
- depression;
- increased sensitivity to cold, etc.
Therapy for serrated tongue for underactive thyroid includes:
- treatment of hypothyroidism using hormone replacement medications, which must be taken daily;
- eating foods rich in vitamin B;
- radiation therapy;
- psychological help for anxiety, stress, depression.
It is also possible to use non-traditional methods (acupuncture, naturopathic remedies and homeopathy, biofeedback (biofeedback), osteopathy) [womentowomen.com].
Temporomandibular joint syndrome
Tooth marks on the tongue
This is a pathological condition that occurs when the function of the temporomandibular joint, which connects the skull and lower jaw, is impaired. Occurs with injuries and significant constant sports loads, decreased bite height, and taking certain medications.
Main symptoms:
- teeth grinding (bruxism);
- headache;
- congestion, noise, ear pain;
- swelling of the sides of the face;
- painful chewing;
- clicking in the joint and subluxations.
In this situation, most people try to use the tongue to keep the jaw in a normal position. That is, if “the bite is incorrect, then to fix the jaw for swallowing ... the tongue presses on the teeth, stabilizing them” [mjtreatmentsc.com]. This can cause teeth marks and indentations on the tongue.
It's worth noting that if your tongue is not swollen, but has teeth marks, you may have a narrow lower jaw, or you have a habit of pressing your tongue too hard against your teeth.
Qi deficiency in the spleen
If your tongue is not only jagged, but also swollen and cracked, then according to Traditional Chinese Medicine, this indicates a lack of Qi (primary life energy) in the spleen. If this happens, the spleen is unable to perform its function in the digestive system, especially converting food into energy. And then the person begins to experience weakness and fatigue, pallor of the mucous membranes (including the tongue) and facial skin, poor appetite and weight loss in addition to a serrated tongue.
Sleep apnea
A possible cause of a jagged tongue is sleep apnea, which is “a common disorder in which one or more pauses in breathing occur during sleep, that is, brief stops in breathing” [nhlbi.nih.gov]. When there are pauses in breathing movements during sleep, the tongue often “sinks into the oral cavity,” and then its edges become uneven.
Bad habits
The development of certain habits, such as clenching the jaw or pressing the tongue tightly against adjacent teeth for a long time, can lead to uneven edges of the tongue. Anxiety can also cause people to press their tongue against their teeth because it causes increased muscle tension.
Deficiency of minerals and vitamins
Deficiency of folic acid and vitamin B12 causes excess production of abnormal red blood cells that do not function normally. This condition is known as megaloblastic anemia. This pathology can lead to swelling of the tongue. To solve this problem, you need to eat foods rich in vitamin B12 and folic acid, and also take medications containing these elements in doses and for a certain time prescribed by your doctor. In addition, iron deficiency can also cause changes. According to livestrong.com, "lack of iron can cause a swollen and jagged tongue... Meat, fish, poultry, fresh leafy greens, legumes and vitamin-fortified breakfast cereals can help meet your daily iron requirement" and prevent this phenomenon.
Painful cracks in the tongue
A tongue with jagged edges may also indicate the possibility of oral cancer, especially if there are painful cracks or sores. The likelihood of cancer is quite low, and it is usually accompanied by other symptoms.
Other reasons
A scalloped tongue that is pale or coated with a white coating may also indicate digestive problems or sinus disease.
Gastrointestinal diseases
The oral cavity and digestive organs are in direct communication. Diseases of the stomach and intestines cause acidity in the mouth, creating a convenient environment for the proliferation of bacteria. A persistent white or yellow bacterial coating appears on the surface of the tongue and mucous membranes, spots or erosions may form, the organ becomes inflamed and increases in size.
A symptom of the development of gastrointestinal diseases is the root of the tongue coated with plaque.
Peptic ulcers of the stomach, duodenum, duodenitis, dysbacteriosis, gastritis with high acidity, and colitis can cause such symptoms. Additionally, patients are bothered by abdominal pain, nausea, vomiting, heartburn, stool disorders, and flatulence.
To treat the pathology and eliminate plaque on the root of the tongue, you need to consult a gastroenterologist. During therapy, plaque and swelling disappear. If erosions have formed on the mucous membranes, it is necessary to do regular antiseptic mouth rinses with Chlorhexidine, Miramistin or Chlorophyllipt.
Why does a child's tongue peel off?
Many parents notice with alarm that the child’s tongue is undergoing changes - it suddenly changes its normal color, begins to peel and peel. Why do such changes occur, do they represent a serious pathology, and what treatment is required?
Geographic tongue, which is also known as desquamative glossitis, is a disease of an inflammatory-dystrophic nature, accompanied by external changes in the mucous surface of the tongue. This disease does not have any “age limits” - it can occur with equal frequency in adults and newborns. Most often, geographic tongue is diagnosed completely by accident, at a regular dentist appointment.
Nervous system diseases
With disorders of the nervous system, unpleasant painful sensations occur, tingling in the tongue, a disturbing feeling of dry mucous membranes, hyperesthesia, burning, disturbances of taste, diction, swelling and the appearance of bacterial plaque. This disease is called stomalgia, most often it affects women during menopause or after suffering shocks. Symptoms of the disease decrease with eating, especially when eating spicy foods. Unpleasant sensations are localized on the tip and sides of the swollen tongue, its edges are wavy, and dents from the teeth are visible.
The main causes of pathology are recently experienced tragic events in life: the death of relatives, cancer of loved ones, personal problems. Patients are easily excitable, constantly look at their tongue in the mirror, and are pathologically afraid of developing cancer.
Treatment of stomalgia is carried out comprehensively. It includes medication, psychotherapy, physiotherapy, acupuncture, and oral sanitation.
Uneven, wavy edges of the tongue may indicate the development of a serious illness. Therefore, if such a symptom appears, you should consult a dentist and therapist. Timely treatment will help avoid the development of severe complications.
Symptoms of geographic tongue
The main symptoms of desquamative glossitis are visible to the naked eye, so most often diagnosing the disease does not cause any particular difficulties.
In the vast majority of cases, geographic tongue refers to painless pathologies - the disease is not accompanied by any complaints or painful sensations. The appearance of the geographic tongue exactly corresponds to its name - whitish stripes, grooves and spots appear on the mucous surface of the tongue, which visually resemble a geographical map. The sizes of such spots can be very different - from several millimeters to centimeters. Most often, such lesions are multiple, and in extremely rare cases - single.
At the initial stages of the disease, the spots are small in size, but quickly begin to grow, merging with each other and creating larger spots.
The appearance of a geographic tongue in some cases may be accompanied by a feeling of discomfort, itching and tingling on the surface of the tongue, especially these unpleasant sensations intensify during meals. When eating too hot or cold, sour, spicy or salty foods, a person may experience disturbances in the sensitivity of the tongue, up to a complete loss of taste.
Is glossitis contagious?
It comes as a surprise to many people that the disease can actually be contagious. Here you need to understand that if glossitis of the tongue occurs due to non-infectious causes, for example, mechanical injuries and burns, then it is not contagious. If the cause of its development is infections, viruses and bacteria, for example, staphylococcus, streptococcus, herpes virus or candida fungi, then the pathology can become dangerous not only for you, but also for others and family members.
In addition, glossitis on the tongue may indicate that you have problems in the body, which again can be contagious to outsiders: diphtheria, helminthic infestations, tonsillitis, scarlet fever, syphilis.
Notice
: Undefined variable: post_id in
/home/c/ch75405/public_html/wp-content/themes/UltraSmile/single-item.php
on line
45 Notice
: Undefined variable: full in
/home/c/ch75405/public_html/wp-content /themes/UltraSmile/single-item.php
on line
46
Rate this article:
( 10 ratings, average: 4.90 out of 5)
language
- E.V. Borovsky, A.L., Mashkilleyson M. Diseases of the mucous membrane of the oral cavity and lips, 1984.
Consulting specialist
Dzagurova Elina Ruslanovna
Doctor rating: 9.5 out of 10 (2) Specialization: Dentist-therapist Experience: 10 years