Periodontal disease is a disease in which there are systemic lesions of the tissues around the tooth, that is, the periodontium. This disease also causes progressive damage to the dental cells (alveolar processes), sclerotic changes, the appearance of a fine-mesh pattern and a decrease in bone mass.
Periodontal disease refers to the last stage of damage to periodontal and gum tissues. Alveolar pyorrhea at the initial stage has no clinical manifestations and develops slowly. There are three stages during which different symptoms appear.
First stage of periodontal disease
At the first stage, degeneration of the alveolar processes is observed, which is accompanied by itching and burning in the gums, the appearance of persistent plaque, and increased sensitivity. There are no visible pathologies or inflammatory processes, but the teeth do not hurt or become loose.
The initial stage is also characterized by a burning sensation in the mucous membrane of the gums, which ceases to receive a normal supply of nutrients. This period is the most favorable for conservative treatment (not requiring surgical intervention).
Timely measures can minimize the consequences of the disease and prevent the transition to the second and third stages. At this stage, the teeth are firmly held, there are no gaps between them, and there is no exposure of the cervix. There is also no bleeding yet, but there is already tartar, which, even with regular professional cleaning, quickly accumulates again.
Unfortunately, the practically asymptomatic course causes the lack of early diagnosis. The disease occurs without itching and pain.
Consequences
The ongoing inflammatory process associated with soreness and inflammation of the gums contributes to the development of periodontitis, which results in the formation of so-called pockets between the teeth and gums, where numerous bacteria accumulate. If this condition is not stopped, deep infections occur, subsequently causing irreversible processes, including loss of bone tissue and teeth.
Ongoing chronic inflammation can put a strain on your immune system, and bacteria, entering the bloodstream through the gum tissue, have a negative impact on the functioning of the heart and lungs. The above conditions sometimes cause frequent respiratory diseases and rheumatoid arthritis.
Second stage of periodontal disease
At the second stage, degenerative processes are observed, provoking the release of pus in the gum pockets, the development of bleeding, and pronounced periodic gingivitis. A purulent process develops in the cavity of the pockets, the gum structure becomes loose, a whitish coating appears and the pericervical area is exposed. Gradually, tooth mobility and cracks in which food accumulates appear. There is pain when biting.
The middle stage indicates the development of periodontal disease, the roots are exposed by approximately 40-50%, interdental spaces and gum pockets are formed. Inflammatory processes periodically appear in the pockets with the release of pus.
Gingivitis
This is the first and reversible stage of periodontitis. Gingivitis is inflammation of the gums. This disease is very dangerous during pregnancy - due to changes in the hormonal levels of the pregnant woman, the disease progresses faster than usual, can lead not only to the loss of teeth in the pregnant woman herself, but also cause dental problems in the future in the child, and even provoke premature birth.
If you notice the following signs, then most likely these are symptoms of developing gingivitis:
- gum inflammation, bleeding,
- bright red gum color,
- pain and swelling in the gum area,
- bad breath, quickly forming plaque and stones.
The third stage of periodontal disease
This stage indicates the appearance of tangible atrophy of a total nature, the necks are greatly exposed and there is a strong displacement and instability of the tooth. The pain is constant and aching, abscesses are private, gum pockets become large and deep. In the absence of appropriate treatment, tooth loss occurs (the process spreads to the entire jaw), and osteomyelitis develops.
At the last stage, also called acute, serious deterioration of the condition is observed. Typically, patients consult a doctor precisely during this period, when pain, inflammation, and pus discharge appear. Severe exacerbation is possible during the dystrophic-inflammatory form, combined with the generalized form. Severe cavity abscesses are observed, and general intoxication due to purulent accumulations is possible. This period is characterized by a rapid course, the result of the acute stage is tooth loss.
Other forms of periodontal disease
In rare cases, neurodystrophic damage to pain receptors is observed, accompanied by the following phenomena:
- exposure of the neck and root of the tooth in the absence of inflammation or visible swelling;
- there is no acute pain, but there are wedge-shaped defects;
- tartar is observed (no plaque);
- there are no cavity pockets or their depth is small;
- The tooth stability is excellent, but only in the first two stages.
The chronic form is the most common; it is a long, sluggish process without pain or obvious symptoms. Often there are no signs at all, which subsequently causes complex treatment. In most cases, cure will require lifelong measures, otherwise the overall condition of the gums and teeth will deteriorate sharply. The result is a dystrophic process.
One more form stands out - neglected. The development time spans decades, the process is not accompanied by pain, inflammation, and there are no clinical symptoms. Signs of the stage are axial separation of teeth, large gaps, movement of individual teeth, ligament degeneration, and systemic dystrophy.
Treatment for this form is long, often very painful, and requires splinting. Measures are also needed to strengthen tissues and restore blood circulation in the periodontium.
How is it classified?
To draw up a treatment regimen, it is important to conduct a detailed diagnosis and determine the characteristics of the disease.
Periodontal disease occurs:
- localized - destruction of the tissues of one or several teeth;
- generalized - destructive processes affect the entire jaw.
This is a chronic, sluggish, progressive disease. The acute form is rare, since the pathology is not infectious. In the acute period, bleeding from the gums, pain, and discomfort during chewing are observed.
The progress of periodontal disease is divided into stages according to the degree of pathological changes in bone and soft tissue.
Causes of periodontal disease
The main reasons that lead to the appearance of periodontal disease:
- disruption of the endocrine system;
- bone tissue injuries;
- lack of vitamins, in particular vitamin C;
- problems with the gastrointestinal tract, cardiovascular system;
- smoking, alcohol abuse;
- hereditary factor;
- the presence of malocclusion (chronic injuries to the mucous membrane);
- taking anticonvulsants;
- the presence of chronic diseases, including diabetes mellitus, hypertension, dystrophic neurogenic processes, atherosclerosis, hypoxia;
- physical inactivity;
- impaired blood circulation in tissues;
- improper dental care.
The exact list of causes of periodontal disease has not been fully established. Much depends on heredity, the functioning of the cardiovascular and endocrine systems, and the presence of diseases of internal organs.
It is impossible to become infected with periodontal disease, since this disease is not caused by viruses or microbes. Bed linen, dishes, cutlery, and kisses cannot cause disease transmission. But personal hygiene should still be given maximum attention, since one of the reasons for the development of lesions is precisely damage to the mucous membrane of the gums and bone tissue.
Reasons for the development of the disease
It is difficult to identify what causes periodontal disease, since the pathology develops due to internal disorders in the body. Tissue atrophy often occurs due to oxygen starvation and lack of nutrients. External factors influence the disease indirectly.
Periodontal destruction occurs against the background of:
- hormonal disorders, disruptions during pregnancy, menopause, puberty in adolescents;
- low level of immunity for a long time;
- smoking, alcohol abuse;
- malocclusion;
- trauma to dental tissues (fracture, bruise), poor-quality prosthetics;
- diseases of the digestive system;
- unbalanced, poor nutrition, deficiency of vitamins and minerals;
- metabolic disorders, diabetes;
- long-term use of medications;
- insufficient oral hygiene;
- heredity, genetic predisposition;
- serious diseases: atherosclerosis, HIV infection, oncology, autoimmune pathologies and other diseases.
The answer to the question of whether periodontitis is contagious is obvious - it is not contagious. It is not associated with infection, and therefore the patient is absolutely safe for people.
Symptoms and signs of periodontal disease
There are no specific symptoms of periodontal disease, but there are signs that indicate problems have arisen and may indicate damage to the bone tissue of the tooth. But there are a number of basic symptoms that indicate the beginning of problems and the need to visit a doctor. Such signs include mobility and gaps between teeth, the appearance of bacterial plaque, periodontal pockets, pus, swelling and swelling of the gums. It should also be remembered that the oral cavity requires constant care, but if an unpleasant odor and the listed symptoms occur during regular cleaning, this indicates a developing disease.
Symptoms of periodontal disease include the following:
- the gums appear pale, and in the early stages there are no obvious inflammatory processes;
- Retraction of the gums appears, the neck is exposed, visually the length of the tooth seems longer;
- there is no bleeding in the early stages, but purulent pockets, enamel erosion, wedge-shaped defects and tooth abrasion may appear;
- At the same time, problems with the endocrine system, diseases of the cardiovascular system, and metabolic disorders can be diagnosed.
Main features
It is important to remember that at the initial stage there are no specific signs; alveolar pyorrhea often develops asymptomatically. Therefore, the first signs are already indicators of degenerative processes and require urgent intervention from a specialist. Pain, atypical plaque, softening of the gums - all this indicates the need to see a dentist and undergo examination with subsequent treatment.
The main signs of periodontal disease are:
- the appearance of atypical plaque in large quantities (this is not a specific sign, but already indicates the presence of problems);
- the appearance of tartar;
- discomfort when eating cold/hot, spicy food;
- itchy gums;
- the appearance of pulsation in the gum area;
- purulent discharge;
- bleeding in the gum area when chewing or other mechanical impact on their surface;
- the appearance of defects such as cavities, pockets or crevices in which food begins to accumulate;
- the gums begin to become covered with a whitish coating;
- teeth become weak, gaps appear between them, abrasion and other defects appear on the surface;
- the necks are exposed, the teeth visually appear longer;
- There is a phenomenon called retraction (destruction, resorption) of the gums.
Treatment of periodontitis
The disease requires urgent intervention by a dentist. Treatment of periodontitis includes non-surgical and surgical methods. The first (professional hygiene) is used in the early stages of the disease and for prevention. They consist of removing tartar (mechanically and ultrasound) and polishing the tooth surface, followed by treating the crown and root of the tooth with special brushes with fluoride-containing protective varnish.
There is a procedure for removing deep tartar called curettage: the doctor removes deposits using special hooks, excavators, curettes (closed curettage), or, if surgery is required, by cutting the gums (open curettage). The goal of surgical methods is to eliminate gum pockets (a consequence of bone tissue resorption) so that the tooth regains stability.
Diagnosis of periodontal disease
Diagnosis of periodontal disease begins with a visual examination, and the first signs of the problem are excessive formation of tartar with atypical exposure of the upper peri-cervical part of the teeth. It is recommended to go to the doctor for an emergency examination in the following cases:
- exposure of the neck or root of the teeth with the absence of severe inflammation;
- gum retraction;
- the presence of periodontal (gum) pockets;
- violation of the inclination of the teeth, the appearance of gaps;
- diagnosing metabolic disorders, problems with the endocrine or cardiovascular system.
Diagnostic methods
It is necessary to understand that a disease such as periodontal disease leads to extremely negative consequences. This is atrophy of the tissues of the mucous membrane of the gums and periodontium, the appearance of side diseases of the jaw, and loss of teeth. Therefore, it is necessary to consult a doctor regularly, and not only when the disease reaches an advanced stage. This will prevent the problem, diagnose periodontal disease at an early stage, start treatment in a timely manner and save teeth.
Diagnosis of periodontal disease includes the following measures:
- biochemical, general blood tests;
- assessment of the state of the immune system (an immunogram is prescribed);
- study of leukocyte vitality;
- Rotter's test to study the saturation of the body with vitamin C (deficiency of this substance is one of the causes of tooth loss);
- diagnostics of proteolysis activity, that is, the process of protein decomposition in the body into enzymes;
- microbiological methods;
- smears, impressions of the oral cavity (taken from the surface of the mucous membrane).
Typically, a diagnosis of periodontal disease is prescribed by a dental therapist after a visit. The patient is referred to a periodontist if there are signs of periodontal disease, the specialist performs a visual examination and further measures are prescribed. X-rays are often required to show the general condition of the teeth, see what form the tissues are in and how deep the lesions are. Treatment is prescribed based on the results of the study; its methods can be different, depending on the degree of damage to the teeth and gums.
Pathological anatomy
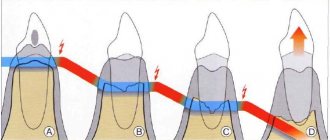
Rice.
1-3. Schematic representation of the formation of a periodontal pocket during periodontal disease (according to A. I. Evdokimov). Rice. 1. The relationship between tooth and periodontal tissue in a healthy person: 1—gingival groove (gap); 2 - interalveolar bone septum. Rice. 2. Initial stage of periodontal disease: 1 - periodontal pocket; 2—resorbable interalveolar bone septum; 3 - epithelium that has grown along the root of the tooth. Rice. 3. Severe stage of periodontal disease: 1 - periodontal and bone pocket formed as a result of resorption of the interalveolar bone septum; 2 - remains of the interalveolar bone septum. Periodontal disease usually begins with inflammation of the gums, occurring as chronic, catarrhal gingivitis (see). In the lumen of the gingival sulcus, abundant layers of loose basophilic masses are formed, including colonies of microbes and single epithelial cells. Later, on the basis of a dense supra- and subgingival plaque rich in microbial flora, tartar is formed (see), which aggravates the pathol, periodontal changes. Chronic gingivitis is accompanied by inflammatory infiltration of the gums with lymphoid, plasma cells, swelling of the gums, active proliferation, vegetation in the underlying connective tissue base of the gums, as well as increased desquamation of epithelial cells. The composition of the cellular infiltrate (lymphoid and plasma cells) is characteristic of a delayed-type hypersensitivity reaction. Already at this stage of the disease, mildly expressed lacunar resorption of the alveolar process bone is detected in the periodontal bone tissue (color fig. 1, 2).
The next stage of the pathological process is the formation of a periodontal pocket, characterized by the destruction of the epithelial cover in the area of the periodontal junction, the vegetation of epithelial layers deep into the periodontal gap. Electron microscopy, according to Carson and Sayegh (RE Carson, ES Sayegh, 1978), shows the disappearance of collagen fibrils of the periodontal ligament, which are normally woven into the cement. The contents of the periodontal pocket are necrotic detritus - structureless, basophilic and oxyphilic masses with colonies of microbes and destroyed leukocytes. The outer walls and bottom of the periodontal pocket are formed by granulation tissue, penetrated by branching layers of stratified squamous epithelium. In the bone structures of the alveolar process, pronounced resorptive changes are observed (tsvetn. Fig. 3), starting in the area of the apex of the alveolar process and leading to its complete resorption. Subsequently, resorbtin lacunae containing osteoclasts appear in the underlying sections of the walls of the dental alveoli, which leads to a gradual thinning of the interalveolar bone septa. At the same time, there is a thinning of the spongy bone in the thickness of the interalveolar septa. The resorption process can proceed as smooth resorption, lacunar resorption, and also as oncosis (as a result of bone cells acquiring the ability to osteoclase).
Against the background of patol, changes in the periodontium and as the periodontal pockets deepen in the adjacent areas of the periodontium, progression of hron and the inflammatory process is observed. Its morphological manifestations are the formation of dense lymphomacrophagic infiltrates with an admixture of plasma cells, the formation of fields of granulation tissue, and with exacerbation patol. process - solitary, and in some cases - multiple abscesses. With the progression of periodontal disease, periodontal pockets and the submersible growth of layers of stratified squamous epithelium, which are reactive in nature, reach the apexes of the roots of the teeth, and the periodontal ligament is completely destroyed. Further resorption of the bone tissue of the alveolar process leads to complete resorption of the interalveolar and interradicular bone septa (tsvetn. Fig. 3). With P., tooth tissue is involved in the pathological process quite early: cement resorption begins, which leads to the formation of deep cement and cemento-dentin niches. In parallel, the process of new formation of cement can be observed. If this process predominates, hypercementosis develops. In the pulp of teeth during P., dystrophic changes expressed to varying degrees are found, leading to its reticular atrophy, as well as to the formation of single and multiple petrificates and denticles in the pulp. Often with P., the development of retrograde pulpitis is noted, which can result in the death of the pulp.
Rice. 1. Histotopogram of the lower jaw with periodontal disease: 1 - teeth; 2 - Interalveolar bone septa with preserved contours of the apexes; 3 - areas of osteosclerosis; 4 - areas of osteoporosis; hematoxylin-eosin staining; x3. Rice. 2. Microspecimen of jaw bone tissue for periodontal disease: 1 - bone plates; 2 - artery with thickened walls and narrowed lumen; 3 — obliteration of the lumen of the vessel; hematoxylin-eosin staining; x 200.
Periodontal disease can occur with the predominant development of dystrophic changes in the periodontal tissues with characteristic atrophy of the bone trabeculae of the spongy substance, pronounced focal osteosclerosis, alternating with focal osteoporosis (Fig. 1). Patol, changes in bone tissue are combined with pronounced changes in its blood vessels: hyperplasia of the inner membrane, sclerosis and hyalinosis of the middle membrane, sharp narrowing or complete obliteration of the lumen of the vessels (Fig. 2).
In the connective tissue base of the gums, pronounced changes in blood vessels are also observed, manifested by proliferation of the endothelium, the formation of parietal thrombi, and sometimes the development of vasculitis; Against this background, swelling of collagen fibers, their fragmentation and even lysis are quite often observed. In general, the condition of the gums is characterized by the development of a sluggish inflammatory process in it; in the connective tissue stroma of the gums, an infiltrate of plasma and lymphoid cells is found, localized mainly in the area of the gingival sulcus.
Morfol, changes in the periodontium, similar to those with P. in humans, were obtained in experiments on animals.
Treatment and prevention of periodontal disease
Treatment of periodontal disease is a long process that requires the patient to strictly adhere to the recommendations and prescriptions of the doctor. Measures to get rid of periodontal disease can be different, it all depends on the stage and how far the damage to the gums and dental tissues has progressed.
The following methods are used in treatment:
- physiotherapy;
- surgical treatment (curettage of periodontal pockets);
- splinting (for loose teeth)
- anti-inflammatory treatment;
- preventive measures (aimed at preventing the development of periodontal disease and its more complex stages, and are also used to normalize the condition of dental tissue).
The main set of measures is aimed at restoring and improving gum blood flow, reducing pain, and inflammation of periodontal tissue. Correct and timely treatment restores the normal supply of tissues with oxygen and nutrients, and allows you to stimulate the formation of new cells.
Physiotherapy
Physiotherapeutic treatment includes:
- ultrasonic treatment of the oral cavity;
- electrophoresis;
- KUF therapy.
Such treatment methods help improve the blood supply to the gum tissue and the general condition of the periodontium.
Prevention of periodontal disease
Prevention of a disease such as periodontal disease should include a whole range of measures, including eating healthy, fortified foods, regular oral care, and visiting the dentist. You need to start with regular intake of microelements. You should first consult with a supervising physician, who can correctly assess the degree of mineral deficiency and advise taking supplements or following a diet. Such prevention will allow you to saturate the body with essential microelements and quickly restore tissue.
In addition, patients with periodontal disease should regularly visit their doctor and maintain oral hygiene:
- Teeth should be brushed twice a day, recommended after each meal;
- To clean the interdental space, you need to use a special dental floss;
- follow a special balanced diet;
- after eating, rinse with special antiseptic rinses;
- use toothpastes with an anti-inflammatory effect.
Periodontal disease also requires regular professional tartar removal, performed by a supervising physician. In this case, tartar will not have time to accumulate in a large volume, the gums will not be injured, which will speed up the cure of the disease and prevent the development of such a dangerous disease as periodontal disease.
What can a doctor do?
Only the dentist and hygienist with a simple examination
can determine the presence or absence of periodontal disease. The essence of the study is to measure the periodontal pocket (for periodontitis) using a special probe and an x-ray. This method allows the doctor to quickly and painlessly assess the condition of your gums, propose a treatment plan to prevent further development of the disease, and develop a special self-hygiene regimen that will suit your specific situation.