What is periodontitis in adults, what are the symptoms, treatment? The disease begins with gingivitis (inflammation of the tissue around the tooth) and does not progress to a more severe form if quality therapy is started in time. At the very beginning of the disease, it is permissible to use folk remedies, but any manipulations and procedures should be discussed with the attending physician.
The pathology is curable, but it is much easier to adhere to preventive measures and prevent its occurrence. Maintaining hygiene is the key to health not only of the oral cavity, but also of various organs and systems.
What is periodontitis
The tissue surrounding the tooth is called periodontium. This includes the gums, root part, socket and dentogingival ligaments. The tasks that these elements perform:
- reliable fixation of dental units in a certain place;
- uniform distribution of chewing load;
- control of muscle fibers.
When the functioning of these structures is disrupted under the influence of certain factors, an inflammatory process occurs and the alveolar processes are destroyed. In the absence of timely medical intervention, incisors, canines and molars become mobile and subsequently fall out, purulent discharge and an abscess are observed.
Pathology is often diagnosed against the background of chronic diseases. Patients with diabetes mellitus, hypothyroidism, gastric ulcer, and heart failure are at risk.
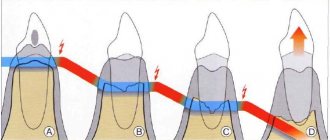
Development of periodontitis
Problems begin from the very moment when a person stops taking care of the oral cavity, and a large amount of persistent plaque accumulates on the enamel. Rotting food particles and a moist, warm environment contribute to the active proliferation of pathogenic bacterial flora. As a result, acids and other aggressive substances are produced, which corrode the crowns and deeper layers, and soft tissues become inflamed.
Gingivitis appears and the gums begin to bleed. If this process is not stopped in time, periodontal pockets form and the infection penetrates to the roots. There is severe sensitivity when consuming hot or cold foods or drinks. Then the rows become loose and individual units fall out completely or partially.
Statistics
This is one of the most common dental diseases in the world. It is second only to caries. According to statistics provided by the World Health Organization, the pathological process occurs in more than 94% of the world's inhabitants.
Periodontitis - ICD
According to the International Classification of Diseases, Tenth Revision, pathology has codes K05.2 (acute form) and K05.3 (chronic).
Why you can’t install removable and bridge dentures against the background of advanced periodontitis
Loss of bone tissue and widening of the sockets during periodontitis create a very ambiguous situation: on the one hand, long-term conservative treatment in the later stages is rarely effective, on the other hand, prosthetics are also difficult, and the problem of missing teeth needs to be solved. However, not every treatment method is suitable.
Why are dental bridges not suitable?
Teeth with periodontitis are weakened and are on the verge of falling out; it is strictly forbidden to use them as support for a denture. The bridge will be movable along with the teeth on which it is attached. The risks are high, even if complex and long-term treatment was carried out before.
Why are removable dentures not suitable?
In fact, after a course of treatment for periodontitis (or closer to the middle of it after acute inflammation has resolved), removable dentures can be installed to solve the problem of partial absence of teeth. But only for a short time, because... When used long-term, they lead to many problems:
- do not stop bone atrophy, but only aggravate this process,
- put increased pressure on the gums and can provoke inflammation, which is extremely undesirable during the course of therapy,
- will require regular correction, since during treatment the damaged tissues are restored, which means the level of the bone with the gum will change - the dentures will no longer fit tightly, will shift, dangle,
- if teeth are partially missing, there is nothing to attach them to - as in the case of bridges, it is better not to use living teeth for support, especially if they are mobile,
- if the teeth are removed scatteredly, then removable dentures will not work at all; the minimum segment is 2-3 missing teeth in a row.
That is, removable dentures can provoke the development of periodontitis and negate all the results of a course of complex treatment. In addition, they are difficult to get used to - more than half of patients are not satisfied with them either in aesthetics or functionality.
Symptoms
The clinical picture is determined even at the earliest stages. Signs of the disease depend on its location, type and severity. Let's consider what phenomena can be used to suspect the presence of periodontal problems.
Main symptoms
In most cases there is:
- bleeding gums (gingivitis);
- bad breath;
- compaction and change in the shade of soft tissues;
- increase in interdental spaces;
- the appearance of dense plaque and stone;
- formation of periodontal pockets;
- loosening of teeth;
- increased sensitivity when eating hot and cold, sweets;
- discomfort while chewing food;
- extraneous gingival discharge;
- tooth loss;
- cyanosis of the mucous membranes.
If any of the above manifestations are detected, you should immediately contact your dentist. With timely medical intervention, there is a possibility that the disease will go away after using traditional methods of therapy.
Additional symptoms
Also in more rare cases you may notice:
- increased saliva viscosity;
- fistulas or abscesses;
- sensation of pulsation in the gums;
- swelling and inflammation of the mandibular lymph nodes, pain (especially when pressed);
- headache, migraine.
Causes of periodontitis
There are several factors contributing to the development of pathology. The most common is considered to be poor-quality oral hygiene care. Infectious agents (mainly streptococcus or staphylococcus bacteria) actively multiply, the products of their metabolic activity and decay penetrate into deep tissues, causing irritation and severe inflammation.
The following can also lead to the disease:
- malocclusions and defects of the dental system;
- increased tone of the masticatory muscles;
- violation of the integrity of the mucous membranes;
- insufficient blood supply to the gums;
- deficiency of vitamins and minerals;
- physical injury to incisors, canines or molars due to impact or fall;
- accumulation of large amounts of plaque and tartar;
- bad habits (smoking, alcohol abuse);
- chronic pathologies of the urinary system;
- Alzheimer's disease;
- stressful situations, experiences;
- imbalance of hormones in the body;
- weakening of the immune system.
Development
There are several stages of periodontitis, each of which is characterized by special symptoms and signs.
With the flow
Division according to one of the criteria.
- Spicy. It affects 1-2 teeth and is accompanied by pronounced symptoms. A sharp pain appears, the mucous membranes swell and bleed.
- Chronic. A sluggish, long-term process has periods of exacerbation and remission.
By localization
- Localized. Develops against the background of injuries and other local factors.
- Generalized. The periodontal tissues of the entire jaw or only the right (left) side are involved.
By severity
- Easy. The teeth are immobile, the gums are bleeding.
- Average. Periodontal pockets up to 0.5 mm in depth are formed.
- Heavy. The destruction is noticeable to the naked eye, there is plaque, stone, incisors, fangs or molars wobble and fall out.
Diagnostics
Knowing the causes of periodontitis and the main symptoms of the disease, it is necessary to confirm its presence and determine the stage of the pathological process. Doctors use the following methods in their work:
- studying the patient's medical history;
- visual examination of the oral cavity;
- determination of the bleeding index;
- radiography;
- laboratory tests (general blood and urine tests);
- rheoparodontography;
- use of a periodontal indicator.
Treatment
Pharmacy chains offer many effective drugs to suppress the pathological process. There are also separate recommendations, the observance of which will help speed up recovery. The patient should not self-medicate. It is important to first consult with a dentist and develop a therapeutic regimen depending on the severity of the disease.
Local drug treatment of periodontitis
If there is increased pain and worsening infection in the mouth, doctors often prescribe antibiotics. For example, Amoxicillin, Tsiprolet, Lincomycin, etc. are used.
The exact dosage must be calculated by the dentist. Additionally, the use of probiotics to restore normal microflora (Linex, Lactobacterin) is indicated.
Ointments and gels
Products for external application are quickly absorbed by soft tissues and kill pathogenic microorganisms. This eliminates not only the cause of the pathology, but also accelerates the regeneration of damaged fibers.
Preparations containing lidocaine are most often prescribed. For this reason, you need to contact a dental clinic in advance to exclude possible allergies due to intolerance to the components. The most popular means:
- Kamistad.
- Solcoseryl.
- Holisal.
- Metrogil Denta et al.
Rinse aids
Liquid formulations help fight bacteria, relieve inflammation and promote rapid healing of wounds. At the same time, the enamel becomes lighter and cleaner, and your breath becomes fresher. On store shelves you can find solutions such as Lakalut, Splat, Parodontax.
Vitamins
During therapy, it is necessary to take vitamin complexes. To quickly heal wounds, normalize metabolic processes and strengthen the immune system, various additives are used in the form of applications to pathological areas.
Professional oral hygiene
This is the main guarantee of healthy teeth and gums. If plaque or tartar has accumulated, it is recommended to contact your dentist. Some useful skincare tips:
- clean in the morning and evening;
- flossing throughout the day;
- use of an irrigator;
- rinsing with special rinses after meals;
- regular massage.
Diet
The menu should include a lot of fresh fruits and vegetables. The most suitable are apples, pears, carrots, bell peppers, cucumbers, berries, citrus fruits, and nuts. To keep your enamel strong, you need to eat more cheese, cottage cheese, beans, dried apricots and other foods high in calcium.
You need to give up fried foods, smoked foods, and too spicy foods. The problem is also aggravated when drinking hot drinks.
Surgery
If the patient knows firsthand what oral periodontitis is and suffers painful symptoms, surgical intervention is indicated. Doctors resort to similar methods when dental units are very loose. Popular methods: splinting, patchwork, open and closed curettage.
Plasmolifting
This is the most effective method after surgery. The procedure for introducing plasma into the gums helps improve tissue regeneration, fights inflammation, and reduces bleeding.
Orthopedic structures
If there are no incisors, canines or molars, dentures are installed. You cannot do without prosthetics, otherwise malocclusion may appear and further progression of the disease.
Physiotherapy
Physiotherapeutic methods show effectiveness as part of complex therapy in combination with pharmaceutical drugs and surgery. After a course of procedures, blood circulation and metabolic processes improve, periodontal tissue is strengthened and restored. In most cases, dentists prescribe:
- ultrasound;
- balneotherapy;
- light therapy;
- electrophoresis;
- darsonvalization, etc.
WHAT IS MEAN BY PERIODONTAL TREATMENT
After collecting all the necessary information, the periodontist will discuss the condition of your gums with you and suggest the most optimal treatment. Most importantly, it must be comprehensive - that is, treatment must cover all identified causes and associated factors that support the disease. Only in this case can it be possible to completely cure or stabilize periodontal disease for a long time.
Treatment will be much more effective if the patient strictly follows all instructions and strictly follows the chosen treatment plan.
Typically, a comprehensive treatment plan consists of general and local treatment and includes all or part of the methods listed below.
Treatment with folk remedies
The use of home recipes is advisable if periodontitis is in the initial stages and is not accompanied by various complications. In severe forms, such techniques are also acceptable as part of complex therapy along with antibiotics, anti-inflammatory drugs, sedatives and immunomodulators. More often, herbal decoctions and infusions, natural juice, and extracts are used for this. Patients, as directed by the dentist, also make lotions, baths, and rinse the mouth.
Hydrogen peroxide and soda
The most affordable and common option. The substances are used for wiping gums, rinsing and brushing. You should mix the ingredients until you get a paste, and then brush your teeth well. But you should not do this without advice from a specialist.
Oak bark decoction
1 tbsp. dry raw materials are poured with a glass of boiling water. After leaving for half an hour, you can rinse your mouth or take a bath. Eating is allowed only after an hour.
Salt treatment
There are several ways to use this available remedy in therapy:
- rinsing with a concentrated water-salt solution (1 tablespoon of dry substance per glass of warm liquid);
- applications;
- oral baths.
Honey and propolis
If you chew bee glue several times during the day, it will penetrate into the interdental spaces and periodontal pockets, which will have a beneficial effect on the condition of the mucous membranes.
No less effective is honey tincture made with alcohol or vodka. The solution is infused for about two weeks, the container is shaken regularly.
Fir oil
You can use sea buckthorn, it works on the same principle. The substance is used in applications during gum massage.
Rose petals
The alcohol infusion is rich in such valuable elements as zinc, phosphorus, and manganese. If you dilute 30 drops in ½ glass of water, you can rinse your mouth. The procedure is carried out 2-3 times a day.
Garlic
You need to mix 1 tsp. crushed product and black tea, pour 1 tbsp. boiling water After leaving for half an hour, the product is ready for rinsing. Causes burning of mucous membranes.
Beetroot pulp
You need to chop a medium root vegetable, squeeze out the juice and place the dry raw material in cheesecloth in one layer. It is worth applying beets to the affected area for 15-20 minutes every 4-6 hours.
Saffron lotions
1 tsp dry matter is combined with a small amount of vegetable oil. The paste wrapped in gauze is kept on the inflamed mucous membranes up to 3 times a day for 20 minutes.
Medical Internet conferences
Review of modern methods of treatment of generalized aggressive periodontitis
Shcherbakova T.A. – 4th year, Faculty of Dentistry
Scientific supervisors – associate, Ph.D. Petrova A.P., ass. Venatovskaya N.V.
FSBEI HE "Saratov State Medical University named after. IN AND. Razumovsky" of the Ministry of Health of the Russian Federation
Department of Pediatric Dentistry and Orthodontics
Summary. This article discusses modern methods of treatment (conservative and surgical) for generalized aggressive periodontitis (GAgP) in the clinical practice of a dentist.
Key words: generalized aggressive periodontitis, periodontal diseases.
Responsible author: Shcherbakova Tatyana Alekseevna,
Modern methods of treatment of generalized aggressive periodontitis
Shcherbakova TA – student of the 4th course of dental faculty
Razumovsky Saratov State Medical University
Pediatric Dentistry and Orthodontics department
Summary. This article describes the modern methods of treatment (conservative and surgical) generalized aggressive periodontitis in clinical practice dentist.
Keywords: generalized aggressive periodontitis, dental, periodontal disease.
Relevance. Aggressive periodontitis is a type of periodontal disease characterized by fulminant destruction of the periodontal ligament and loss of alveolar bone mass, which usually occurs in young people, less often in patients of older age groups [1]. According to the classification of periodontal diseases, adopted at a meeting of the presidium of the periodontology section of the Russian Dental Association in 2001, this disease was included in an independent group of periodontal diseases - aggressive forms of periodontitis. However, practicing dentists more often turn to the ICD-C-3 classification of dental diseases based on ICD-10 (WHO, 1995), according to which aggressive periodontitis corresponds to code K 05.4 “Periodontal disease”. Based on research conducted by the Department of Periodontology, Wonkwang University School of Dentistry, Iksan, Korea, the incidence of aggressive periodontitis in a study population of 1,692 patients (1,020 men (60.3%) and 672 women (39.7%) was 28 cases (1.65%) There were no significant differences between the percentage of male and female patients. The generalized form was more common than the localized form in a ratio of 27:1. The mean age was 34.5 years [2]. Even so that the prevalence of aggressive periodontitis is significantly lower than other periodontal diseases, such an immutable risk factor as a strong genetic predisposition causes significant difficulties in the process of its treatment. The lack of early diagnosis and timely treatment in patients with this disease in a short time can lead to rapid destruction of periodontal tissue and tooth loss [3].There are specific diagnostic signs, but their clinical manifestations may vary between patients. If the disease is diagnosed in advanced stages, successful treatment is challenging. There is a wide variety of treatment options available today, with fairly variable success rates. However, research in this area is growing at an exponential rate and treatment options such as tissue engineering and genetic technologies are promising for this disease.
Purpose: to find out the feasibility of various methods of treatment of generalized aggressive periodontitis (GAgP) according to literature sources.
Tasks:
1. Characterize the main clinical signs of generalized aggressive periodontitis.
2. Consider the basic principles of treatment of the pathology being studied.
3. Find out the effectiveness of non-surgical treatment for GAgP
Materials and methods. An analysis of scientific articles in Russian and English was carried out, a review of modern educational publications on the topic of types of periodontal diseases and methods of their treatment was carried out.
Results and discussion. When faced with this pathology in clinical practice, it is necessary to take into account that generalized aggressive periodontitis is a multifactorial disease in which microbiological, genetic, immunological and behavioral factors are integrated. They determine the onset, course and severity of the disease. The presence of bad habits, such as smoking, or an unsatisfactory level of oral hygiene in patients causes more massive periodontal destruction compared to those who maintain a satisfactory level of oral health.
The disease has a wave-like course with periods of exacerbation and remission. This causes the presence of two different clinical pictures during the examination. During the period of remission, patients do not present any complaints, the gums are pink, but probing reveals deep periodontal pockets. The absence of visible signs of an inflammatory reaction, despite the presence of deep periodontal pockets and disruption of the tooth-gingival junction, together with the complete physical health and young age of the patients, is a characteristic feature of aggressive periodontitis, which is detected at this stage of the disease. Periods of remission can last from several weeks to several months or years, accompanied by periods of exacerbation of the disease. During the acute phase, progressive destruction of the alveolar bone and loss of the periodontal junction occurs. At this stage, during a clinical medical examination, the gums have all the signs of inflammation from mild to severe. Inflammatory gum hypertrophy is common. When probing with a calibration probe, bleeding is typical in six areas around each tooth or even spontaneous release of purulent exudate. Most patients consult a dentist at this stage of the disease.
The prognosis of treatment largely depends on a timely diagnosis. Early diagnosis of the disease helps prevent its progression and avoid serious loss of alveolar bone mass. In addition, since aggressive periodontitis tends to run in families, it is necessary to screen close relatives for early diagnosis of the disease in other family members [4].
Conservative treatment remains the primary method of antibacterial therapy for generalized aggressive periodontitis . In the initial stages of the disease, when the destruction of the periodontal joint and bone is mild to moderate in severity, treatment of the disease is based on the use of systemic antibiotics in combination with mechanical therapy. Treatment should begin with an attempt at complete elimination or bacteriostatic action on etiological factors and modifiable risk factors. It should be borne in mind that the disease has a strong genetic predisposition. The response of the human body to pathogenic microorganisms in dental plaque plays a significant role in its pathogenesis and expression. This response is determined genetically and is an unchangeable risk factor for the pathology in question [5]. However, the disease is also dependent on microbial and environmental factors, and can therefore be successfully controlled in susceptible individuals, indicating the absolute importance of timely removal of dental plaque at home by the patient or the doctor at a dental appointment. In patients susceptible to the disease, even a small amount of dental plaque can provoke a humoral and cellular immune response. Mechanical removal of plaque from the tooth surface can be achieved by teaching and motivating the patient in proper oral hygiene through a visual demonstration on a mock-up of teeth brushing using the modified Bass method (for patients without gum recession) and the modified Stillman method (for patients with hyperesthesia). Also, the use of auxiliary cleaning hygiene items for interdental spaces (floss, interdental brushes, brushes) will ensure effective treatment of the most inaccessible areas of the oral cavity. Regular visits to the dentist to monitor the effectiveness of plaque control are important. For further control, oral rinsing with 0.12% or 0.2% chlorhexidine or 1% povidone iodide may be recommended as an addition to mechanical measures [6]. Aminofluoride and tin fluoride in rinses and toothpastes are also effective in combating supragingival plaques in aggressive periodontitis. In addition, the use of fluoride as a mouth rinse is recommended for remineralization of exposed root surfaces, and also as a desensitizing agent in patients with complaints of dental hypersensitivity [7]. It has been scientifically proven that smoking is a significant risk factor and leads to a more severe course of the disease. The effectiveness of conservative and surgical treatment and regenerative therapy in such individuals is significantly less than in non-smoking patients. Therefore, the doctor at the dental appointment should inform about the effect of smoking on the periodontal condition and the benefits of quitting it [8].
One of the options for conservative mechanical antimicrobial therapy is Scaling & Root Planing (SRP) - a method of instrumental removal of supra/subgingival dental plaque and tartar, leveling the surface of the tooth root, used by clinicians as etiotropic therapy for periodontitis. For this purpose, it is possible to use manual instruments, mainly curettes and scalers, as well as air abrasive systems and fine-grained diamond burs. Scaling and Root Planning are carried out sequentially in one visit. After the intervention, the surface of the crown and root should be hard, clean and free of micro-roughness. SRP is one of the most commonly used bacterial reduction procedures and is considered by many physicians to be the gold standard of treatment [9]. However, this method does not ensure the complete destruction of pathogenic microorganisms and their metabolic products from periodontal pockets. There is a pattern: the deeper the periodontal pocket is revealed during probing, the lower the effectiveness of SRP [10]. An alternative to mechanical antimicrobial therapy was proposed by Quirynen and represents a single-phase disinfection of the entire oral cavity. This method leads to a significant improvement in the clinical situation of the initial stages of periodontitis, compared with the isolated use of SRP. It involves complete sanitization of the oral cavity, carried out by brushing the tongue with a 1% chlorhexidine solution for 1 minute, removing dental plaque, rinsing the mouth with a 0.2% chlorhexidine solution for 2 minutes, as well as irrigating periodontal pockets with a 1% chlorhexidine solution . Careful precautions are necessary, since high concentrations of chlorhexidine in sensitized patients can cause an individual reaction in the form of contact dermatitis, itching and urticaria. The effect of topical use of chlorhexidine during pregnancy and lactation has not been studied, so the antiseptic should be used only in extreme cases. The effect of the drug in pediatric practice has also not been studied; therefore, it is not recommended for use in children under 18 years of age. In general, the treatment modality is selected based on the specific clinical situation and patient preferences [11].
Photodynamic therapy and laser irradiation are additional methods to the main therapy for inhibiting pathogenic bacteria in periodontal pockets [12]. An effective and atraumatic method of treatment is the use of lasers, since they have bactericidal and detoxifying effects. This is due to a number of factors: improvement of regional blood flow in the area of the pathological focus, increased chemotaxis of leukocytes to the area of inflammation and activation of proteolytic enzymes, which have a detrimental effect on microbes. The most widely used are helium-neon gas and gallium arsenide semiconductor lasers. The light they emit is effectively absorbed by the cells of the mucous membranes and has a greater depth of penetration into the tissue. Laser devices of the AL-010 and SOFT-LASER series are convenient to use [13, 31].
Photodynamic therapy (PDT) is also a non-invasive infection control approach that combines laser energy with a photosensitizer to produce singlet oxygen molecules and free radicals that are effective in killing bacterial cells. PDT has high clinical success rates and a number of advantages such as: reduction of treatment time for subgingival areas, destruction of microorganisms within a short period of time, absence of the need for anesthesia and damage to adjacent tissues, as well as the development of resistant forms of bacteria [14]. In recent years, these modern methods have shown themselves to be a promising direction, popular among doctors, as a non-surgical treatment for generalized aggressive periodontitis. The combined use of SRP, PDT and laser irradiation shows greater clinical effectiveness compared to monotherapy. During the initial stages of treatment, regular visits to the dentist can assess the patient's response to non-surgical therapy [15].
Systemic antibiotic therapy. The use of systemic antibiotics is an integral part of the treatment of aggressive periodontitis, since pathogenic bacteria, such as Aggregatibacter actinomycetem-comitans and Porphyromonas gingivalis, cannot be completely destroyed using other methods [16]. Previously, tetracycline antibiotics were widely used to achieve this goal. They have the ability to concentrate in periodontal tissues and inhibit the growth of A. actinomycetem-comitans. In addition, tetracyclines inhibit collagenase, reducing tissue destruction and facilitating bone regeneration [17]. But the development of resistance to them has led to the use of other pharmacological groups as combination or sequential therapy. The current preferred combination is amoxicillin 250 mg three times daily with metronidazole 250 mg twice daily for 8 days. This is one of the most effective combinations of drugs, which has enough evidence for this [18]. With therapeutic treatment in the initial stages of the disease, antibiotic therapy significantly improves overall treatment results. Identification of the species of bacteria and their sensitivity to antibiotics is not mandatory, since the combinations described above may be clinically and economically more beneficial. The use of only one drug (doxycycline, azithromycin, metronidazole and clindamycin) produces results when used in addition to SRP. The choice of antibiotic is made based on numerous criteria - possible allergic reactions on the part of the patient, concomitant pathologies, medical history [19].
Topical antimicrobial agents are also a necessary component of the therapeutic treatment of aggressive periodontitis, especially if there is limited accumulation of exudate, deep periodontal pockets and lack of adequate response to mechanical therapy and the use of systemic antibiotics. The main advantage of using this method is the delivery of smaller doses of drugs to the periodontal pocket, while the concentration of the active substance at the site of infection is maintained at a high level. This avoids side effects typical of systemic antibacterial agents.
In addition, this option is applicable in case of intolerance to systemic administration of drugs. Recently, drugs with gradual and slow release of the active ingredient have been used. The decision to use topical anti-infective adjunctive therapy remains a matter of individual clinical judgment, treatment phase, and patient status and choice [20].
A review of the literature and scientific research on the topic of non-surgical treatment of generalized aggressive periodontitis showed that this pathology can be successfully treated with therapeutic methods. Since such treatment leads to the cessation of disease progression, resolution of inflammation, reduction in the depth of periodontal pockets, and significant reconstruction of alveolar defects. Based on these data, the treatment plan should begin with primary or additional mechanical antimicrobial therapy in combination with systemic antibiotics. It is recommended that antibiotic therapy be started 24 hours before SRP or other mechanical plaque removal methods and continued concurrently with these procedures. After 4-6 weeks, the patient's oral health is re-evaluated. If there are no significant changes in the initial stages of therapy, the doctor may repeat the treatment using different combinations of antibiotics and possible treatments. If there is no effect, you should proceed to surgical treatment [21].
Surgical treatment of generalized aggressive periodontitis is a set of measures aimed at preventing further tissue damage and bone loss in the event of late diagnosis or ineffective therapeutic intervention. In order to minimize undesirable consequences, it is possible to use alternative laser surgery. With extensive loss of periodontal tissue, surgical treatment can lead to increased tooth mobility and a worsening of the clinical situation as a whole. Therefore, a careful assessment of risk factors and benefits for a specific individual situation is necessary [22]. Currently, restorative surgical treatment is based on the regeneration of the anatomical form and function of the periodontium. Replacement bone grafts, guided tissue regeneration (GTR) and biological modifiers (growth and differentiation factors, extracellular matrix proteins) are widely used.
In order to eliminate pathological pockets, it is rational to perform flap operations on soft tissues. The repositioned flap (modified Widmann flap) and the technique of tilting the flap while preserving the gingival papilla are the methods of choice in the practice of the dentist. The combination of surgical treatment with the use of systemic antibiotics leads to a more intensive reduction in microbial load and pocket depth.
Bone destruction, which occurs quickly in aggressive periodontitis, is a particular problem and requires immediate attention from a physician. There are two methods with the most successful treatment outcomes: bone transplantation and guided tissue regeneration. The dental materials market represents a wide range of transplantation materials, including autografts, allografts, xenoimplants and alloplasties. In the process of autotransplantation, material obtained from one anatomical site is transplanted to another within the same organism. Autogenous transplants are considered the standard and have excellent regenerative properties, which have been scientifically proven by histological examination. Additional benefits include eliminating the risk of spreading the disease, eliminating the immune response, and reducing the cost of surgery. The main limitations associated with the use of autografts in periodontal regeneration are the limited amount of bone tissue that can be transferred, coupled with a high risk of developing pathological processes at the donor site [23]. Currently, advances in the field of tissue engineering and biomaterials technology provide a large number of options for the treatment of bone defects, so doctors are striving to use alloimplants, xenoimplants and alloplastic bone substitutes in their practice. The transplantation of bone tissue between two genetically different organisms is called alloimplantation. Bone allografts are unique in that they typically have the cellular component removed to reduce the risk of rejection. In addition, they are carefully processed to eliminate any possibility of disease transmission. Clinical studies confirm the favorable outcome of treatment using these materials. In terms of filling intraosseous defects, more than 50% of them are completely resolved [24]. The use of animal-derived materials for human tissue repair relies on the use of either bovine or coral material. These types of implants are called xenoimplants. The combination of bovine material with purified porcine collagen or synthetic polypeptide (PepGen P-15) stimulates regeneration and leads to the formation of a healthy periodontal ligament. Due to the low allergenicity and biodegradation of collagen, it has good tissue compatibility. Collagen preparations reduce inflammatory reactions and shorten wound healing time [25]. Synthetic bone substitutes include osteoconductive polymers in the form of blocks, granules, cements, or osteoinductive proteins. Proteins stimulate osteogenesis, cementogenesis and periodontal ligament growth, and osteoconductors provide a passive matrix for new bone. Hydroxyapatite, beta-tricalcium phosphate, and bioactive glass are the most commonly used alloplastic materials [24].
The principle of directed tissue regeneration is based on the use of membranes that prevent the migration of gingival epithelium and the growth of granulation tissue, which allows specific poorly differentiated cells of the periodontal ligament to form a new connective tissue attachment. The membrane can be produced from biological preparations or from the patient’s blood. One of the most commonly used is a membrane made of stretched polytetrafluoroethylene. Many experimental and clinical studies have proven the effectiveness of using membrane technology in conjunction with planting materials. This method is being actively improved, membrane production technologies are being improved, but today guaranteed efficiency can only be found in the case of 3-wall defects [26].
The use of biological mediators (insulin-like growth factor, platelet-derived growth factor, platelet-rich plasma) and extracellular proteins leads to improved clinical and radiological parameters. Platelet-rich plasma promotes the restoration of lost periodontal tissue, as platelets play a critical role in wound healing [27]. They promote initial coagulation at the wound site, as well as the release of growth factors. The main strategy of this method is to enhance and accelerate the effect of growth factors contained in platelets, which are universal initiators of the regeneration of all wounds. Plasma platelets also contain fibrinogen, fibronectin and vitronectin, which promote osteoconduction, acting as matrices for bone and connective tissue repair [28].
Treatment of generalized aggressive periodontitis is a challenging goal because it requires a multidisciplinary approach. When diagnosed at a late stage, the chance of tooth loss is up to 60%. Losing teeth at a young age can lead to psychological trauma and changes in a person's behavior. In this case, the solution to cosmetic problems is possible through combined periodontal and orthodontic therapy [29], prosthetics [30], and implant treatment. In order to maintain optimal treatment results and prevent relapses, maintenance therapy is necessary and continues throughout life. Psychotherapy also has a positive effect and should be started immediately after the first consultation with a dentist and continued depending on the psychological state of the patient [31,32].
Conclusions:
1. A characteristic feature of generalized aggressive periodontitis is the rapid destruction of periodontal tissue. The disease most often affects young people with no concomitant systemic diseases.
2. The main goal of treatment is to reduce or eliminate subgingival microorganisms, restore lost tissue and maintain periodontal health.
3. It is traditionally believed that GAgP has a poor prognosis and only radical treatment is advisable in such a situation. Modern treatment regimens for generalized aggressive periodontitis must take into account the importance of early diagnosis and the validity of combining various techniques; only in this case can we count on long-term stabilization of periodontal health.
Gum massage for periodontitis
With the help of simple manipulations, you can improve trophism and strengthen blood vessels in damaged periodontal tissues. The method is used in combination with folk recipes and traditional treatment.
It is necessary to wash your hands thoroughly and treat them with an antiseptic composition. You will need your thumb and index finger to wrap around the gum surfaces. If severe pain occurs, you must stop all manipulations and contact a dental clinic. Massage techniques:
- Stroking movements. The procedure not only begins, but also ends with this stage.
- Trituration. The degree of pressure gradually increases.
- Squeezing out the contents of periodontal pockets with intense pressure.
- Squeezing the oral and vestibular surfaces for 5-7 seconds (no more).
It is better to use essential oils. This will ensure sufficient glide.
examination and treatment of periodontitis in pregnant women
In situations where a doctor diagnoses periodontitis during pregnancy, treatment can be prescribed only after a complete examination and receipt of the results of additional tests and a complete life history. To diagnose inflammatory periodontal diseases, dentists use a comprehensive assessment method, which consists of a dental examination, the results of examination and probing of periodontal pockets, and assessment of x-rays of the jaws. After receiving all the results, the attending periodontist has the opportunity to assess the degree of damage to periodontal tissues, on the basis of which therapy is planned.
Complications
Inflammatory processes are extremely undesirable for the human body. When the doctor understands what causes periodontitis, why it is dangerous, and how to determine its type, it is possible to develop a therapeutic regimen and eliminate negative manifestations in a short time. However, most often patients run to the clinic when it is already too late. Bacterial flora and toxins gradually penetrate the bloodstream and are delivered to all organs and systems. As a result, acute respiratory viral infections, endocrine disorders, and systemic diseases are provoked. In its advanced form, the walls of blood vessels become thinner, and atherosclerosis develops, which leads to strokes and heart attacks.
Symptoms of the complicated stage:
- severe toothache;
- constant weakness, fatigue, apathy;
- persistent increase in body temperature;
- discharge of pus from the alveoli;
- destruction of alveolar processes.
What is the difference between periodontitis and periodontal disease?
Periodontal disease is a disease that is accompanied by the destruction of bone tissue and does not lead to inflammatory processes. These diseases differ in the nature of treatment, causes, frequency of occurrence, etc. Periodontal disease occurs in no more than 3% of the population, develops with diabetes mellitus or due to a hereditary factor, and is sluggish (periodontitis is more intense).
With periodontal disease, the gums very rarely bleed, their swelling is not observed, the process of development of the disease always covers the entire dentition. Periodontitis can be focal or widespread.
Prevention
Following these recommendations will help prevent this insidious disease and protect against other oral diseases:
- regularly brush your teeth and perform hygiene procedures;
- use a high-quality brush and paste;
- prevent dental diseases and gum problems;
- strengthen immunity;
- avoid stressful situations and experiences;
- eat right, include foods rich in vitamins and minerals in your diet;
- if you have problems with your bite, visit an orthodontist to develop therapeutic tactics;
- in the absence of dental units, install dentures, do not leave empty sockets;
- undergo regular preventive examinations at the dental clinic, harden yourself, and be physically active.
Local factors
Insufficient level of oral hygiene
The inability to properly brush your teeth with a special children's toothbrush and the reluctance to regularly carry out hygiene procedures lead to the accumulation of microorganisms in the periodontal pockets, and the toxins they release trigger the inflammatory process.
Short frenulum of the tongue or lip
Insufficiently long frenulums provoke atrophy and inflammation of the adjacent gum area due to constant tension on the frenulum fibers. The inflammatory process is localized in the area of the lower central teeth.
Chewing food on one side
The habit of chewing food on one side is fraught with the accumulation of plaque on teeth that are not involved in chewing. It is necessary to explain to the child that food should be chewed on both the left and right sides.
Anomalies and deformations of the dental system
The development of the inflammatory process in periodontal tissues can be caused by both functional overload of certain teeth and insufficient load on them. The reason for this is an incorrect bite or an incomplete set of teeth (the permanent teeth have not yet grown in, and some of the baby teeth have already fallen out).
Gum injuries
This group of factors that provoke the occurrence and development of periodontitis includes chronic trauma to the gums from decayed teeth or parts of braces, as well as filling defects and damage to periodontal tissue by nails, pens, and hair clips.
Nutritional nature
Too soft food does not contribute to a sufficient load on the child’s chewing apparatus and self-cleaning of the teeth, which results in the accumulation of plaque at their base, and as a result, the appearance of tartar in children.
Which doctor should I contact for periodontitis?
If there are obvious signs of a pathological process, you must visit a periodontist at the Dentika clinic. During the initial examination, he carefully examines the oral cavity, interviews the patient about complaints, and prescribes diagnostic procedures. Consultations with dentists of related specializations are also required. Then an accurate diagnosis is made and a treatment regimen is developed.
Upon completion of therapy, it is necessary to see a specialist every 3-6 months. In this way, a sustainable result will be maintained after medical intervention.
Dental periodontitis begins and manifests itself as gingivitis - with inflammation and bleeding of the gums. Then, in the absence of therapy, the symptoms increase, pain and other signs appear. The earlier treatment is started, the higher the likelihood of effective use of traditional recipes without medications and surgical intervention.
Some patients neglect daily hygiene procedures, believing that sometimes not cleaning before bed will not have negative consequences. If you do not take care of the oral cavity, the risk of more severe pathologies that require long-term therapy and subsequent prosthetics increases. By understanding what periodontitis means, its causes, types and treatment in dentistry, you can create all the conditions for maintaining a healthy smile for many years.