One of the most severe, excruciating pains is toothache. It occurs for various reasons: caries, infection, loss of dental filling, inflammatory process, periodontal disease. In addition to severe pain, swelling of the cheeks, gums, and jaw may be observed. Failure to see a dentist in a timely manner often leads to the development of phlegmon and tooth loss. Broad-spectrum antibiotics are often used in dentistry. The drugs allow you to get rid of gumboil, inflammation, and pain. The remedies are selected individually and taken taking into account the doctor’s recommendation. Dental antibiotic in adult and pediatric dentistry - features Antibacterial agents have proven themselves in the treatment of various diseases caused by infections and pathogenic microbes. They are used to eliminate the inflammatory and infectious process in the oral cavity and maxillofacial region, as well as to suppress pathogenic microflora. This group of drugs is used in the treatment of chronic and acute pathologies (implantation, surgery, periodontology, dentistry). A dental antibiotic is prescribed for the following complications and infections: tooth abscess - an inflammatory process of the roots with abundant accumulation of pus; various inflammatory and purulent processes; periodontitis – inflammation of connective tissues (periodontal); pulpitis - a symptom of advanced caries, which often leads to the destruction of hard tissue; before surgery - to prevent inflammatory processes and complications; gumboil - gum disease. In some cases, the drug is prescribed after tooth extraction and for the prevention of dental disease. The effect of the drugs is different. Use: to disrupt the formation of supporting polymers of cell walls, block the actions of microorganism enzymes, accumulation in bone tissue. Antibiotic therapy has also proven itself in pediatric dentistry. Drugs for inflammation of gums and teeth Antibacterial drugs are effective for inflammatory processes of tooth roots and gumboils. These are purulent diseases in the subnaosteal or subgingival part. They appear in the form of purulent sacs on the gums. Incorrect and untimely treatment leads to surgical intervention. The main causes of appearance: jaw injury; complication after improper treatment of pulpitis and tooth extraction; consequences of acute respiratory viral infections, influenza; mechanical damage to gingival tissue; advanced forms of caries; inflammation of gum pockets; hypothermia. Fluxes come in different types: ossifying, ordinary, serous-albumic, purulent, fibrous. They are manifested by symptoms such as general weakness, fever, severe toothache radiating to the temple, swelling, pathological mobility of teeth, enlarged lymph nodes in the neck, redness in the localized area. An antibiotic for toothache that has developed as a result of gumboil helps at the initial stage of the disease. Medicines relieve symptoms. Additionally, vitamin and mineral complexes are prescribed to strengthen the immune system. The operation is prescribed in advanced cases. The abscess is opened under local anesthesia, cleansing is carried out, and drainage is installed to release residual purulent masses. After surgery, the patient will have to take antibacterial drugs prescribed by the dentist. Therapeutic treatment with antibiotics has a cumulative effect, so it is important to follow the dosage and not stop taking it prematurely. The choice of means depends on the cause of inflammation, the age of the patient, the characteristics of the disease and the degree of its neglect. You can use drugs such as Amoxiclav, Lincomycin, Azithromycin, Citrolet, Clindamycin, Trichopolum, Biseptol. The drugs are prescribed taking into account contraindications and individual tolerance. To avoid microbial resistance of the body, use for more than 10 days is contraindicated. In childhood, flux is rare, but leads to serious consequences due to the accelerated spread of infection in the body. At the slightest sign of suppuration, you should immediately contact a specialist. Treatment is aimed at eliminating the source of the inflammatory process and generally strengthening the body and immune system.
Dental antibiotics for periodontal disease and periodontitis Antibacterial drugs are often used in treatment regimens for periodontal disease.
Moreover, each clinical case requires a special approach. Therapy is aimed at restoring normal microbial flora. Antibiotics are prescribed in the form of tablets, injections, ointments, and gels. The medicine is selected by a periodontist taking into account the severity of damage to periodontal tissues and the results of a diagnostic examination. It is necessary to distinguish periodontal disease from periodontitis, despite the similarity of symptoms: unpleasant odor; soreness; swelling, bleeding gums; feeling of unpleasant taste; pathological mobility of teeth. Periodontitis is a consequence of exposure to pathogenic bacteria. Whereas periodontal disease often develops against the background of a metabolic-dystrophic disorder. Other provoking factors of pathology: genetic predisposition; pathological bite; gum injuries due to incorrectly selected dentures and crowns; deposits in subgingival pockets; hormonal imbalance; gastrointestinal exacerbations; infectious respiratory diseases; abnormal attachments of the frenulum; diabetes. Although there are some differences, both diseases can lead to complete tooth loss. Severe forms require long-term treatment, including antibiotic therapy. Antibiotics used in dentistry for periodontitis and for the prevention of periodontal disease are prescribed in a course (up to 10 days), in the form of tablets, injections and topically. Proper oral hygiene and nutrition are of great importance. If there is a deficiency of macro- and microelements in the body, an effective drug is selected. Professional teeth cleaning, at least 2 times a year, and regular removal of microbial plaque with high-quality pastes will prevent the development of periodontal disease. Medicines for prophylaxis Prophylaxis with antibacterial agents is a common technique in oral surgery and dentistry. Antibiotic therapy before and after surgery reduces complications. It is advisable to use products with high bioavailability and minimal side effects. Requirements for medications used for preventive purposes: increased activity against pathogenic bacteria, more often found in ondontogenic inflammatory lesions; correspondence of the spectrum of action to representatives of the microflora located in the oral cavity; good penetration into tissue, especially during operations to open phlegmon and abscess. An antibiotic when implanted in dentistry minimizes the risk of side effects. Actively fight against foci of infections and bacteria. Selected based on weight and age. Common drugs are penicillins and cephalosporins. The prescription of drugs depends on the complexity of the surgical intervention and possible complications. Prevention is mandatory in case of prolonged surgery or unfavorable treatment. Osteotropic antibiotics: what they are and what they are used for In dental practice, osteotropic antibiotics are often used. An antibacterial drug (ABP) is prescribed: to eliminate the inflammatory-purulent process (chronic and acute) in case of peristitis, abscess, odontogenic sepsis, pericoronitis; as a prophylaxis against infectious complications after implantation and surgery; patients at risk (patients with diabetes, cardiovascular problems). Antibacterial therapy is contraindicated for surgical interventions on bone tissue, bleeding, and large-area wounds in the oral cavity. Frequently used drugs for the inflammatory process Several types of antibiotics are used in dentistry for toothache and inflammation. Penicillin group. Prescribed at any age, with minimal side effects and easy tolerability. The main use is for periodontal inflammation. Effective against anaerobic bacteria. Cephalospoirins. They are used when it is necessary to perform dental manipulation with the risk of injury, as well as during periodontal and odontogenic inflammatory processes. Tetracyclines. Relieves swelling in the area of bone and soft tissue. Imidazole and derivatives. They have a depressing effect on pathogenic microorganisms and quickly penetrate bone tissue. Recommended for extensive inflammatory lesions. Macrolides. Used during pregnancy and allergies to drugs of the penicillin group. Eliminates gram-negative and gram-positive bacteria. Lincosamides. Do not cause allergies. Used for severe bone tissue infections. The prescription of osteotropic antibiotics is combined if the tests reveal different types of pathogenic microbes. Side effects and contraindications Despite the fact that the antibiotic has proven itself well for toothache and inflammation, its use is contraindicated in case of renal and liver pathologies, diabetes mellitus, and taking certain medications. Prescribed with caution to children, elderly patients, and pregnant women. Possible side effects: dermatitis, urticaria, skin rashes and other allergic reactions; diarrhea, nausea; kidney and liver damage; headache; anemia; candidiasis of the mucous membranes. Dental antibiotics are an irreplaceable thing. The drugs prevent a serious complication, but subject to the right choice and strict adherence to the doctor’s recommendations. Author: Zhukov M.A.
also read with this article A child grinds his teeth: reasons 04/23/2021 You should pay attention to the circumstances under which a child grinds his teeth in his sleep. This could be anxiety from the day before, or an uncomfortable sleeping position. If a child has been grinding his teeth for several nights, there may be reasons... How dental impressions are made 04/08/2021
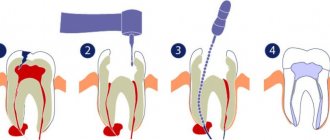
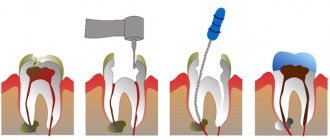
The negative reflection of the dentofacial rows, tissues and alveolar processes is called a dental cast (impression, imprint). It plays an important role in prosthetics and orthodontic treatment, stump grinding, pulp removal, and crown preparation.
Bruxism: why people grind their teeth in their sleep 03/05/2021 Bruxism is grinding your teeth in your sleep. It most often appears at night and may indicate serious health problems.
Quite often, patients come to me with complaints of increased tooth sensitivity. It is impossible to drink cold water in the summer without eating ice cream.
Typically, gum recession is to blame. Let's figure out what it is and what can and should be done to enjoy delicious ice cream without discomfort.
Gum recession is the exposure of the neck of the tooth, which is accompanied by aesthetic discomfort and increased sensitivity.
Why does gum recession occur?
Gum recession occurs for many reasons.
The main reasons for a recession are:
- Hygiene. Plaque and tartar that are not removed in a timely manner lead to “squeezing” of the gums and exposure of the neck of the tooth. Also, overly aggressive poor home hygiene leads to the same consequences.
- Pathological bite. When the tooth is positioned incorrectly, when the tooth is tilted in one direction or another, or when there is severe crowding, the periodontium (the complex of tissues surrounding and holding the tooth) is overloaded, which leads to a reduction in the gums and exposure of the tooth root.
Treatment of gum recession.
Causes
According to statistics, in most cases, periodontitis is caused by pathogenic microorganisms that arise due to insufficient oral hygiene or the presence of concomitant diseases. Let's consider a few more factors that can trigger the development of periodontitis:
- Irregular or improper brushing of teeth.
- Diseases that reduce the body's defenses (HIV, diabetes, systemic lupus erythematosus).
- Violation of the integrity of the gums due to injury.
- The presence of concomitant diseases of the oral cavity (gingivitis, caries, tartar).
- Changes in hormonal levels.
- Periodontitis is often caused by smoking.
- Malocclusion.
- Hereditary factor.
Symptoms of periodontitis
Signs of periodontitis can vary. Manifestations of the pathological process depend on the location of inflammation and the severity of the disease. The following clinical picture may be observed:
- Pain in the gums of various types (aching, throbbing, shooting).
- Gaps appear between the teeth.
- An unpleasant, putrid odor that does not disappear even after cleaning the mouth.
- Increased gum sensitivity.
- Exposure of the tooth root.
- Loose teeth.
- Bleeding gums.
Basic requirements for the treatment of periodontal diseases:
Treatment must be comprehensive. This means that the treatment plan should include methods and means aimed at eliminating the symptoms of the disease, normalizing the condition of periodontal tissues and affecting the patient’s body as a whole, i.e. the right combination of local and general treatment.
- It is necessary to strictly individualize complex therapy, taking into account the type, severity of the disease and the characteristics of the clinical course, as well as the general condition of the patient.
- A justified choice of methods and means of influencing the periodontal lesion and the patient’s body as a whole.
- Compliance with the correct sequence of application of various methods and means of complex therapy.
- During the period of remission, repeat courses of treatment to prevent exacerbation of the chronic process.
- Provide for rehabilitation measures.
- Medical examination.
Classification of periodontitis
Depending on the course of the pathological process, periodontitis occurs:
- Spicy. Characterized by rapid development. Without the necessary therapy, literally in 2 months the pathological process can lead to tooth loss.
- Chronic. The disease occurs in a latent form, tissue destruction occurs slowly, but still, after a certain time it leads to serious complications.
Depending on the location of the inflammatory process, the following are distinguished:
- Generalized periodontitis. The inflammatory process affects the periodontium completely; the cause of development is often low immunity.
- Localized periodontitis. It can be treated more quickly and often occurs due to injury to the gums.
Depending on the severity there are:
- Easy. It goes unnoticed. Signs include bleeding. The gaps between the teeth do not exceed 2 mm.
- Average. Pain in the gums appears, the teeth gradually become unsteady and gaps between the teeth of up to 4 mm appear.
- Heavy. This stage of periodontitis is characterized by destruction of bone tissue and deformation of the interdental septa. Gaps from 5 to 10 mm. Partial or complete loss of teeth is observed.
The theoretical basis for the application of these methods,
Confirmed by clinical observations, is as follows:
- With periodontitis, there is a violation of the histofunctional correlation of the tooth with surrounding tissues. Destruction of periodontal tissue leads to a decrease in the area of the ligamentous apparatus and the walls of the alveoli, a change in the topography of compression and tension zones under load, an increase in the specific pressure on the tissue, a change in the nature of the deformation of fibers and bone tissue due to a change in the direction of the spatial displacement of the tooth root.
- The dynamic function of chewing is changed, but is an additional factor in the influence of the external environment on periodontal tissue.
- There is a close connection between the chewing function and blood circulation in periodontal tissues.
- Changes in chewing functions cause a violation of histofunctional correlations in the tooth-periodontal system, manifested by circulatory disorders due to changes in vascular tone, the development of reactive and then stagnant hyperemia.
- The term “injury”, “overload” of the periodontium and “traumatic occlusion” should be understood as such a change in chewing functions when a tooth or group of teeth is exposed to an accelerated, time-drawn-out influence of the same type of chewing pressure, which causes an enrichment of vascular reactions.
- Pathological mobility of teeth in the initial stage of the disease is caused by tissue swelling and is enhanced by the destruction of the fibrous apparatus and periodontal bone tissue.
- Destruction of periodontal tissues significantly reduces their endurance, adds vertical load and is directed at an angle to the long axis of the tooth, reduces the level of adaptation and compensation.
How is periodontitis treated?
To make sure of the diagnosis, you need to visit a competent dentist, who will visually determine the primary diagnosis. In order to finally verify the presence of periodontitis, it is recommended to undergo general blood and urine tests to identify the inflammatory process in the body, as well as undergo panoramic radiography of the teeth.
Dentists at the Dr. Jacques Center offer periodontitis treatment in the following ways:
- If you consult a doctor at the initial stage, the patient will be prescribed drug therapy, physiotherapy, and, if necessary, orthopedic correction.
- When diagnosing moderate periodontitis, experts suggest performing minimally invasive interventions, such as cleaning dental pockets, antiseptic procedures for tooth roots, splinting or clasp prosthetics, which will prevent tooth loss.
- In more complex cases, full-scale surgical intervention cannot be avoided: bone augmentation or flap surgery. The purpose of the manipulation is to strengthen the gums and hide the tooth roots. The procedures are performed under anesthesia, so patients will not feel any discomfort.
Detailed video about what periodontitis is and how it is treated
Among the methods used in orthopedic dentistry, the following must be indicated:
- Selective when grinding.
- Temporary splinting.
- Orthopedic techniques.
- Reception of permanent splinting devices and prostheses.
- Direct prosthetics and splinting.
Orthopedic methods used to treat periodontal diseases can relieve inflammation, improve blood circulation and tissue trophism by eliminating pathological mobility, normalizing occlusal relationships, and relieving the traumatic effect of chewing pressure.
Types of complications with fixed dental prosthetics
The most common types of complications encountered with fixed prosthetics are:
Stomatitis and gingivitis (inflammatory processes of the gums)
Stomatitis and gingivitis
This type of complication mainly arises from improper grinding of teeth; this concerns preparation without the so-called ledge on which the lower part of the crown sits and in no case should it hang over the tooth or be pressed into the gum. The second reason may be a very massive intermediate part of the bridge, which puts pressure on the gum. Accompanied by cutting pain, redness and swelling in the pressure area. It would also be incorrect to consider too large or too small a space between the intermediate part and the gum - the rinsing space; this will lead to the accumulation of food debris and bacteria, which will ultimately cause an unpleasant odor and an inflammatory reaction. The presence of sharp edges of bridges and individual crowns can provoke chronic injury - rubbing of the tongue and cheeks . In case of any inflammatory phenomena of the oral mucosa after prosthetics, you should consult a doctor. As anti-inflammatory therapy, you can use various gels, for example Metrogyl Denta, as well as various herbal decoctions and extracts, for example Rotokan.
Dental diseases under dentures (caries, pulpitis, periodontitis)
It is important to understand that all orthopedic structures are fixed either to completely healthy teeth or to teeth prepared in advance for prosthetics. In case of insufficient diagnosis or improper preparation of the oral cavity for prosthetics, complications such as caries under the crowns, pulpitis or even periodontitis may occur. A pathological process that goes undetected in time will ultimately lead to tooth extraction. Periodontitis can also be caused by non-compliance with certain rules when planning the structure, for example, if a bridge is too long in length or a crown that is too high, which will lead to overload of the tissues that hold the tooth in the bone.
Periodontitis (inflammatory processes of all tissues surrounding the tooth)
Periodontitis
The most important cause of periodontitis in fixed prosthetics is the preparation of teeth without a ledge. As a result, the dental technician will not be able to make the correct crown on the model. It will definitely hang over the tooth and cement will remain under the overhanging edge during fixation, which will provoke a pathological reaction and it is not possible to remove this cement from there without damaging the structure. This is manifested by cyanosis of the gums, swelling and bleeding , followed by recession, darkening and exposure of the gray edge of the crown. Naturally, aesthetics are also compromised.
The choice of design depends on many factors, such as the general condition of the body, gum biotype, length of the defect, etc. If all conditions are not taken into account sufficiently, an inflammatory reaction of all tissues surrounding the tooth may occur, which will lead to rapid atrophy of the bone around the affected tooth and, accordingly, its loss. To prevent this complication, an odonto-periodontogram is often performed before prosthetics, which is a graphical recording of the condition of the periodontium and the degree of atrophy of its tissues. Odontoparodontogram during prosthetics helps to choose the correct design of the prosthesis and determine the number of supporting teeth.
Allergic reactions to materials used in prosthetics
Allergic reactions to materials used in prosthetics.
Mainly allergies after orthopedic treatment when an artificial prosthesis comes into contact with the gums and can manifest itself locally in the form of gingivitis with symptoms such as redness and rashes on the oral mucosa, burning and dryness in the mouth, or more general ones. reactions of the body, such as a rash on the skin of the face , swelling, an attack of bronchial asthma. Such reactions can appear either immediately or several hours or even days after installation of the prosthesis. Any allergic reaction during prosthetics requires analysis of the cause and subsequent treatment.
Galvanic syndrome
Such a reaction as galvanism requires special consideration. It manifests itself in the presence of various metals in the oral cavity, and this only happens on exposed metal and does not apply to dentures lined with ceramics. When saliva enters, which acts as an electrolyte, the metals acquire different potentials, resulting in the formation of galvanic currents. Symptoms of this complication are a metallic taste in the mouth, dryness, burning, headaches, sleep disturbances, and local darkening of metal dentures is possible. When galvanism is detected, it is necessary to replace all metal structures with prostheses made of more bioinert materials .
Cementation and loosening of a fixed structure
Dental cements on which permanent structures are fixed must meet certain requirements. However, sometimes de-cementation (“unsticking”) of the permanent structure occurs. This can occur from excessive load, an incorrectly ground tooth, a bridge that is too long, expired or insufficient cement for fixation, as well as one large or several small fillings on a tooth that fly off while remaining in the crown.
Chips of the lining of artificial teeth and crowns
Chips in the lining of artificial teeth and crowns
The lining of crowns and artificial teeth consists of porcelain, this material is beautiful and strong, but if overloaded, it cannot withstand deformation and chips. The cause may be an error in the planning of the orthopedic design, a technical error in manufacturing, as well as the patient's frequent consumption of too hard foods, such as nuts and bones. Sometimes chips can be restored without removing the orthopedic structure, right in the oral cavity, but only the attending physician can resolve this issue.
Malocclusion due to crowns and teeth that are too low or too high
In the case of too low clinical crowns, the efficiency of the chewing function will be quite low, and in the case of too high crowns, the entire masticatory apparatus . Malocclusion sooner or later causes even more serious disorders of the temporomandibular joint, as well as neurological disorders, which can often be expressed in the form of headaches. If the patient feels that he is not grinding food tightly and too large pieces of food remain, or feels pain in the joints after prosthetics, he should immediately consult a doctor to correct the bite.
Violation of the plane during prosthetics
For any prosthetics, the so-called occlusal plane is very important. By it we mean a plane passing through the cutting edges of the central incisors and the distal cusps of the seventh teeth separately for the upper and lower jaws. Incorrect prosthetics can lead to disruption of this plane and disruption of the movements of the temporomandibular joint. This often manifests itself with serious adverse consequences in the form of facial and headaches, pain in the joint area, and clicking when opening the mouth. Such errors require long and careful treatment. In this case, in-depth gnathological studies will be needed, which are carried out in our clinic. Gnathology examines the interaction of all organs of the dental system and affects many factors. Today, much attention is paid to the development of gnathology and neuromuscular dentistry.
Fractures of bridges and crowns
Fractures of bridges and crowns
Fractures, as a rule, can occur in those fixed prostheses that cannot withstand excessive load, as well as due to technical errors: too thin a frame or a very narrowed part. This complication mainly applies to stamped-soldered and temporary plastic structures. Stamped-brazed structures today are practically replaced by prostheses made of stronger materials. And replacing temporary plastic ones, if necessary, is practically easy and does not take much time.
Causes of complications after fixed prosthetics
Errors in diagnosis and planning of orthopedic treatment
Errors in diagnosing and planning orthopedic treatment
Perhaps the most important and most difficult stage of orthopedic treatment is planning and choice of design. An incompletely studied medical history, insufficient X-ray examinations and incorrect interpretation of images, an inattentive approach to the patient’s complaints. All this today is a gross mistake by the doctor.
Mistakes when preparing the oral cavity for prosthetics
Before orthopedic treatment, it is necessary to carry out sanitation of the oral cavity: professional oral hygiene, removal of severely damaged teeth that cannot be properly restored with fillings or inlays, therapeutic treatment of teeth necessary according to indications, and soft tissue and bone grafting is also possible. Errors in preparation can be detected after prosthetics, so a very careful approach of all doctors is necessary.
Errors in the clinical stages of prosthetics
Orthopedic treatment usually consists of several stages. Making a mistake at any of the medical stages can lead to adverse consequences. The most common medical errors in permanent prosthetics include incorrect preparation of teeth , inaccurately taken impressions, incorrect bite determination, incorrect fitting of frames, non-compliance with the rules when installing a prosthesis, as well as non-compliance with the stages of prosthetics.
Errors in technical stages of prosthetics
Half the success of proper orthopedic treatment depends on the dental technician. Failure to comply with certain rules for the manufacture of dentures leads to further complications. Most often, these are errors in the inaccurate production of plaster models, poor casting of frames, and incorrect modeling of the cutting or chewing surface of the teeth by a dental technician.
Removable tires
The splinting properties of removable splints are provided by various combinations of continuous support-retaining and reversible clasps, as well as different shapes of occlusal pads. Their spread was facilitated by the development of parallelometry techniques, precision casting on refractory models, and the use of cobalt alloys and precious metal alloys.
Removable splints can be used to splint one group of teeth or the entire dentition. When immobilizing the front teeth, it is advisable to bring the splint to the premolars, and when splinting the lateral teeth, to the canines.
Removable splints can be included in the design of the arch prosthesis as its integral part. These are prosthetic splints:
1) continuous clasp type tire;
2) splint guard;
3) a single splint for the entire dentition.