The temporomandibular joint is a complex paired anatomical formation that provides horizontal and vertical movement of the lower jaw relative to the lower jaw. The load on the joint is determined not only by the quality of the food that needs to be chewed, but also by the condition of the dental system. The condition of the temporomandibular joint (TMJ) in turn affects our well-being and overall health.
According to data provided in the reports of the World Health Organization for 2021, musculo-articular dysfunction of the TMJ is detected in approximately every second person aged 20 to 50 years. And these are only those cases that are recorded in medical documentation. A fairly large number of people do not associate persistent headaches, clicking in the joints when chewing, difficulty opening the mouth with a painful condition of TMJ and are in no hurry to seek medical help.
Often, the pathology of the temporomandibular joint is detected during an examination performed for another reason, for example, in preparation for prosthetics. At the same time, the variants of joint diseases can be very different from dysfunctional syndrome to habitual joint dislocation.
Structure and functions of the temporomandibular joint
The joint is formed by the head of the horn of the lower jaw and the articular surface (fossa) of the temporal bone. Between these bone formations there is a fibrous intra-articular disc, which is fused on all sides with the joint capsule. Ligaments and muscles help keep the joint in the correct position. They limit the range of motion in the joint. Attempting to exceed this functional limitation causes pain and prevents damage to the TMJ.
The main function of the joint is to ensure movement of the lower jaw in three directions:
- vertical: opening and closing the mouth;
- horizontal: lateral displacements of the lower jaw relative to the upper;
- sagittal: movement of the lower jaw back and forth relative to the upper.
The combination of movements of one jaw relative to the other allows us to chew, speak, and express emotions through facial expressions.
Why does pain occur in the lower jaw?
Purulent diseases
The cause of pain is inflammation of the bone, periosteum or nearby soft tissue. In 70-80% of cases the disease is of odontogenic origin. Less commonly, the process is provoked by acute infections and jaw injuries. Complemented by edema, hyperemia, general condition disorder, intoxication syndrome, regional lymphadenitis. Pain is observed in the following pathologies:
- Periostitis.
The symptom is more pronounced in acute purulent periostitis. The pain is sharp, pressing or boring, radiating to the eye, ear, temple, neck. Intensifies when opening the mouth. Weakness, low-grade fever, and swelling of the cheeks are noted. In chronic periostitis, the pain is periodic, moderate or mild, pressing or bursting. The contours of the face are slightly changed. - Osteomyelitis.
Characterized by a sudden manifestation with a rapid rise in temperature to febrile levels, chills, and severe intoxication. The pain is shooting, pulsating, diffuse, radiating to the neck and half of the face. They get worse when swallowing, limiting mouth opening. The teeth are mobile, pus is released from the gums. The oral mucosa and skin of the chin become numb. In chronic osteomyelitis, the symptom increases after closure of the fistula, decreases or disappears after the outflow of pus resumes. - Perimaxillary abscess.
The formation of an abscess is preceded by toothache. Then dense swelling occurs. The pain quickly intensifies, and the symptoms of intoxication increase. The patient refuses food. After spontaneous opening, the manifestations disappear; in the absence of treatment, chronicity with periodic exacerbations, resumption of pain and suppuration is more often observed. - Perimaxillary phlegmon.
Typically acute onset with rapid progression of local manifestations, purulent-resorptive fever. The pain is jerking, aggravated by talking, chewing, and moving the lower jaw, and is complemented by increased salivation and the formation of a diffuse infiltrate with a fluctuation zone. The condition continues to deteriorate due to severe intoxication.
Traumatic injuries
Injuries to the lower jaw most often result from fights. Damage due to falls, car accidents, or industrial accidents is possible. In case of a bruise, the asymmetry of the face is caused by swelling of the soft tissues; the closure of the teeth is normal. The symptom is moderate, quickly decreases, and does not create serious obstacles to articulation or food intake.
Among the fractures, injuries to the body predominate; violations of the integrity of the angle and branches are less common. Half of the fractures are bilateral. At the time of injury, a sharp explosive pain occurs, decreasing only slightly over time, intensifying when talking, biting, or chewing. Possible numbness of the chin and lower lip. Facial asymmetry, articulation disorders, stepped dentition, mobility, and sometimes tooth dislocations are noted.
Fractures of the alveolar process of the lower jaw are less common than the upper jaw; they develop from impacts, falls from a height, etc. They are accompanied by intense spontaneous pain, which intensifies when swallowing or attempting to close teeth. The mouth is half-open, and the protruding edge of a bone fragment can be seen under the mucosa. The bite is broken, the teeth are mobile, dislocations are possible.
Pain in the lower jaw
Neuralgia
The symptom is accompanied by trigeminal neuralgia involving the 3rd branch (n.mandibularis). It is provoked by external factors (shaving, cold air, water), stress on the masticatory muscles. Prosopalgia is paroxysmal in nature and is a series of pain impulses that are felt like a lumbago or electric shock from the side of the face along the lower jaw to the chin. The pain is sudden, lasts several minutes, reaches such intensity that the patient freezes, does not move, does not speak.
With neuralgia of the glossopharyngeal nerve, the pain impulse is caused by chewing, swallowing, talking, lasts from several seconds to 3 minutes, occurs at the root of the tongue, spreads through the tonsils, palate, pharynx, ear. Radiating pain in the lower jaw. In patients with ganglionitis of the submandibular node, the pain is paroxysmal, burning, boring, pulsating. Lasts from 1 minute to 1 hour. They begin in the tongue, spread to the lower jaw, temple, back of the head, neck, and shoulder girdle.
Muscle damage
Bruxism is formed due to spasm of the masticatory muscles. After night attacks, patients are bothered by pain in the jaws, caused by clenching and intense movements relative to each other. Muscle pain, dental pain, headaches, dizziness, and drowsiness are possible. With myofascial syndrome, pain develops due to overload of the masticatory muscles. It is perceived as moderately expressed and deep. At first it appears only under load (chewing, clenching the jaws), then it increases and becomes constant.
Dental reasons
The symptom is disturbing in the first days after tooth extraction. It is especially pronounced in the presence of an inflammatory process, removal of impacted or incorrectly erupted wisdom teeth. Some patients report pain due to wearing braces and dentures. Aching, pressing or pulling pain in the jaw and masticatory muscles, problems with chewing and swallowing, biting the cheeks and tongue are detected in children with malocclusion.
The cause of severe progressive paroxysmal pain, which spreads to the entire lower jaw and intensifies at night, is acute diffuse pulpitis. Prolonged intense pain under the influence of external stimuli, spontaneously occurring pain attacks are also observed during the period of exacerbation of chronic pulpitis. Irradiation along the trigeminal nerve is typical. Between attacks, moderate or minor aching pain is possible, aggravated by biting.
Tumors of the lower jaw
Pain syndrome is characteristic of a number of odontogenic and non-odontogenic benign neoplasms. Distinctive features of such neoplasias are slow growth and lack of germination of surrounding tissues:
- Odontogenic fibroma.
More often diagnosed in children. The pain is aching, not intense, and does not occur in all patients. It can be combined with tooth retention and inflammation in the affected area. - Cementoma.
As a rule, it is localized in the area of molars or premolars of the lower jaw. The course is asymptomatic or with minor pain that increases with palpation. - Osteoma.
Accompanied by pain, facial asymmetry, slowly increasing over months or years. Large tumors limit the mobility of the lower jaw. - Osteoid osteoma.
Unlike other neoplasms, the pain is sharp, intense, intensifying at night and when eating. The face is asymmetrical, in the oral cavity there is a bulge in the area of premolars or molars. - Osteoblastoclastoma.
More common in adolescence and young adulthood. Facial asymmetry, tooth mobility, aching, bursting pain gradually progress. Over time, fistulas form over the neoplasia. Pathological fractures are likely.
Malignant neoplasms of the lower jaw are found less frequently than benign ones. Cancer is characterized by a rapid increase in pain, radiating to the cheek, ear, eye, and temporal region. Accompanied by mobility, tooth loss, germination of masticatory muscles, salivary glands, and ulceration. Osteogenic sarcomas rapidly progress and quickly infiltrate soft tissues. Over the course of several months, the pain increases from moderate, pressing, aching or bursting to constant, unbearable, and can only be eliminated with narcotic analgesics.
Cardiac ischemia
Irradiation into the lower jaw can be observed with angina pectoris and myocardial infarction. Painful sensations are caused by the spread of impulses from the heart to the upper thoracic segments of the spinal cord, from there, along other nerves - to the face, neck, left arm, left shoulder blade. The main symptom is burning, pressing, squeezing or bursting pain behind the sternum.
An attack of angina lasts several minutes and is eliminated after stopping physical activity and taking nitroglycerin. During a heart attack, the pain is wave-like, very intense, lasts more than 30 minutes, and does not disappear when using the methods listed above. In the atypical course of a heart attack and coronary artery disease, retrosternal pain may be absent, only reflected pain is observed, including in the jaw.
Causes of dysfunction of the masticatory joints
A gnathologist specializes in the diagnosis and treatment of TMJ diseases. In fact, this is a dentist with a narrow specialization. Factors that can lead to temporomandibular joint disease include:
- vascular pathology, which leads to impaired blood supply to the joint;
- increased tone of the muscles of the face and neck (increased tone, spasms);
- violation of occlusion;
- manifestations of psychosomatics.
Occlusion disorders underlie the largest number of cases of TMJ disease. Normally, the antagonist teeth of the upper and lower jaws contact their chewing surfaces in a certain way. The cusps and depressions on the upper surface of the antagonist teeth should contact according to the “pestle and mortar” principle. If the teeth on the jaw are positioned incorrectly and their correct contact is impaired, compensatory mechanisms are activated. In particular, the tone of the chewing muscles changes and the lower jaw shifts in such a way as to achieve full contact of all chewing surfaces of the teeth.
This displacement eliminates the occlusal obstacle, but creates additional stress on the temporomandibular joint. Habitual displacement of the jaw over time leads to damage to the anatomical structures of the joint. Increased tone of the masticatory muscles provokes hemodynamic disturbances in the TMJ area, which does not contribute to rapid regeneration.
If the cause of unpleasant symptoms in the TMJ area is a violation of occlusion, a gnathologist may recommend orthodontic treatment. This is the only way to get rid of the problem, since if the teeth are incorrectly positioned on the jaw, only symptomatic treatment of TMJ problems can be carried out, which will only lead to a temporary improvement in the condition.
Supporting actions
Self-massage of the jaw area is necessary for developing muscles and joints. It is carried out using the following techniques :
- stroking;
- rubbing (with gentle pressure);
- effleurage
Before the procedure, the patient will need to thoroughly wash their hands and treat them with a small amount of oil, which will ensure good gliding of the hands over the skin. After this, you need to walk lightly over the problem area, spending no more than 5 minutes on each part of the body. The total duration of the massage should be within 15 minutes. You can massage the jaw area 2-3 times a day.
Gymnastics should be done only after a doctor’s prescription. It includes a series of strengthening and relaxing procedures that reduce pain and also allow the patient to get rid of crunching in the jaw area.
Examples of muscle relaxation exercises:
- the patient massages the chin area for 5 minutes, and then slowly pronounces all the letters of the alphabet, starting with the letter “B” and adding the sound “A” to each of them. The result is the syllables “Ba”, “Va”, “Ga”;
- the patient pronounces the letters of the alphabet, while simultaneously massaging the area of the chin and jaw;
- to strengthen the ligaments, the patient opens his mouth, stretches out his tongue to the fullest extent and tries to pull it towards the chin, in this position he lingers for 10 seconds. The exercises are repeated 15 times.
Therapeutic exercises can be performed 2-3 times a day. It is advisable that it goes away a few hours after eating. The duration of classes should not exceed 15 minutes. During the process, all movements must be smooth; strong jerks can lead to increased pain.
What to do if you have jaw pain:
Symptoms and prevention of TMJ dysfunction
Pain in the masticatory joint is an extremely rare occurrence. In this regard, patients rarely associate the existing pathological manifestations with the condition of the TMJ. Let's see what symptoms you need to make an appointment with a gnathologist:
- Headache. There are a great many causes of headaches, but the “contribution” of the temporomandibular joint is most often “forgotten” by specialists. Elimination of TMJ pathology often relieves a person of headaches.
- Clicking in the joint. The characteristic sound when opening the mouth is a consequence of dislocation or subluxation of the masticatory joint, which usually resets on its own.
- Limitation of mouth opening. This may be a consequence of swelling of the joint tissue as a result of the development of an inflammatory process or dislocation of the joint.
- Pathological abrasion of tooth enamel.
Measures to prevent the development of TMJ dysfunction include regular visits to the dentist, rational prosthetics, timely treatment and restoration of damaged teeth, and orthodontic treatment as indicated.
Types of neck and jaw pain
The neck may hurt on the left side under the jaw, or the pain occurs on the right or in the front and radiates to the back. The nature of pain can be very different, due to one or another reason for its occurrence. The nature of the pain is very important for making a diagnosis, so it is necessary to describe it to the doctor as accurately as possible.
Intense pain on the sides of the neck under the jaw
Most often, such pain occurs due to inflammation of the lymph nodes and tonsillitis. Both diseases are the result of an infection entering the body. Migraines and dental infections can also cause severe pain under the jaw.
It's a dull pain
If the pain is aching in nature, then it could be caused by a migraine, which, with bright light, changes in lighting or loud sounds, intensifies and concentrates in one place. Additionally, symptoms such as vomiting, nausea, vision problems and constant thirst may appear. Aching pain can also be associated with infectious dental diseases.
Pain under the jaw on the left
If your neck hurts on the left side under the jaw, then this may indicate almost any of the diseases that were listed above; Pain can also be associated with problems in the cardiovascular system. For example, pain on the left under the jaw appears with a heart attack or angina, which, as a rule, comes from pain in the chest area and is accompanied by acute pain in the teeth.
Pain when pressing
If your neck under your jaw begins to hurt when pressed or pressed, this may indicate inflammation of the lymph nodes, as well as diseases such as auricular ganglion neuralgia, osteogenic sarcoma, or the presence of sialoliths. Any painful sensations cannot be ignored. Even if discomfort in the neck and jaw does not cause any particular problems, this is not a reason to ignore it. Seeing a doctor in a timely manner is a decision that needs to be made immediately. Only a doctor can tell why your neck hurts under your jaw and what needs to be done about it.
Diagnostics
In order to make a diagnosis, the doctor conducts an examination according to the following scheme:
- Questioning the patient. Of interest to the specialist are complaints, conditions for the appearance of unpleasant symptoms, duration of the disease, previous treatment and its effectiveness.
- External examination and palpation. The gnathologist examines the patient’s face, paying attention to the area where the TMJ is located. By feeling the joints, you can get an idea of its structure and the state of its tissues.
- Dental examination. Anomalies of occlusion and the degree of their severity are identified.
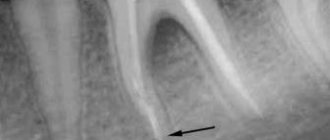
- X-ray examination. The photographs show the bone formations that form the joint. By their relative position one can determine the presence of dislocations and subluxations, and by the thickness of the joint space one can judge the condition of the cartilaginous disc.
Pain when opening a child's mouth
The peculiarity of pain in children is that the child can rarely describe the symptom in detail, as well as assess its severity. In addition, children often tend to hide from adults if they are in pain, especially if they are afraid of doctors.
Parents should pay attention to the following features:
- The child began to speak slurredly and reluctantly;
- It is painful or impossible to open your mouth wide;
- Does not eat well, tries to avoid chewing food;
- There is noticeable swelling on one side of the face;
- The baby holds on to the ear or jaw and constantly touches them.
These signs can indirectly tell parents that the baby has a sore jaw.
Treatment
A gnathologist can carry out treatment either independently or with the involvement of specialists from other fields. This is especially true when the cause of the development of TMJ pathology has been identified and can be eliminated. The help of an orthodontist is necessary for patients with malocclusion. Wearing a brace system or aligners to correct occlusion has a beneficial effect on the condition of the entire dental system.
Detection of arthrosis or ankylosis of the temporomandibular joint also requires the involvement of specialized specialists. The doctor's specialty will be determined by the cause of the development of degenerative-dystrophic processes in the tissues of the TMJ. Metabolic disorders, injuries, infections will require additional examination and the development of an individual treatment plan.
How does the mechanism of tooth pain sensitivity work?
The nerves connected to each tooth and to the gum tissue are part of one of the segments of the peripheral nervous system, namely the facial one. There is one nerve plexus for each jaw, formed by many nerve endings extending from each of the teeth. Greatly simplifying the innervation scheme of the teeth, we can say that they are all ultimately connected to the branches of the facial trigeminal nerve.
And if inflammation occurs anywhere along the innervation, pain signaling this can be felt in all tissues penetrated by nerve endings from this plexus. Therefore, patients who need treatment for caries of several teeth often come to the doctor with a complaint of pain in the entire dentition. The pain spreading throughout all the nerves of the plexus does not allow one to clearly indicate the location of its localization.
First aid
A joint dislocation or subluxation that occurs for the first time can cause severe pain. Joint dysfunction can also cause pain of the same intensity. Regardless of the cause of the discomfort, you must do the following:
- provide rest to the joint: do not eat, talk as little as possible;
- take a pain reliever;
- Consult a doctor as soon as possible and undergo the necessary examination.
Experts categorically do not recommend heating a sore joint if the cause of the pain is unknown. In case of dysfunction, heat exposure can lead to some relief of the condition, but in case of dislocation, on the contrary, it will cause harm. Under the influence of heat, blood flow to the tissue increases, which contributes to the development of edema and makes reduction difficult. Thus, when trying to help yourself or a loved one, you can unknowingly cause serious harm.
Neurological pathologies
Neurogenic pain, i.e. sensations caused by pathologies of the facial or trigeminal nerve often occur after hypothermia, head and face injuries. They are always accompanied by a number of additional symptoms, which makes it possible to determine nerve damage.
Why does it hurt to open your mouth?
It is recommended to use anti-inflammatory drugs, painkillers, warming procedures, and neuroprotectors
Opening the mouth is accompanied by pain because the affected nerve is irritated.
The nature of the sensations and accompanying symptoms
The pain can be completely different in nature.
Associated symptoms depend on which nerve is affected - pain in neighboring areas of the face, dry mouth, impaired facial expressions, cough, sore throat, swallowing problems, sore throat, inability to chew, impaired diction.
Treatment methods
The use of anti-inflammatory drugs, painkillers, warming procedures, and neuroprotectors is recommended. Operative methods are ineffective.