basic information
Syphilis is an infection that can be transmitted between people in various ways and poses a direct threat to life. Foci of syphilis can be located in intimate areas, on the arms, and torso. In recent years, cases of infection in the mouth have become more frequent. The following photos in the new collection of the site Obolezi.com will demonstrate what it looks like.
Diagnosis of secondary syphilis
Secondary syphilitic lesions of the pharynx must be distinguished from diseases such as leukoplakia, aphthous stomatitis, diphtheria, ulcerative membranous tonsillitis, and pharyngeal tuberculosis.
Friends! Timely and correct treatment will ensure you a speedy recovery!
In the tertiary period of development of syphilis of the mucous membranes
The most common and important manifestations are lesions of the oral cavity, pharynx and pharynx.
Tertiary lesions of the tongue can manifest themselves in the form of isolated gummas (soft tumor), which develop in its thickness, or as diffuse infiltration, which covers most of the tongue, and then turns into diffuse sclerosis (pronounced coarsening) of the mucous membrane and muscle tissue.
But most often the location of the tertiary form of syphilides is the soft and hard palate. Most often in this case there is a diffuse form, but in some cases limited gummous tumors are observed. The pathological process begins with virtually no pain and is a diffuse swelling, and then thickening and compaction of the soft palate, which gradually loses its mobility. Infiltrates usually have a bluish-red color. Then the gummas disintegrate and deep ulcers are formed, which have sharply defined edges.
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
Tertiary lesions in the pharynx can take the form of tubercular syphilis or gummous lesions, which are mainly localized on the vault of the pharynx and its posterior wall. Such lesions are very rarely detected before ulceration, because they practically do not bother the patient.
After the healing process of gummous-ulcerative lesions, dense scars appear, as well as adhesions between the arches, walls of the pharynx and the soft palate, which often causes atresia (fusion) of the pharynx and disruption of the swallowing process.
Risks of getting sick
If you are confident that your body is ready to withstand any challenge, know: after the first contact with a patient, the chances of being photographed showing syphilis on the face are 80%. The remaining 20% is not due to the presence of immunity to treponema, but to too little of it to cause a big problem.
Diagnosis of tertiary syphilis
Tertiary syphilis of the pharynx must be differentiated from tuberculosis, scleroma and malignant neoplasms of the pharynx. Gummous ulcerations are painless and have sharply defined edges and a bluish-red color. They do not cause the disorders that occur with pharyngeal tuberculosis. The bottom of a syphilitic ulcer is shiny, smooth and shaped like a crater. For a final diagnosis, histological examination is necessary.
More about symptoms
Symptoms vary depending on the current stage. So, at first, signs of infection appear only by the appearance of papules on the skin (or mucous membranes, in the case of a photo of syphilis in the throat), in place of which an ulcer later forms. By the end of the first stage, the ulcers disappear on their own and appear with renewed vigor in the second. With the beginning of the second stage, internal organs begin to suffer. At the third stage, total intoxication of the body occurs. The rash on the body becomes massively lumpy.
Primary syphilis: what you might not know about
From horror stories from Soviet propaganda, we know that syphilis is such a terrible disease in which the nose falls off. In addition to being properly intimidating, these ideas also had a downside. Like, if nothing hurts and your nose is still there, then it’s not syphilis... you can tolerate it.
Judging by the comments, including in my journal, many are still in such misconceptions to this day.
A little history
The science of syphilidology arose due to the enormous incidence of syphilis and its social significance. The experimental basis of syphilidology was often completely unethical experiments on people.
To understand how this terrible infection proceeds, healthy people were infected with syphilis (France, Russian Empire) or those infected were deliberately left without treatment (USA, Sweden, Norway). These absolutely inhumane experiments, however, brought a clear understanding of the stages of the infectious process and its patterns.
Onset of the disease. "Chancre"
Treponema pallidum, penetrating the body, spreads quite quickly through the lymphatic system and can enter any organs and tissues. However, the first manifestations of the disease should not be expected immediately, but after the incubation period, which averages one month. This period can vary from 9 to 90 days depending on many factors: taking antibiotics at this time, the presence of other diseases, alcohol or drug addiction; Also, the incubation period may change for those people who have encountered this infection more than once, etc.
You should know that syphilis infection can occur not only through sexual contact. And although there have been few such cases lately, they still occur.
So, after about a month, primary syphiloma (hard chancre) forms exactly in the place where the treponema was introduced. Dermatologists have a saying: “Syphilis is the first to punish the organ that sinned.”
So if the lesion is still on the genitals, and not in some other place, the “everyday” version of infection looks doubtful, although it is not excluded (and who said that medicine is easy?).
A chancre is an ulcer or erosion that, depending on its location, can look different, but, as a rule, it has a regular, round shape and clearly defined boundaries. Actually, the term “chancre” is not entirely adequate; it is more correct to say “primary syphiloma.”
The hard base of syphiloma, which gives the name to the symptom, is not always pronounced, and only a doctor can distinguish a specific ulcer from others. In most cases, chancre is completely painless, which misleads those suffering. 8 out of 10 victims, proudly entering my office and showing skin lesions, refer to very, very violent sex, sports, tight trousers and use the word “rubbed”... I have to disappoint them and send them for tests. And, on the contrary, patients who come with huge round eyes and shouts “Doctor, I think I have syphilis - it hurts so much that I can’t walk” more often find solace in some other diagnosis.
There are also atypical chancre. A chancre-felon (it is very painful), a chancre-amygdalitis (in the tonsils), a chancre-crack (in the folds of the skin, for example in the corner of the lips or the anus) and indurative edema, when the affected area swells, can develop on the fingers. But they are rare.
...And other symptoms
Other symptoms of infection include enlarged lymph nodes and lymphatic ducts. These appear as small, firm balls under the skin near the original lesion. If the primary lesion occurred on the genitals, then, accordingly, the lymph nodes will be enlarged in the groin area. The affected lymph nodes have a hard-elastic consistency, are not fused with the surrounding tissue, are not “hot”, and are painless.
The lymphatic duct may also be enlarged. It looks like a fairly dense, painless cord, reminiscent of a ballpoint pen refill that has gotten under the skin.
Attention! If you only have the last symptom, do not be alarmed, this may be a variant of the norm.
In general, the “troika” - primary syphiloma (chancroid), syphilitic lymphadenitis and syphilitic lymphangitis - makes up ALL the symptoms of primary syphilis. As you can see, syphilis already exists, but there are no falling noses yet, and not everyone will have them soon. But you need to be examined and treated, because there are no shameful diseases!
By the way, about analyzes
It is important to know that blood tests may be negative throughout the incubation period and as long as two weeks after the onset of symptoms. So if you took tests somewhere anonymously and you received a negative (good) result, but no one examined you, do not rush to rejoice. It’s better to have courage and go to a dermatovenerologist, because after the primary period (if left untreated), the secondary and tertiary periods may begin, and this is much worse.
But what about the USSR?
In the USSR there was syphilis. Both after the Civil War and after the Patriotic War. But really punitive Soviet venereology, grossly trampling on the rights of the sick in favor of the healthy, dealt with it. Only isolated cases remained, so students at that time had to see the above-described symptoms only on dummies. However, perestroika put everything in its place, now there is enough syphilis, and, of course, it is better to prevent it (read the article “
Prevention of sexually transmitted infections
"), than treatment.
If you are interested in what the secondary and tertiary periods of this disease look like (this is where the horror-horrors accumulate), what latent syphilis is, how this infection affects the nervous system and internal organs, and how dangerous this disease is for pregnant women, write questions in the comments, and I will try to answer them in the next article.
Leonid Shchebotansky
Photo istockphoto.com
Causes of stomatitis
Stomatitis under the tongue in adults is a reaction of the immune system to certain types of irritants, which are any substances. The causes of stomatitis have not been clearly identified; presumably, the body exhibits an individual reaction to certain substances or microorganisms.
Possible causes of stomatitis on the tongue in adults:
- bacteria and infections of the oral cavity (caries, gingivitis, periodontitis, etc.);
- diseases of the gastrointestinal tract of an infectious or viral type;
- respiratory diseases (ARVI, influenza, etc.);
- frequent injury to the tongue by orthopedic or orthodontic structures;
- damage to the tongue due to a chipped tooth;
- fungal infection;
- bad habits (smoking or alcoholism);
- burning the tongue or eating “spicy” foods.
In addition to the listed causes of stomatitis on the tongue in adults, inflammation of the mucous membrane can be caused by the herpes virus (herpetic stomatitis).
Treatment
Do not self-medicate under any circumstances!
The main objective of the therapeutic course is the elimination of Treponema pallidum from the body, relief of symptoms and prevention of pathology. Treatment is carried out exclusively in the venereology department of specialized medical institutions.
The treatment course consists of:
- Local therapy , which consists of washing syphilitic lesions with antiseptic drugs. Most often, the main active component of such antiseptics is chloramine. If the ulcers are bleeding, they are treated with white mercury ointment. Calomel or xeroform powders provide effective symptomatic relief. A solution of chromic acid or 10% lapis will help stop the growth of hypertrophic ulcers.
- Antibacterial therapy . Long-term use of antibiotics is prescribed. Most often, a long course of penicillin injections is given. If you are intolerant to penicillin, take tableted antibiotics of various groups.
- Taking immunomodulators helps strengthen the body's protective functions.
- Symptomatic treatment is selected taking into account the stage of development of syphilis and accompanying symptoms. For this purpose, antipyretics, painkillers, antihistamines, and agents to stimulate tissue regeneration are prescribed.
- Sequestrectomy is performed if the disease clinically subsides completely.
Important! Secondary and tertiary forms of syphilis are practically untreatable. Regular examination for this pathology will allow timely identification of the disease and its effective treatment.
The prognosis for recovery after diagnosis of syphilis in the mouth can be positive, subject to timely detection and immediate treatment of the pathology. When treating this disease, it is important to complete the full course and not mistake a temporary reduction in symptoms for recovery.
Possible complications
Complications of syphilis in the mouth often develop due to untimely treatment and diagnostic examination. In this connection, the pathogenic effect of spirochetes extends beyond the tissues in the oral cavity and to systemic organs inside the body.
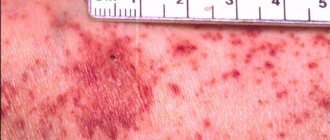
A clear example of a complication of syphilis in the mouth.
As a result, various complications arise, manifested by:
- Damage to the skeletal system and organs.
- Necrosis of the muscular skeleton at the site of the lesion.
- Local bleeding.
- Dysfunctions of the circulatory system.
- Asymmetry of the face with damage to the facial and cervical muscles.
- Destruction of the cellular structure of the brain.
It is important not to delay visiting a venereology clinic in order to prevent the development of severe consequences of this insidious disease. And it must be remembered that immunity to this venous disease is not formed and therefore, if any rash appears on the mucous membrane of the cheeks, gums, or tongue, you should seek medical advice from specialists.
Causes of syphilis in the mouth
Treponema pallidum - the causative agent of syphilis
There is congenital and acquired syphilis. The first occurs when a pathogen passes through the placenta from an infected mother to the fetus. The second develops when Treponema pallidum infects a person, penetrating through injured mucous membranes and skin during sexual intercourse.
Experts pay attention to factors that contribute to causing syphilis in the mouth:
- The use of non-sterile medical instruments in dentistry and ENT practice.
- Entry of the pathogen into the bloodstream during blood transfusion, during injections, during surgery.
- Using the same household items (cutlery, toothbrush, bath accessories).
- Oral sex.
There are circumstances that increase the risk of infection. These include:
- Injuries to the mucous wall of the oral cavity.
- Unhealthy lifestyle.
- Weak general and local immunity.
Syphilis of the throat: damage to the pharynx
The pharynx is the initial part of the digestive tract and respiratory tract. It connects the nasal cavity and the larynx, the vocal organ.
Damage to the pharynx in primary syphilis
With primary syphilis, unilateral lesions are more often observed. Chancre can be erythematous, erosive or ulcerative. Treponema pallidum has a tropism for lymphoid formations of the throat. Their defeat leads to the appearance of an indomitable cough. With the disease, regional lymph nodes always enlarge.
Damage to the pharynx with secondary syphilis
The pharynx in secondary syphilis is often affected along with the larynx. At the same time, skin rashes appear on the patient’s skin—secondary syphilides.
Damage to the pharynx in tertiary syphilis
In tertiary syphilis, damage to the pharynx occurs in the gummous form, diffuse and early ulcerative-serpentiform forms.
- The gummous infiltrate does not manifest itself in anything until ulceration appears. When gumma disintegrates, bleeding may occur and the bones of the spine and skull may be destroyed. As a result of the development of scar tissue, communication (partially or completely) between the nasal and oral cavities is disrupted. Breathing becomes possible only through the mouth, the voice changes, taste and smell disappear.
- In the diffuse syphilomatous form, multiple lesions are observed on the mucous membrane of the pharynx. At the beginning of the disease, the changes are in the nature of hypertrophic pharyngitis. But then an extensive syphilitic ulcer is formed, similar to carcinoma.
Preventive measures
Prevention of sexually transmitted syphilis is based on the following measures:
- Systematic screening for syphilis, especially if you are sexually active.
- Avoid casual sexual relationships with little-known partners.
- Mandatory use of barrier contraceptives, especially during oral sex.
Household syphilis can be prevented by observing the following preventive measures:
- Strict adherence to personal hygiene rules.
- Avoiding physical contact with an infected person.
- When living together with a sick person, there must be strictly individual dishes, personal hygiene items, clothing and bedding.
- Systematic disinfection of bathroom items.
Reference! Preventive therapy is prescribed to family members who have a sick person.
Prevention of congenital syphilis consists of:
- Preliminary examination for syphilis at the preparatory stage for pregnancy.
- Throughout pregnancy, undergo routine examinations for syphilis RPHA.
- If the results are positive, the woman undergoes mandatory treatment.
- Undergoing preventive treatment provided that the woman has previously had syphilis.
Within 2 days after sexual contact with a possibly infected person, you can get emergency prevention of syphilis from a venereologist.
Basics of pathology
Oral syphilis is a type of sexually transmitted sexually transmitted disease. The pathology is caused by a pale spirochete localized on the oral mucosa. The first signs are visualized in this part of the body.
According to the International Classification of Diseases according to etiology, syphilis is classified into:
- Congenital
- Acquired
Important! Syphilis in the mouth can be treated only at the initial stage of pathology development. If left untreated, the infection quickly spreads through the flow of blood and lymph to all organs and tissues.