Tooth extraction is a dental operation that is performed strictly for medical reasons. Reasons for tooth extraction may include severe traumatic tissue damage, incorrect position in the jaw, the formation of a large cyst, or advanced pulpitis.
Tooth extraction can be simple or complex. Even when the procedure is performed by an experienced dentist, negative consequences cannot be ruled out. One of the possible complications of the operation is inflammation of the periosteum, or periostitis.
Content:
- What is bone tissue?
- Why does atrophy occur?
- What does it lead to?
- How to recover
- How to avoid atrophy
Bone atrophy after tooth extraction is a very common problem.
If you do not resort to implantation in time, the gums will gradually begin to sag. Subsequently, when a decision is made about implantation, it may turn out that there is simply nowhere to place the implant. To exclude atrophy, it is important not to postpone dental treatment until later. In the near future, after tearing out the unit, you should discuss the possibility of prosthetics with your dentist.
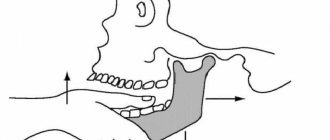
Dislocation of the lower jaw
If the mouth is opened wide during anesthesia and tooth extraction, dislocation of the lower jaw may occur. This complication is more common in patients with habitual dislocation. The occurrence of dislocation can be facilitated by relaxation of the masticatory muscles under the influence of conduction anesthesia.
Clinic and diagnosis of dislocation of the lower jaw
The clinic and diagnosis of mandibular dislocation is based on the patient’s complaints and clinical examination. The main complaint is pain in the preauricular area and the inability to close the teeth. Pain in patients with habitual dislocation may be moderate, as well as in patients who have undergone conduction anesthesia
Clinical manifestations: the patient cannot close his mouth; in case of unilateral dislocation, the jaw is shifted to the healthy side; in case of bilateral dislocation, it is shifted forward.
A symptom of elastic mobility is characteristic of a dislocation. The doctor, grasping the lower jaw on both sides with his index fingers and thumbs, attempts to establish it in a position of central occlusion. To some extent this is successful, but as soon as you stop holding the lower jaw, it returns to its original position.
Dislocation of the temporomandibular joint a - anterior b - posterior
Treatment of lower jaw dislocation
We complete the tooth extraction and then treat the dislocation of the lower jaw.
First way. The chair is lowered, its back is set vertically. The patient rests the back of his head against the headrest and fixes his hands on the armrests. The doctor stands in front of the patient, wraps the thumbs of the right and left hands with gauze napkins or a towel. He then grabs the lower jaw with both hands so that the thumbs rest on the chewing surface of the molars, and the rest cover the lower edge of the jaw. After this, the doctor presses firmly with his thumbs on the molars, moving the lower jaw down. Without ceasing to push the lower jaw down, the doctor moves it posteriorly. The sound of a click and the disappearance of the symptom of elastic fixation indicate that the dislocation has been eliminated. Having warned the patient about the possibility of recurrence of the dislocation when the mouth is opened wide, the doctor applies a chin-parietal bandage to the patient to limit the opening of the mouth. It is recommended to wear the bandage for 5-6 days.
Second way. The patient is seated in a chair in the same position. The doctor stands in front of the patient, inserts the index fingers of the right and left hands into the vestibule of the mouth and moves them along the anterior edge of the branch as high as possible, to the top of the coronoid process. Then the doctor sharply and firmly presses on the anterior edge of the coronoid process. The essence of the method is that, having felt pain in the area of the anterior edge of the coronoid process, the patient tries to avoid it by eliminating the pressure of the doctor’s fingers. He cannot move his head and entire body backwards, as they rest against the back and headrest of the chair. Therefore, subconsciously he tries to move the lower jaw down and back, i.e. carry out the movement of the lower jaw that is necessary to eliminate the dislocation. In this case, the doctor does not have to overcome the force of contraction of the masticatory muscles, as is done when using the first method to reduce a dislocation.
What is bone tissue?
This is the connective tissue of the jaw that performs a protective and supportive function. It is formed by two types of cells (osteoblasts and osteoclasts) and intercellular substance. The latter includes calcium chloride and fluoride, collagen fibers, due to which the bone becomes elastic and more elastic.
The functions of osteoblast cells are the production of collagen and calcium salts, osteoclasts are the destruction of bone and a decrease in its volume. Throughout life, creative processes in the jaw are replaced by destructive ones. While a person is young, this balance is maintained, but over the years, regenerative reactions become less active. As a result, after about 40 years, the influence of osteoclasts becomes more pronounced.
It is for this reason that if a tooth is pulled out from an adult, the gums will begin to sag quite soon. Without adequate chewing load, the bone will decrease in size. To restore the pressure necessary for full functioning of the jaw, it is necessary to undergo implantation or prosthetics.
Why does atrophy occur?
Removal of dental bone tissue is not carried out on purpose. Atrophy is almost always the result of a long “downtime” of a certain area of the dentition. Among the factors contributing to the problem:
- advanced inflammatory gum diseases;
- periodontal damage;
- purulent inflammation of the maxillary sinuses;
- acute/chronic pathologies of the thyroid gland;
- vitamin D deficiency;
- long-term use of glucocorticosteroids and some other medications;
- congenital anomalies of the upper or lower jaw;
- hereditary tendency to the disorder.
But most often, bone tissue subsides after tooth extraction. This is the main cause of the disease. While chewing food, the blood supply to the bone increases. It is due to this that its original volume is preserved. After tearing out the unit, the empty area is no longer subject to the necessary chewing load. Local blood supply deteriorates. Then the bone decreases. In one year, its volume decreases by approximately 25%.
Osteoma is a benign formation of mature bone tissue. Some authors do not consider osteoma a true tumor, believing that it arises as a result of disorders of embryonic development and bone formation.According to our data, osteoma occurs in 8% of patients with bone tumors of the jaws, more often in young and middle-aged women. There are peripheral and central osteoma. Peripheral osteoma in the form of a round, less often irregularly shaped bone formation is connected to the jaw with a narrow or rather wide base, leading to facial deformation.
The central osteoma, emanating from the endosteum, is located deep in the jaw bone, has a small size (up to 1.5 cm), and is asymptomatic. It is possible that its appearance in the form of a focus of osteosclerosis is a reaction to irritation during a chronic periodontal process. Based on the structure of the tumor tissue, a distinction is made between compact and spongy osteoma. Closely adjacent to the osteoma are exostoses and osteophytes, localized on the alveolar process of the jaw in the form of small bony protrusions. Their nature is controversial; most authors do not classify them as tumors. They grow extremely slowly, but by causing deformation of the alveolar process, they interfere with the manufacture of a denture.
The clinical picture of osteoma depends on its size and location. It increases slowly, painlessly, develops in various parts of the facial skeleton, and is detected by chance or when facial deformation is detected. Functional disorders can occur when osteoma is localized on the upper jaw (diplopia, difficulty in nasal breathing), on the zygomatic arch (limited mouth opening). Osteoma of the styloid process (in the form of a so-called megastyloid) leads to unpleasant sensations and pain in the retromaxillary region and the corresponding half of the throat. No malignancy of osteoma is observed.
The X-ray picture of osteoma, especially compact osteoma, is characteristic. On an x-ray, it appears as a more dense formation than bone, with clear boundaries, extending beyond the jaw in the peripheral form. Spongy osteoma is heterogeneous on the radiograph; there is an alternation of areas of compaction and rarefaction. Differential diagnosis, especially of spongy osteoma, is carried out with ossifying fibroma, chondroma, osteosarcoma. Macroscopically, osteoma tissue is spongy or dense bone.
Microscopically, the tissue of compact osteoma resembles the structure of the cortical layer of mature bone, but differs from it in the disruption of the general structural plan: the osteon canals (Haversian canals) are arranged randomly, osteons have a bizarre shape. Spongy osteoma is represented by an interlace of convoluted bone beams of varying degrees of maturity, enclosed in cellular fibrous tissue.
Treatment of osteoma involves excision within the unaffected bone. The operation is used for cosmetic and functional indications, as well as in case of difficulties with dental prosthetics. If it is impossible to carry out surgical treatment (impaired general condition of the patient, hard-to-reach localization of osteoma, etc.), dynamic observation is established.
The prognosis for life is favorable.
Osteoid osteoma and osteoblastoma are benign osteoblastic tumors that are closely related to each other, although they have some differences in clinical manifestations. They are rare, mainly in middle-aged people.
Osteoid osteoma develops in the cortical layer of the jaw. Being located superficially, it initially causes a feeling of awkwardness, then mild pain, more at night, during meals. The mucous membrane over it becomes hyperemic, and palpation reveals a painful swelling of the bone of small sizes (up to 1 cm). Some authors associate the presence of a painful symptom with sclerosis of the surrounding bone. Osteoblastoma is located in the spongy substance, is characterized by large sizes (more than 1-1.5 cm), with it, as a rule, there is no pain and hyperemia of the mucous membrane.
X-ray examination of osteoid osteoma reveals a focus of bone loss up to 1 cm in diameter with clear contours and surrounding sclerotic bone. Sometimes a bone compaction is detected in the center of the lesion. In osteoblastoma, there is no zone of reactive bone formation in the surrounding tissue, and the rarefaction focus is larger than in osteoid osteoma.
Tumors are differentiated from neuritis, trigeminal neuralgia, chronic osteomyelitis, and cystic lesions of the jaws.
Macroscopically, both tumors are a red soft tissue formation, often with an area of ossification in the center; with osteoid osteoma, the surrounding bone tissue is whitish due to sclerosis.
Histological examination reveals cellular, highly vascularized tissue consisting of immature bone and osteoid. In some cases, osteoblastoma is difficult to distinguish from osteosarcoma.
Treatment consists of removing the tumor along with sclerotic areas of the surrounding bone. In case of incomplete removal, relapse is possible.
The prognosis for life is good.
Ossifying fibroma (fibroosteoma) - this benign tumor is found only in the jaw bones. Clinically and radiologically, it proceeds identically to fibrous dysplasia, differing from the latter in its clear boundaries and the presence of a capsule. Previously considered as a focal form of fibrous dysplasia.
Ossifying fibroma is differentiated from desmoplastic fibroma, ameloblastic fibroma, and benign cementoblastoma.
Treatment consists of removing the tumor and capsule.
The prognosis is favorable, recovery occurs.
Osteosarcoma is a highly malignant tumor characterized by direct formation of bone or osteoid by tumor cells. It occurs most frequently (up to 50%) among other primary bone malignant neoplasms of the jaws. Even in the initial stage, osteosarcoma gives hematogenous metastases to the lungs, which are sometimes detected earlier than the primary tumor. In a large percentage of cases it affects young and middle-aged men. They note a more frequent localization in the lower jaw compared to the upper jaw.
Often the appearance of a tumor is preceded by trauma. A painful, localized tumor occurs on the outer surface of the jaw or alveolar process. The teeth within the swelling move forward and become mobile. The tumor grows quickly, within 1-2 months, and bulging appears on the side of the oral cavity. On palpation, the tumor is motionless, of dense consistency, the mucous membrane above it stretches, becomes pale, and an expanded vascular network is visible. Intense pain occurs at night, and paresthesia occurs in the corresponding areas. In the late stage of the disease, the tumor reaches a large size. A pathological fracture of the jaw is possible. Regional lymph nodes do not enlarge. Weakness and loss of appetite are noted.
The X-ray picture of osteosarcoma presents two main types of changes: osteoplastic (sclerotic) and osteolytic (osteoclastic). In the osteoplastic form, pronounced osteosclerosis is observed without visible destruction of bone substance. The tumor is detected in the form of a bone compaction with unclear boundaries and the presence of diverging spicules - bone needles located perpendicular to the surface of the jaw (“needle periostitis”). The osteolytic variant is characterized by an irregularly shaped bone tissue defect with blurred, uneven contours. The cortical layer at the border of the defect splits and rises at an acute angle in the form of a spur or visor. The presence of the latter makes it possible to complete the outer contours of the tumor. Sometimes there is a mixed version.
Diagnosis of osteosarcoma, especially in the initial stage and in the case of an osteolytic variant of the tumor, is difficult. It is differentiated from the inflammatory process of giant cell tumor (lytic form), Ewing's sarcoma. The diagnosis must be confirmed morphologically. If it is impossible to obtain punctate for cytological examination, an open biopsy is performed.
Macroscopically, the tumor in its osteoplastic form is a dense bone-like tissue of a whitish color with foci of decay, in the osteolytic form it is a crumbling bleeding mass. Morphological study reveals polymorphism of the tumor tissue; undifferentiated spindle cell tissue may be present.
Treatment of osteosarcoma involves resection of the jaw and surrounding soft tissue. Combined treatment with preoperative radiation is used for radiosensitive tumors, but often the tumor is resistant to ionizing radiation. Radiation therapy is used only for palliative purposes.
The prognosis is unfavorable, but treatment of patients with an early stage of the tumor in isolated cases leads to recovery.
"Surgical Dentistry" edited by Robustova T.G.
Fourth edition. Moscow "Medicine" 2010
Clinical examples:
- Ameloblastoma of the mandible
What does it lead to?
Many patients believe that atrophy is a completely harmless consequence of tooth loss. After all, visually this problem almost does not manifest itself at all. But that's not true. As the bone subsides, aesthetic defects in appearance arise and disturbances in the functioning of internal organs occur.
The most common consequences of decreased jaw bone volume are:
- change in appearance - an asymmetrical oval of the face appears, lips and cheeks seem to fall inward;
- a large number of wrinkles form in a short period of time;
- diction changes - the person becomes “lisp”;
- diseases of the gastrointestinal tract occur (this is due to poor quality of chewing food, swallowing large pieces);
- changes in bite, displacement of teeth adjacent to the atrophied area;
- impossibility of implantation without prior bone grafting.
How to recover
Most often, to eliminate the effects of atrophy, dentists prescribe surgery. Medicines cannot correct the situation. They often turn out to be useless, even if they just need to slow down regression.
Among the most effective methods of returning the original volume of the bone structure:
- Sinus lift. Suitable for working on the upper jaw only. During the intervention, the surgeon raises the bottom of the maxillary sinus to the height required for implantation. He fills the resulting cavity with special shavings. After sinus lift, you can proceed to implantation.
- Osteoplasty. An operation to transplant a small area of donor/own material. If necessary, the doctor can use synthetic material. The technique is popular because it takes little time. At the same time, the risk of rejection of the transplanted area is minimal.
- Tissue regeneration. An innovative technique that involves growing new bone tissue directly in the patient’s mouth. To obtain the desired result, a special protective membrane is placed in the deformed area. It creates a space in which regenerative processes take place as actively as possible.
- Transplantation of the prepared block. Indicated if you need to restore a large atrophied area of the jaw. The doctor takes material for transplantation from the patient’s bone, obtained from the palate, beard. It is also possible to use donor blanks.
The specialist decides which of the available methods is suitable for a particular patient on a personal basis.
Fracture of the alveolar process of the jaw
A fracture of the alveolar process of the jaw can occur either due to the fault of the doctor (rough work, violation of the removal technique) or due to a pathological process (soldering of the tooth to the alveolar wall). Types of fracture of the alveolar part of the jaw: • fracture within the alveolus of the tooth being removed; • fracture within the periodontium of several teeth; • fracture of the alveolar process, extending beyond the dentition (fracture of the tubercle of the upper jaw).
Causes of fracture: • Compression of the bone during fixation of the forceps. • Too active dislocation, which leads to bending and breaking of the alveolar wall. • Pathological processes leading to a decrease in bone strength (cysts, tumors, osteomyelitis). • Osteoid type of articulation.
Diagnosis of a fracture of the alveolar process of the jaw
Diagnosis of a fracture of the alveolar process of the jaw is based on the nature of the complaints, medical history, examination and x-ray examination. Sometimes when a fracture occurs, you can hear a characteristic sound - a crack. When the alveolar process of the upper jaw is fractured along with the tubercle, quite severe bleeding from the venous plexus may occur.
Symptoms: • appearance of foamed blood in the wound; • passing a stream of air into the mouth during an increase in pressure in the nasal cavity (oronasal test); • the appearance of blood from the nasal passage on the affected side.
Treatment of a fracture of the alveolar process of the jaw
If the fragment of the alveolar process remains connected to the soft tissues, then it is fixed with a metal splint. Otherwise, the fragment is removed and the sharp edges are smoothed. After this, an osteotropic biological preparation can be injected into the alveolus, and the edges of the gums can be brought together with sutures.
How to avoid atrophy
It is much easier to avoid a problem than to look for ways to solve it later. The only way to prevent jaw atrophy is timely implantation. Under no circumstances should you walk around with an unsightly toothless smile for a long time.
If the bone begins to decrease due to periodontitis, severe thyroid disease, or hormonal imbalance, you should undergo proper treatment. At the same time, the patient needs to carefully monitor the health of his teeth and gums and unquestioningly follow all medical prescriptions.
A healthy and balanced diet is crucial in the prevention of atrophy. All people should eat fresh vegetables and fruits every day. While chewing them, the necessary load is created on the jaws, and the blood supply to the tooth roots increases.