AUTHORS: Daniel London, Oded Nahlieli
Keywords:
sonography (ultrasound), salivary glands, parotid gland, submandibular gland, sublingual gland, stones, tumor, inflammation
Key points
- The salivary glands are superficial and can therefore be examined in detail using ultrasonography.
- It is important to scan each gland sequentially according to the protocol.
- The salivary glands can be affected by inflammatory, benign and malignant pathology, which can be detected sonographically.
- The salivary glands may have congenital anatomical abnormalities and may contain calculi, which are also detected sonographically.
- The purpose of the article is to gain in-depth knowledge about the structure of healthy glands, available sonography techniques, pathological changes and differential diagnosis of diseases.
Embryology
The parotid gland, like other major salivary glands, develops from the epithelium of the oral cavity. The gland bud appears in the embryo at the 6th week of development in the depths of the groove separating the cheek from the gum, in the form of an epithelial cord, which grows towards the ear. At the 8th week. embryonic development, the distal end of this cord begins to branch and gives rise to excretory ducts and terminal secretory sections of the liver. At the beginning of the 3rd month, gaps appear in the anlage of the excretory ducts, their epithelial lining becomes double-rowed, and in large excretory ducts multilayered. Differentiation of glandular epithelium in the terminal secretory sections of the liver. occurs somewhat later than in other salivary glands.
Content
- 1 Etymology
- 2 Structure 2.1 Location
- 2.2 Blood supply
- 2.3 Lymphatic drainage
- 2.4 Nervous nutrition
- 2.5 Histology
- 4.1 Causes 4.1.1 Mumps
- 5.1 Mumps
- 6.1 Bacterial infections 6.1.1 Acute bacterial parotitis
- 6.2.1 Mumps
- 6.3.1 Systemic lupus erythematosus
- 7.1 History and examination
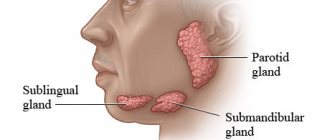
Anatomy
Rice.
1. Variants of the parotid gland and parotid duct (but B. G. Ali-Zade and M. K. Artemova, according to S. N. Kasatkin): a - trapezoidal parotid gland and straight parotid duct; b - semilunar-shaped parotid gland and arcuate parotid duct; c - triangular-shaped parotid gland and geniculate parotid duct; d — oval-shaped parotid gland and the ascending direction of the parotid duct; 1 - parotid gland, 2 - parotid duct; 3 - chewing muscle. In the Parotid Gland, there is a superficial part (pars superficialis), adjacent to the masticatory muscle, and a deep part (pars profunda), extending into the mandibular fossa (fossa retromandibularis). Sometimes a pharyngeal process extends from the inner edge of the gland. O.J. most often it has an irregular pyramidal or trapezoidal shape, sometimes crescentic, triangular or oval (Fig. 1).
In a newborn O. has a mass of 1.8 g, contains a lot of loose connective tissue and blood vessels, its secretory function in the first 6 weeks. insignificant. The gland grows most intensively up to 2 years, increasing 5-6 times. At the end of the 2nd year of life, gistol ends. differentiation of the skin, its growth slows down.
In an adult O. weighs 20-30 g; its vertical size is 4-6.5 cm, sagittal 3-5 cm, horizontal 2-3.8 cm. In old age, the size and weight of the body. are decreasing.
Rice. 2. Scheme of the parotid gland bed (horizontal section): 1 - skin; 2 - subcutaneous tissue; 3 - superficial layer of the fascia of the parotid gland; 4 - chewing muscle; 5 - lower jaw; 6 - medial pterygoid muscle; 7 - wall of the pharynx; 8 - deep layer of fascia of the parotid gland; 9 - styloid process; 10 - internal carotid artery; 11 - internal jugular vein; 12 - digastric muscle; 13 - sternocleidomastoid muscle. Rice. 3. Bed of the parotid gland: 1 - temporomandibular joint; 2 - external carotid artery; 3 - chewing muscle; 4 - septum between the parotid gland and the submandibular gland; 5 - submandibular gland; 6 - digastric muscle; 7 - sternocleidomastoid muscle; 8 - styloid process; 9 — wall of the external auditory canal; 10 - external auditory opening.
In front, the parotid gland is adjacent to the masticatory muscle (m. masseter), the branch of the lower jaw (r. mandibulae) and the medial pterygoid muscle (m. pterygoideus med.); at the back it borders with the sternocleidomastoid muscle (m. sternocleidomastoideus), the posterior belly of the digastric muscle (venter post m. digastrici) and the mastoid process (processus mastoideus); medially adjacent to the styloid process (processus styloideus) and the stylohyoid (m. stylohyoideus) and styloglossus (m. styloglossus) muscles, the internal carotid artery (a. carotis int.) and the internal jugular vein (v. jugularis) extending from it int.), hypoglossal nerve (n. hypoglossus) and peripharyngeal tissue; from above it adjoins the zygomatic arch (areus zygomaticus) and the external auditory canal (porus acusticus ext.). These formations limit the bed of the liver. (Fig. 2), which is lined by the fascia of the liver. (fascia parotidea). Fascia O. g. fused with the fascia of the surrounding muscles and attached to the edge of the lower jaw, zygomatic arch, mastoid and styloid processes. Between the angle of the lower jaw and the sternocleidomastoid muscle, the fascia forms a dense septum (Fig. 3), separating the O. from the submandibular gland (submandibular gland, T.; gl. submandibularis).
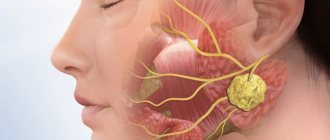
Rice. 4. Topography of the parotid gland: 1 - auriculotemporal nerve; 2 - superficial temporal arteries and vein; 3 - zygomatic arch; 4 - temporal branch of the facial nerve; 5 - zygomatic branch of the facial nerve; 6 - parotid duct; 7 - buccal branches of the facial nerve; 8 - facial arteries and vein; 9 - chewing muscle; 10 - marginal branch of the facial nerve; 11 - submandibular gland; 12 - cervical branch of the facial nerve; 13 - external carotid artery; 14 - subcutaneous muscle of the neck; 15 - internal jugular vein; 16 - sternocleidomastoid muscle; 17 - external jugular vein; 18 - v. retromandibularis; 19 - parotid gland; 20 - maxillary artery; 21— parotid plexus of the facial nerve; 22 - facial nerve; 23 - auricle; 24 - accessory parotid gland.
Through the thickness of O. zh. large vessels and nerves pass through; external carotid artery (a. carotis ext.) with the maxillary (a. maxillaris) and superficial temporal arteries (a. temporalis superficialis) branching off from it, v. retromandibularis, nerves auriculotemporal (n. auriculotemporalis) and facial (n. facialis). The facial nerve (see) forms the parotid plexus (plexus parotideus) in the thickness of the gland, the branches of which, leaving the gland, fan out to the facial muscles (Fig. 4). This determines the radial direction of the incisions of the gland during operations.
The system of excretory ducts of the gland is represented by intralobular, interlobular and interlobar ducts, which merge into the common parotid duct (ductus parotideus), or Stenon duct, which was first described by the Danish scientist N. Stenon in 1661. Length of the parotid duct 40-70 mm, its dia. 3-5 mm. The parotid duct usually originates from the upper third of the gland, bends around the edge of the masseter muscle and the fatty body of the cheek (corpus adiposum buccae) and opens into the vestibule of the mouth at the level of the upper second molar. In this place on the mucous membrane of the cheek there is a papilla of the liver. (papilla parotidea). According to S. N. Kasatkin (1948), in 44% of cases the parotid duct is ascending, in 23% - descending, less common are straight, cranked, arcuate (Fig. 1), S-shaped and bifurcated parotid duct. In half of the cases, the duct of the accessory parotid gland (glandula parotis accessoria) flows into it. Sometimes a blind canaliculus, the so-called, departs from the parotid duct near its mouth. Shievich's organ is a rudimentary salivary duct. The parotid duct contains valves and terminal siphons that regulate the excretion of saliva.
Blood supply is provided by the branches of the external carotid artery, superficial temporal artery, transverse artery of the face (a. transversa faciei), posterior and deep auricular arteries (aa. auriculares post, et profunda). Intraorgan arteries and veins pass through the interlobular septa. Venous drainage occurs into the pterygoid plexus (plexus pterygoideus) and the mandibular vein.
Lymphatic vessels of the lake. drain into the superficial and deep parotid lymph nodes (nodi lymphatici parotidei superficiales et profundi); their efferent vessels go to the superficial and deep cervical lymph nodes (nodi lymphatici cervicales superficiales et profundi).
Innervation is carried out by sympathetic and parasympathetic nerves. Preganglionic sympathetic fibers originate in the gray matter of the upper thoracic segments of the spinal cord and are interrupted in the superior cervical ganglion (gangl, cervicale sup.). Postganglionic sympathetic fibers go to the lake. as part of the external carotid plexus (plexus caroticus ext.). Sympathetic nerves constrict blood vessels and inhibit the secretion of saliva. The gland receives parasympathetic innervation from the lower salivary nucleus (nucleus salivatorius inf.) of the glossopharyngeus nerve. Preganglionic fibers go as part of this nerve and its branches (n. tympanicus, n. petrosus minor) to the ear ganglion (gangl, oticum). Postganglionic fibers reach the gland along the branches of the auriculotemporal nerve. Parasympathetic fibers stimulate secretion and dilate blood vessels.
X-ray anatomy
Sialography of the Parotid gland (see Sialography) in the anterior direct projection allows you to detect the shadow of the gland. outward from the branch of the lower jaw. In the lateral projection of the lake. projected onto the ramus of the mandible and the fossa retromandibularis area. The parotid duct on the sialogram in the lateral projection runs in an oblique direction from back to front and upward. Its intraglandular part crosses the posterior edge of the ramus of the lower jaw at the border of its middle and lower thirds or lies on the angle of the lower jaw. At the level of the anterior edge of the mandibular ramus, the duct emerges from the gland, and its extraglandular part is located at the base of the coronoid process of the mandible. Interlobar ducts of the lake. They merge into the parotid duct at different angles and have different numbers of branches. Depending on this, S. N. Kasatkin (1948) divides the glands into many branched, moderately branched and few branched.
Recommendations
- https://www.colgate.com/en-us/oral-health/basics/mouth-and-teeth-anatomy/submandibular-gland—location—function-and-complications
- ^ a b
Ibrahim, Dalia.
“Accessory parotid gland | Reference article on radiology". Radiopedia
. - ^ a b
Jacobs S. (2008).
"Chapter 7: Head and Neck". Human anatomy
. Elsevier. p. 193. Doi:10.1016 / B978-0-443-10373-5.50010-5. ISBN 978-0-443-10373-5. - ^ a b c d
Fehrenbach MJ, Herring SW (2012).
Illustrated Anatomy of the Head and Neck
(4th ed.). St. Louis, MO: Elsevier/Saunders. paragraph 154. ISBN 978-1-4377-2419-6. - "Parotid gland". TeachMeAntatomy.info
. Retrieved November 11, 2015. - Spratt JD, Abrahams PH, Boon JM, Hutchings RT (2008). McMinn's Clinical Atlas of Human Anatomy
(6th ed.). St. Louis, MO: Elsevier/Mosby. paragraph 54. ISBN 978-0-8089-2318-3. - ^ a b
Nancy A. (2013).
Ten Kate's Oral Histology: Development, Structure and Function
(8th ed.). St. Louis, MO: Elsevier. ISBN 978-0-323-07846-7. - ^ a b c
Bath-Balogh M, Fehrenbach MJ (2011).
Illustrated dental embryology, histology and anatomy
(3rd ed.). Elsevier. paragraph 135. ISBN 978-1-4377-1730-3. - Arhakis A., Karagiannis V., Kalfas S. (2013). "Salivary alpha-amylase activity and salivary flow rate in young adults." Journal of Open Dentistry
.
7
: 7–15. Doi:10.2174/1874210601307010007. PMC 3601341. PMID 23524385. - Moore P. (2003). The Developing Man
(7th ed.). Saunders. pp. 203, 220. ISBN 978-0-8089-2265-0. - ^ a b c d f g gram h i j k l m p o p
Wilson KF, Meyer JD, Ward Police Department (June 2014) “Diseases of the Salivary Glands.”
American family physician
.
89
(11):882–88. PMID 25077394. - Mehanna H, McQueen A, Robinson M, Paleri V (October 2012). "Swelling of the salivary glands." BMJ
.
345
:e6794. doi:10.1136/bmj.e6794. PMID 23092898. S2CID 373247. - ^ a b
Iro H, Zenk J (2014-12-01).
"Diseases of the salivary glands in children." GMS Current Topics in Otorhinolaryngology, Head and Neck Surgery
.
13
:Doc06. Doi:10.3205/cto000109. PMC 4273167. PMID 25587366. - ^ a b c d e
Bucur A, Dincă O, Niță T., Totan C, Vlădan C. (March 2011).
"Parotid tumors: our experience." Reverend Chir.
Oro-maxilo-fac. Implantol .
2
(1): 7–9.
ISSN 2069-3850.[ permanent dead link
](there is a translation button on the web page) - Sivaram P, Rahul M, Jayan K, Sulfekar MS. (2015). "Metastatic malignant phyllodes tumor: an interesting presentation as parotid edema." New Indian Journal of Surgery
.
6
(3): 75–77. Doi:10.21088/nijs.0976.4747.6315.2. ISSN 0976-4747. - Psychogios, Georgios; Bohr, Christopher; Konstantinidis, Yiannis; Kanis, Martin; Vander Porten, Vincent; Plzak, Jan; Knopf, Andreas; Betz, Christian; Guntinas-Licius, Orlando; Zenk, Johannes (2020-08-04). "A Review of Surgical Techniques and a Decision Guide for the Treatment of Benign Parotid Tumors." European Archives of Otolaryngology
. Doi:10.1007/s00405-020-06250's. ISSN 0937-4477. - Office of Rare Disease Research (2011). "Frey's syndrome." National Institutes of Health. Retrieved December 17, 2012.
- ^ a b c d f g gram h
Carlson ER, Ord RA (2015).
Pathology of the salivary glands: diagnosis and treatment
(Second ed.). Hoboken, NJ: Wiley/Blackwell. ISBN 978-1-118-93375-6. OCLC 904400135. - Sujatha D, Babita K, Prasad RS, Pai A (November 2013). "Parotid lymphoepithelial cysts in human immunodeficiency virus: a review". Journal of Laryngology and Otology
.
127
(11):1046–49. Doi:10.1017/S0022215113002417. PMID 24169222. - ^ a b c d f f
Anniko M., Bernal-Spreckelsen M., Bonkowski W., Bradley P., Jurato S., eds.
(2010). Otorhinolaryngology, Head and Neck Surgery
. Springer. ISBN 978-3-540-42940-1. - ^ a b
Shliev T, Kolokitas A, Miloro M (2015).
"Chapter 14: Wage Infections". In Hupp JR, Ferneini EM (eds). Head, neck and orofacial infections: a multidisciplinary approach
. p. 235. ISBN 978-0-323-28946-7. - Kumar B.S., Sathasivasubramanian S.P. (January 2012). "The role of salivary gland scintigraphy in detecting salivary gland dysfunction in patients with type 2 diabetes." Indian Journal of Nuclear Medicine
.
27
(1): 16–19. Doi:10.4103/0972-3919.108832. PMC 3628255. PMID 23599592. - "Scanning the function of the salivary glands." Johns Hopkins Sjogrens Center
. Received 2018-03-25.
Histology
The parotid gland has a lobular structure. Connective tissue septa extending from the fascia of the stomach divide its parenchyma into lobules, which in turn form 5-7 larger lobes.
Rice. 5. Schematic representation of the histological structure of the parotid gland. A - at a magnification of 200 times: 1 - intercalary duct; 2 - striated duct; 3 - terminal secretory department; 4—fat cell; 5 - interlobular duct; 6 - interlobular septum; 7 - blood vessel; hematoxylin-eosin staining; B - with a magnification of 600 times: 1 - fat cell; 2 - serocytes of the terminal secretory section; 3 - striated duct; 4 — myoepitheliocytes; 5 - intercalary duct; hematoxylin-eosin staining.
O.J. is a complex alveolar gland (see Glands). Its lobules are formed from terminal secretory sections tightly adjacent to each other - acini and excretory intralobular ducts: intercalated and striated (Fig. 5).
The terminal secretory sections are formed by glandular epithelial cells - serocytes, located on the basement membrane, consisting of a dense network of reticular fibers. The serocyte has a pyramidal shape, its cytoplasm contains a basally located rounded nucleus, a well-developed endoplasmic reticulum with numerous cisterns, a lamellar complex and secretory granules of various types.
In the terminal secretory sections of the lake. secretory tubules are distinguished, which are located between serocytes and have the appearance of thin tubes without their own walls.
Intercellular secretory tubules are characteristic of glands with protein secretion. The apical pole of serocytes, as well as their surface facing the intercellular secretory tubules, are covered with microvilli.
The terminal secretory sections pass further into narrow intercalary ducts lined with cuboidal epithelium, and then into striated ducts, or salivary tubes, lined with single-layer columnar epithelium. The characteristic basal striation of the epithelium of striated ducts depends on the accumulation of mitochondria lying between the folds of the plasmalemma of the basal part of the cell. It is believed that the striated ducts play a role in changing the concentration of primary saliva.
Between the cells and the basement membrane of the terminal secretory sections, intercalary and striated ducts there are myoepithelial cells, or basket cells, which are contractile elements that contribute to the secretion of secretions and maintaining the tone of the gland ducts.
Intralobular ducts pass into interlobular ducts, which run in layers of connective tissue between the lobules of the gland, merge with each other, forming interlobular ducts and, finally, the parotid duct. Interlobular ducts of the lake. lined with double-row prismatic epithelium, which, as the excretory ducts thicken, becomes multilayered. Along the parotid duct the epithelium is multilayered cubic, and at the mouth of the duct it is multilayered squamous.
Physiology
As an organ of the digestive system, the parotid gland, together with other salivary glands, secretes saliva into the oral cavity; its edges have a complex composition and perform various functions (see Saliva), exocrine (salivary) function of the o. performs starting from the 4th month of embryonic development. In this period, according to E. Sh. Gerlovin (1963), the secretion of O. zh. is mucous in nature, at the end of the 2nd year of life it becomes serous. The amount of saliva secreted is not constant and depends on the state of the internal environment of the body, the type and smell of food, the nature of irritation of specific receptors of the oral mucosa, etc. (see Salivation).
Cells of O. perform an excretory function, accumulating and removing various medicinal substances, poisons, toxins, and, in patients with diabetes, sugar from the body with saliva.
There is evidence indicating the endocrine function of the lake. Thus, biologically active substances (parotin, nerve growth factor, epithelial growth factor) were extracted from gland cells. Ito (I. Ito, I960) found that parotin has the properties of a hormone and affects protein and mineral metabolism. From O. zh. insulin-like protein is isolated. A histofunctional connection was revealed. with the reproductive, parathyroid, thyroid, pancreas, pituitary and adrenal glands.
Operations
To remove the cyst together with P. g. An incision is made in the sublingual area. When isolating a cyst and gland, it is necessary to insert a probe or catheter into the duct of the submandibular gland to avoid injury to it. Isolation of pancreas. should start from the distal pole. In cases where part of the cyst is localized below the mylohyoid muscle, B. D. Kabakov proposed performing the operation in two stages. At the first stage, after dissecting the tissue in the submandibular or submental region, the cyst shell is isolated to its narrowed part at the mylohyoid muscle. This isthmus (the narrow part of the cyst) is ligated and divided. The part of the cyst separated from the surrounding tissue is removed. The wound is sutured in layers, leaving a small opening. At the second stage, the cyst is opened from the bottom of the mouth, widely excising the mucous membrane of the sublingual region covering the cyst, as well as the membrane of the cyst. After this, the cyst wall is sutured with knotted sutures to the edges of the mucous membrane of the sublingual region. The cyst cavity is packed.
See also Salivary glands.
Bibliography:
Kasatkin S.N. Anatomy of the salivary glands, Stalingrad, 1948; Guide to surgical dentistry, ed. A. I. Evdokimova, p. 226, M., 1972, bibliogr.; Sazama L. Diseases of the salivary glands, trans. from Czech., Prague, 1971, bibliogr.; Solntsev A. M. and Kolesov V. S. Surgery of the salivary glands, Kyiv, 1979, bibliogr.; Rauch S. Die Speicheldrusen des Menschen, Stuttgart, 1959.
I. F. Romacheva; V. S. Speransky (an., hist.).
Research methods
When identifying pathology of the Parotid gland, questioning and examining the patient, palpation of the liver are of great importance, which allow us to make an assumption about a particular disease of the bladder. (inflammation, tumor, damage, etc.).
Laboratory, instrumental, and X-ray radiological methods play a significant role in clarifying the diagnosis. research.
Probing of the parotid duct allows one to determine its patency and the presence of dense foreign bodies in it.
Cytological examination of the secretion of the gland, as well as puncture biopsy with histol, examination of organ tissues help to identify morphological changes in the gland, in particular in the presence of a tumor.
Secretory function of the lake. studied using sialometry (measurement of the amount of saliva released per unit of time), as well as radioisotope methods—radiosialography and radiosialometry, based on the ability of the parenchyma of the liver. concentrate and release radioactive isotopes 131I, 99Tc with saliva.
To determine foreign bodies and morphol, changes in the structure of the ducts and parenchyma of the lake. (chron, inflammation, tumor) X-rays of the gland are performed without contrast and with contrast of the ducts (see Sialography).
Layer-by-layer images of the organ are obtained using tomography (see), and the use of panoramic tomography (see Pantomography) makes it possible to simultaneously examine and compare the right and left O.
Ultrasonic dowsing (see Ultrasound diagnostics) is a method for diagnosing tumor processes in the liver. and, in addition, allows one to judge the size of the gland and the degree of sclerosis of its parenchyma.
Scanning of the body. using 99Tc (see Scanning) allows you to visualize the parenchyma of the gland, identify the localization of its non-functioning areas, which is also an indirect sign of a violation of its function.
Thermal imaging (see Thermography) is carried out to measure the temperature in the tissues of the body. An increase in the cut is a sign of acute inflammation, a malignant tumor, Sjögren's syndrome, and a decrease is a sign of a benign tumor, cystic formations, certain forms of hron, mumps and etc.
Pathology
Patol, processes in P. zh. similar to those with damage to other salivary glands. On patol, the condition of the gland is indicated by an increase in sublingual folds, painful in acute inflammation, painless in chronic inflammation, dense consistency in tumors and soft consistency in pancreatic cysts.
Damage
P.J. are relatively rare. In case of a gunshot wound, they are usually combined with damage to the bones of the facial skull. In addition, there are cases of damage to the pancreas. disc during the preparation of lower jaw teeth for crowns, during surgery for acute inflammatory processes in the sublingual region, when removing salivary stone (see Sialolithiasis) from the middle or posterior sections of the submandibular duct. Damage to the gland can be diagnosed by examining the wound, in which the glandular tissue can be clearly visible. Patients are bothered by pain when talking or eating. As a result of scarring of the wound, the outflow of secretions from the ducts of the pancreas. may be disrupted, which leads to the appearance of a ranula - a retention cyst (see Cyst).
Diseases
P.J. include reactive-dystrophic processes, acute and chronic inflammation, cysts, tumors (see Salivary glands).
Reactive-dystrophic diseases are usually not an isolated lesion of the pancreas: they develop with systemic damage to the salivary and lacrimal glands - Mikulicz's disease (see Mikulicz syndrome), all excretory glands - Sjögren's syndrome (see Sjögren's syndrome), as well as other autoimmune and endocrine diseases (see Salivary glands). P.J. At the same time, it increases in size, becomes denser, and subsequently a decrease in its function is observed.
Rice. 2. Sublingual area with acute inflammation of the sublingual salivary glands: sublingual folds of uneven thickness (indicated by arrows), the mucous membrane of the sublingual area is swollen. Rice. 3. Sublingual area with chronic inflammation of the sublingual salivary glands: 1 - tongue, 2 - frenulum of the tongue, 3 - thickened, raised sublingual folds, 4 - tuberous surface of the right sublingual gland.
Inflammation of the pancreas. can be acute or chronic. The cause of acute infection can be mumps viruses with an atypical course (see Epidemic mumps), influenza (see), etc. The disease begins acutely and is accompanied by an increase in body temperature. The gland is enlarged in size, sharply compacted on palpation, and painful. The sublingual folds are thickened, the oral mucosa is swollen (Fig. 2). These phenomena persist for 4-5 days, then the infiltrate slowly resolves and the condition returns to normal. On the 2-3rd day of the disease, an abscess may develop. Treatment is conservative, in case of an abscess - surgical. Chron, inflammation of the pancreas. is observed relatively rarely, is usually bilateral and is combined with damage to the parotid or submandibular salivary glands (see Parotid gland, Submandibular gland). Clinically manifested by swelling of the pancreas. If left untreated, the gland slowly enlarges, thickens, and becomes lumpy (Fig. 3). Pain appears only when the process worsens. Treatment includes general measures aimed at increasing the body's resistance; novocaine blockade is applied locally. In addition, treatment of concomitant diseases is necessary.
The most common patol, process in P. g. is a retention cyst, which occurs when the outflow of secretions from the pancreas is disrupted. The shell of the cyst consists of connective tissue rich in blood vessels, the bundles penetrate into the connective tissue layers of the lobules of the pancreas. In the peripheral parts of the cyst shell there are elongated cells such as fibroblasts; very rarely one or two rows of cubic or multirow cylindrical epithelium cells are found on the inner surface of the cyst shell. The first wedge, a symptom of a cyst, is the appearance of swelling in the sublingual area (painless, soft or elastic consistency), the edges, slowly increasing, can spread to the submandibular area. When the mucous membrane of the floor of the mouth in the sublingual region becomes thinner, spontaneous opening of the cyst and its emptying may occur. In this case, it decreases in size or is not detected at all, but after a certain time (weeks, months) it reappears and increases. Treatment of the cyst is surgical: a cystotomy is performed (opening the cyst and emptying) or the cyst is removed along with the pancreas.