If you go to the mirror and open your mouth wide, you can see two formations that are located on the side surfaces, in the depths of the pharynx, which are shaped like an almond. This is why the tonsils are called tonsils. And since the tonsils are located in the soft palate, they are called palatine tonsils.
Also, in common parlance, the palatine tonsils are also called tonsils. They are one of the important organs of the pharyngeal immune system and form an important part of the Pirogov-Waldeer lymph-epithelial pharyngeal ring.
Palatine tonsil, tonsila palatina. It is located in the tonsillar fossa between the palatoglossus and velopharyngeal arches.
Make an appointment right now!
Call us by phone or use the feedback form
Sign up
What other tonsils are there in the pharynx?
Other tonsils that form the lymphoid pharyngeal ring are: adenoid vegetations, or, more simply, adenoids, which are not a paired organ. They are located in the dome of the nasopharynx. It is impossible to see them with the naked eye. In order to recognize the condition of the adenoids, it is necessary to perform an endoscopic examination of the nasopharynx. Inflammation of the adenoids is called adenoiditis and is more common in children.
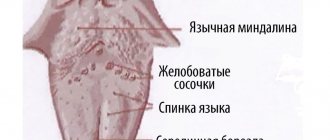
Also in the pharynx there is a lingual tonsil, located at the root of the tongue, which, like the adenoids, is an unpaired organ.
There are also tubal ridges, which are also called tubal tonsils. They are located at the entrance to the pharyngeal mouth of the auditory tube. The tube ridges are located deep in the nasopharynx, on the lateral (medial) surfaces of the nasopharynx on the right and left. Tubal tonsils perform an important function - they protect against infection entering the auditory tube. Since each of the tonsils of the lymphoepithelial pharyngeal ring deserves separate close attention, in this article we will only talk about the palatine tonsils and chronic tonsillitis. Other tonsils and the pathology they cause will be described in detail separately, in other relevant ENT articles.
Read more about tonsils
It must be said that the palatine tonsils are the largest lymphoid formations of the entire pharyngeal ring, and they play, perhaps, the leading role in the disposal of bacterial and viral infections that enter the pharynx by airborne droplets.
Due to their size, the palatine tonsils are the first to stand in the way of microbes that enter the oral cavity from the external environment, and protect the body from infection by viruses, bacteria, spirochetes, protozoa and other microorganisms.
The palatine tonsils have depressions - lacunae, which in turn are exit holes for deep and sharply convoluted canals - crypts, which are located in the thickness of the palatine tonsil, leading to its root. The number of lacunae and crypts can vary from 1 to 14, but on average, in each amygdala there are from 4 to 7 lacunae. The diameter of the lacunae can also vary, depending on gender, age, individual characteristics of the patient, as well as the duration and severity of the disease and the presence of scar changes in the tonsils themselves.
It is believed that the wider the exit hole - the lacuna - the higher the likelihood of the palatine tonsil to self-cleanse. This statement is true. Accordingly, the smaller the diameter of the lacuna, the more pronounced and severe the tonsillitis. Moreover, if the tonsil produces a large amount of caseous-necrotic detritus (plugs), the severity of the course also noticeably increases.
Normally, on the mucous membrane of the palatine tonsils, as well as in the thickness of the palatine tonsils, in the lacunae and crypts, there is a growth of non-pathogenic and conditionally pathogenic microflora, in normal (permissible) concentrations. If there are more microorganisms (for example, due to intensive growth, or the addition of other pathogenic microflora from the outside), the palatine tonsil immediately destroys and utilizes the dangerous infection and normalizes a dangerous condition for the body. At the same time, the macroorganism, that is, the person, does not notice this in any way.
The tissues of the palatine tonsils produce the following main protective substances: lymphocytes, interferon and gamma globulin.
The palatine tonsils act as a serious infectious and inflammatory barrier and are an important component in creating not only local, but also general immunity in the human body. Therefore, when it comes to removing the palatine tonsils, you first need to think ten times, weigh the pros and cons, and only after that make a decision about removing the tonsils.
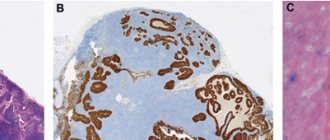
Histology
Rice.
4. Diagram of the structure of the palatine tonsil: 1 - capsule; 2 - tonsil crossbars; 3 - lymphatic follicles of the tonsil; 4 - tonsil parenchyma; 5 - multi-row squamous epithelium of the pharynx surface of the tonsil, continuing into the crypts; 6—exit openings of tonsil crypts. M. consist of stroma and parenchyma (Fig. 4). The stroma forms the connective tissue framework of M., formed by collagen and elastic fibers. They form a capsule (shell) around the M.’s circumference, from which connective tissue crossbars (trabeculae) extend into the M.’s depth. In the thickness of the crossbars there are blood and lymphatic vessels and nerves of the M., and sometimes the secretory sections of small salivary glands. M.'s parenchyma is represented by lymphoid tissue (see), the cellular basis of the cut is lymphocytes, macrophages, and plasma cells. Elements of lymphoid tissue form in places round-shaped clusters—follicles, which are located parallel to the epithelium along the free surface of the tumor and along the crypts. The centers of the follicles can be light - the so-called. reproduction centers, or reactive centers. The free surface of the M. is covered with a mucous membrane with multi-row squamous non-keratinized epithelium. In the area of the crypts it is thinner and in places broken; the basement membrane is also fragmented, which contributes to better contact of the lymphoid tissue with the environment.
Chronic tonsillitis
Chronic tonsillitis is an autoimmune disease that occurs as a result of frequent sore throats and a decrease in the body’s overall resistance since childhood. With the development of the disease and its exacerbation, a person does not have enough general immunity to keep the palatine tonsils “in working order” and adequately fight the infection.
If harmful microbes get onto the surface of the mucous membrane and into the lacunae of the palatine tonsil, a real battle occurs between the microbes and the human immune system.
The palatine tonsil fights all pathogenic and conditionally pathogenic infections, but not being able to fully resist attacking microbes, it provokes either a new outbreak of sore throat or an exacerbation of chronic tonsillitis (treatment cannot be delayed in any case), thereby triggering an infectious-inflammatory process in palatine tonsils.
As a result of a lost fight, pus accumulates and stagnates in the lacunae of the tonsils, that is, dead leukocytes that come to the aid of the tonsil in the fight against a dangerous infection. The purulent masses irritate and inflame the tonsil tissue from the inside and have a toxic effect on it, thereby causing a sore throat - a severe infectious outbreak of inflammation of the tonsils.
In the absence of quick and adequate treatment, the contents of the lacunae and crypts of the palatine tonsils serve as a breeding ground for pathogenic microbes and a constant source of infection, even after an attack of tonsillitis.
Forms of the disease
- recurrent form, that is, with frequently recurring sore throats;
- protracted form, when the inflammatory process in the palatine tonsils is characterized by a sluggish and prolonged course;
- compensated form, when episodes of sore throat and exacerbation of tonsillitis are not observed for a long time.
Chronic tonsillitis is the most common disease among all diseases of the pharynx and one of the most common diseases of all ENT organs, along with such a diagnosis as acute sinusitis.
Chronic tonsillitis can affect both adults and children, from the moment the palatine tonsils begin to develop (from 2-3 years). Moreover, the incidence of this disease in childhood is much higher.
Some respiratory diseases can also be classified as social diseases. For example, sinusitis and tonsillitis are among them. Poor environment, stress, lack of sleep, overwork, monotonous and poor nutrition, as well as poor heredity are predisposing factors to the development of the disease.
Contraindications
They can be absolute (excluding the possibility of tonsillectomy) and relative, when everything is postponed until the reasons preventing the operation are eliminated.
Absolute contraindications:
- diseases with increased bleeding: hemophilia, hemorrhagic diathesis, Werlhof's disease, agranulocytosis, leukemia;
- heart failure grade 2–3;
- acute infectious diseases and exacerbation of chronic ones;
- active form of tuberculosis;
- cirrhosis of the liver.
Relative contraindications:
- caries (before sanitation - dental prophylaxis of the oral cavity);
- inflammation of the gums;
- pustular diseases of the mouth and skin;
- ARVI and influenza;
- exacerbation (decompensation) of chronic diseases;
- menstruation;
- pregnancy after the 26th week due to the risk of premature birth.
Causes
The development of the disease is closely related to frequent sore throats (acute tonsillitis). Very often, incompletely cured tonsillitis leads to chronic tonsillitis. Very often, tonsillitis is an exacerbation due to the accumulation of plugs in the tonsils - caseous-necrotic masses, which are often confused with food debris.
Main reasons for development
- Unfavorable working conditions. The greatest influence is exerted by gas and dust levels in the air at work.
- Poor environmental conditions, pollution from vehicle exhaust gases, harmful emissions into the atmosphere.
- Low quality of consumed water.
- Weak (low) immunity.
- Severe hypothermia of the body.
- Stressful situations.
- The presence of chronic diseases in the nasal cavity, paranasal sinuses and oral cavity - dental caries, purulent sinusitis, etc., which often leads to infection of the tonsils.
- Irrational or poor nutrition, in which excess amounts of proteins and carbohydrates are consumed.
- Heredity (mother or father suffers from chronic tonsillitis). It is very important for a woman to undergo one or two courses of treatment for tonsillitis during pregnancy (depending on the severity of the process) in order to minimize the likelihood of the disease developing in the unborn child.
- Frequent overwork, fatigue syndrome, inability to fully rest.
- Smoking and alcohol abuse.
Risk factors
The main risk factors for developing tonsil cancer include:
- smoking and chewing tobacco use;
- frequent alcohol consumption (if a person smokes and drinks a lot of alcohol, the risk increases even more);
- infection caused by human papillomaviruses (HPV), especially types 16 and 18;
- therapy with immunosuppressive drugs after organ transplantation;
- HIV infection.
It is known that malignant tumors of the tonsils caused by HPV usually occur at a younger age and respond better to treatment.
Symptoms
How to independently recognize chronic tonsillitis? Symptoms and treatment in adults and children can only be correctly determined by an ENT doctor. Below are characteristic signs - if you find them in yourself, consult a doctor.
The disease is characterized by symptoms such as:
- Headache.
- Feeling of something foreign in the throat, as if something was stuck in the throat. In fact, this is nothing more than large accumulations of caseous masses, that is, plugs in the thickness of the palatine tonsils.
- Increased fatigue, weakness, decreased performance. All this is due to the so-called tonsillogenic intoxication, or in other words, intoxication syndrome.
- Aching pain in the joints and muscles (with severe illness).
- Aching pain in the heart, with interruptions in heart function - extrasystole (with severe illness).
- Pain in the lower back, in the kidney area (with severe disease).
- Bad mood, and in some cases increased body temperature, and for a long time.
- Persistent skin rashes, provided that there was no previous skin pathology.
All these symptoms appear due to the entry of waste products of microorganisms into the blood from the palatine tonsils, i.e. staphylococcal and streptococcal infections, poisoning the entire body.
Bad breath appears due to the accumulation of organic substances and the decomposition of bacterial infection in the lacunae (recesses of the tonsils) and crypts (their canals). Tonsils become a source of bacterial infection, which can spread throughout almost the entire body and cause inflammation of the joints, myocardium, kidneys, paranasal sinuses, prostatitis, cystitis, acne and other diseases.
If the tonsils do not cope with their function as an immune organ, then even slight overwork, stress, or mild hypothermia can significantly reduce the immune defense and open the way for microbes and exacerbation of the disease.
Early stages of infection
Juvenile formations on the tonsils have different causes, but if there is a conclusion that the child has been diagnosed with the papilloma virus, this requires parents to constantly monitor and pay attention to their health status. Specialists from the first children's medical center in Saratov will help you decide on the most effective preventive and therapeutic measures. If your child often coughs for no apparent reason, or says that he has an uncomfortable sensation of the presence of a foreign object in his throat, immediately sign up for a consultation and visit a specialist who will select the most appropriate and effective treatment.
Complications
Chronic tonsillitis is very dangerous due to rapidly occurring complications. The most severe of them are heart disease - myocarditis, inflammation of the joints - rheumatism and serious kidney damage - glomerulonephritis.
Some toxins that are produced by microbes in the tonsils and then enter the bloodstream can damage cartilage and ligament tissue. The result is inflammation and pain in the muscles and joints. Other toxins often cause persistent fever, changes in blood tests, fatigue, depression, and severe headaches.
Chronic tonsillitis can affect the functioning of such a vital organ as the heart. The tonsils are often parasitized by group A beta-hemolytic streptococcus, the protein of which is very similar to the protein found in the connective tissue of the heart. Because of this, the immune system can show retaliatory aggression not only to the emerging streptococcus, but also to its own heart. As a result, heart rhythm disturbances, heart valve prolapses, and even the development of severe myocarditis and bacterial endocarditis occur.
For the same reason, articular surfaces and kidney tissue are at great risk. Unfortunately, the development of diseases such as rheumatoid arthritis and glomerulonephritis is extremely high.
Due to the fact that the source of infection remains in the tonsils for a long time, a distortion of the body’s reactivity occurs, resulting in allergic changes. In some cases, just one course prescribed by a doctor can get rid of itching and allergic rashes, and in some cases stop the development of bronchial asthma attacks.
Diagnostic methods
During the initial appointment, the doctor examines the throat, identifies an enlarged tonsil, and evaluates its appearance. The doctor examines the nasal cavity, outer ear, and palpates (feeling) the lymph nodes in the neck. If, based on the results of the examination, there is a suspicion of a malignant tumor, then a biopsy is performed. A thin needle connected to a syringe is inserted into the tonsil, and cells are removed from the tumor by pulling the piston. This procedure is called a needle aspiration biopsy. The resulting material is sent to the laboratory to be examined under a microscope for the presence of malignant cells.
After the malignant nature of the neoplasm is confirmed by the results of a biopsy, an examination is carried out to assess the extent of the spread of cancer in the body, clarify the stage and correctly plan treatment.
Diagnostic methods that may include examination:
- Computed tomography , magnetic resonance imaging.
- Orthopantomography is a special type of radiography of the skull bones, when in the picture they seem to “unfold” into one plane. This test is often performed by dentists. For tonsil cancer, it helps determine whether the malignant tumor has invaded the bone of the upper or lower jaw.
- PET/CT scanning is the “gold standard” in the search for metastatic foci. The patient is injected with a safe radiopharmaceutical that accumulates in cancerous areas. Then the images are taken using a special device (PET scanner). Thanks to the radiopharmaceutical, all tumor foci are well contrasted in the images. To more accurately assess the location of tumors, images obtained using PET scans are superimposed on CT images.
An analysis for human papillomaviruses is performed. This is important, since treatment tactics may depend on the HPV status. The virus itself, after infection, remains in the body for the rest of its life. There is no way to get rid of it; there are no effective antiviral drugs to treat this infection.
Chronic tonsillitis during pregnancy
It is very important to pay attention to the disease during pregnancy. When planning a pregnancy, even in the case of a compensated condition, that is, a condition outside of an exacerbation of tonsillitis, it is highly advisable to carry out a planned course as prescribed by a doctor. This will reduce the bacterial load on the entire body in general and on the palatine tonsils in particular.
It is very encouraging that doctors are now referring pregnant women and women who are just preparing for pregnancy for treatment of tonsillitis. Unfortunately, in some cases one of the reasons for not carrying a pregnancy to term is this disease, although at first glance it is hard to believe, tonsillitis is a traffic jam, the treatment of which and other manifestations may seem in no way related to pregnancy.
Before conceiving a child, it would be correct to examine the future father of the child for the disease and, if necessary, treat it as well. This will significantly reduce the risk of developing chronic tonsillitis in the unborn child. And, on the contrary, the worse the condition of the future father and especially the mother, the risk of developing the disease in the child increases many times over.
Before pregnancy, it is very important to carry out comprehensive treatment of the symptoms of chronic tonsillitis. But even during pregnancy, it is recommended to repeat the course, preferably in the second trimester, when the woman’s condition is perhaps the most comfortable. It is important to note that physiotherapeutic procedures cannot be carried out during pregnancy, but it is highly desirable to wash the palatine tonsils using a vacuum method, followed by treatment with antiseptic solutions.
Determination of stage
Determination of the stage of cancer is carried out according to the TNM system (T - tumor, N - nodulus, M - metastasis), including the size of the primary tumor, the spread of tumor cells to regional (located next to the primary tumor) lymph nodes and to distant areas (lungs, liver) . Today, the Russian Federation has adopted the seventh classification of tumors (the newest is the eighth). The connection between tonsil cancer and HPV infection is also taken into account during staging (but only for the eighth classification) - with similar morphological data of the tumor and its distribution, the stage of tonsil cancer associated with HPV infection is often lower, in contrast to cancer associated with other factors . In general, the prognosis for tonsil cancer associated with HPV infection is more favorable.
Tonsil cancer staging based on tumor size is “T”. headandneckcancerguide.org
The right approach
Sore throat, tonsillitis - treatment in children and adults is important to carry out immediately for all diseases of the oral cavity and nasopharynx that bother you. If breathing through the nose is impaired, and mucus or mucopurulent discharge flows down the back wall of the pharynx, then these symptoms should be given special attention.
Chronic tonsillitis - treatment (effective) can be conservative and surgical. Due to the fact that the removal of tonsils can cause serious harm to the defenses and immunity of the human body, otolaryngologists should try their best to preserve the tonsils and restore their functions without resorting to surgery to remove the tonsils. Modern methods of treating tonsillitis provide a greater chance of recovery without intervention.
Friends! Timely and correct treatment will ensure you a speedy recovery!
Chronic purulent tonsillitis - treatment of a conservative type must always be carried out in an ENT clinic, performing a complex, pathogenetically based course of treatment, as well as using a medicinal approach - medications prescribed by an ENT doctor.
Difference from tonsillotomy
Along with tonsillectomy, there is another operation with a similar name - tonsillotomy, in which enlarged tonsils are removed not entirely, but partially (usually in children). The indication for such an operation is the hypertrophy of these tonsils, when they occupy the entire space from the anterior palatine arch to the midline of the pharynx. With tonsillotomy, only the “excess” of enlarged tonsils is removed, returning them to normal size. Tonsillotomy is less traumatic than radical removal of the tonsils, and allows you to preserve their protective functions.
A complex approach
First stage
Viral tonsillitis - treatment with a good and pronounced effect is obtained by washing the lacunae of the palatine tonsils. There are two ways to wash the tonsils.
A very old method is to rinse the tonsils with a syringe. Previously, this method was widely used, but today it is used for lack of a better one or when the patient’s gag reflex is very pronounced.
The disadvantages of this method are that during the process of washing the palatine tonsils, the pressure created by the syringe is not sufficient to effectively wash out caseous masses from the lacunae of the tonsils. Also, this technique is contact and traumatic, since when using a straightened attic needle, its thin and sharp end can prick the inner surface of the palatine tonsil, namely the crypts - the channels into which the needle enters. Also, the tip from the set with a syringe is used for rinsing the tonsils and injecting into the larynx. On the contrary, it is very wide in diameter and injures the tonsil tissue when inserting the tip into the lacuna, or in general, due to the large outer diameter, it cannot always get there.
Practice has shown that today, the best results are achieved by the approach when the ENT uses the Tonsilor attachment.
First, it is necessary to rinse the lacunae of the palatine tonsils with a modified attachment of the Tonsilor apparatus with a transparent antiseptic solution, for example, saline solution (also known as isotonic sodium chloride solution). This is necessary so that the doctor can clearly see what he is washing out of the palatine tonsils.
Second phase.
Since the tonsils are washed from pathological secretions, it is necessary to immediately influence the tissues of the palatine tonsils with low-frequency ultrasound. At the same time, a medicinal solution passes through the ultrasonic tip of the “Tonsilor” apparatus, which, due to the ultrasonic effect of cavitation, turns into a finely dispersed medicinal suspension, which, due to hydraulic shock, hits the tissues of the palatine tonsil and the posterior wall of the pharynx with force and impregnates the medicinal solution into the submucosal layer of the tonsil.
The procedure for exposure to ultrasound is correctly called: Ultrasonic medicinal irrigation. In our clinic we use a 0.01% solution of Miramistin. This drug is good because it does not lose its properties under the influence of ultrasound. Miramistin is a very strong antiseptic drug, and ultrasound exposure further enhances the durability of the physiotherapeutic effect.
Third stage.
It is necessary to treat (lubricate) the palatine tonsils with Lugol's solution, which is also a strong antiseptic based on iodine and glycerin.
Fourth stage.
The otorhinolaryngologist at our clinic conducts a laser therapy session on the tissue of the palatine tonsils and the mucous membrane of the posterior pharyngeal wall. Laser treatment of tonsillitis in adults is very effective. Its action is aimed at reducing swelling and inflammation of the tissues of the palatine tonsils.
The laser radiation source can be installed in the oral cavity and acted in close proximity to the palatine tonsils and the mucous membrane of the posterior pharyngeal wall, thereby achieving the best results.
You can also install the laser emitter on the skin of the anterolateral surface of the neck in the projection of the location of the palatine tonsils and the posterior wall of the pharynx.
Fifth stage.
It is recommended to conduct sessions of vibroacoustic influence. They are carried out with the aim of normalizing microcirculation in the tissues of the palatine tonsils and improving the trophism (nutritional function) of the palatine tonsils themselves.
Sixth stage.
Effectively sanitize the microflora located on the surface of the palatine tonsils using ultraviolet irradiation (UVR).
This method has long been known, has proven itself very well and is still in service in many city (especially children's) clinics.
In this case, it is necessary to approach courses. The number of procedures in each specific case is determined individually at the first consultation with an ENT specialist. But for a lasting effect to occur, at least five sessions must be performed. If, during the fifth procedure, caseous and mucous masses are still washed out of the lacunae of the palatine tonsils, rinsing and other procedures must be continued “until clean rinsing waters”. As a rule, the number of ENT procedures does not exceed 10 treatment sessions.
After a full course, the lacunae of the palatine tonsils restore their ability to cleanse themselves, and the patient feels much better and more energetic.
In order to have a lasting result, it is necessary to carry out conservative treatment 2 to 4 times a year, as well as independently once every 3 months, take homeopathic and antiseptic medications.
In this case, you will most likely be able to avoid exacerbations of this disease and the need to remove the tonsils.
If, 2-4 weeks after the end of the course, caseous detritus again begins to accumulate in the thickness of the palatine tonsils, and the patient’s ENT complaints begin to bother them, as before the start of the course, conservative treatment of chronic tonsillitis in children and adults is considered ineffective. In this case, the patient is asked to consider the option of surgical removal of the tonsils. But fortunately, such an outcome (result) is quite rare.
Drug treatment of chronic tonsillitis
Dear patients! In this article I will describe only general principles and approaches.
More precise treatment will be offered to you at the initial ENT consultation, where an accurate diagnosis, form and degree of the disease will be made, as well as an optimal recovery plan will be proposed and a prognosis for the duration of remission will be given.
So:
- Antibacterial approach. Antibiotic therapy is important and necessary. But the decision to prescribe antibacterial drugs is made individually and only after a visual examination.
Antibiotics can be either light, prescribed for a short course and have no effect on the mucous membrane of the gastrointestinal tract, or heavy, which must be prescribed under the guise of probiotic medications. The choice of antibiotic depends on the severity of chronic tonsillitis and the microflora that supports this condition. - Probiotic treatment is prescribed in case of taking aggressive antibiotics, as well as in the presence of concomitant gastritis, duodenitis, reflux esophagitis.
- Antiseptic approach. Antiseptic sprays, aerosols, and rinses also give a very good effect and are therefore mandatory in the fight against chronic tonsillitis. I prefer a 0.01% solution of Miramistin, a 1% solution of Dioxidine (1 ampoule diluted - 10 ml + 100 ml of boiled warm water) and Octenisept, which must be diluted with boiled warm water or saline in a dilution of 1:5 , or 1:6.
- Decongestant (desensitizing) therapy is mandatory. It is needed to relieve swelling of the palatine tonsils and the surrounding tissue, as well as the mucous membrane of the posterior pharyngeal wall. This is also necessary for better absorption of all medications used. Such modern medications as Cetrin, Claritin, Telfast can cope with these tasks. But if a certain desensitizing drug helps you for a long time, you should not change it to another.
- Immunostimulating therapy. Here I want to draw your attention to the fact that the doctor prescribes drugs that stimulate the immune system. These drugs should not be confused with immunomodulators, which are strictly prescribed by an immunologist based on the results of a blood test. There are not so many drugs that stimulate local immunity at the level of the palatine tonsils and the mucous membrane of the posterior pharyngeal wall. Of the well-known drugs, Imudon comes first. The course must be at least 10 days. You need to take (dissolve) Imudon 1 tablet 4 times a day.
- Homeopathic treatment. In addition to conventional drug therapy of a chemical nature, it is necessary to take homeopathic medications that improve the trophism and, as a result, the nutritional function of the palatine tonsils. The drugs of choice may be tonsillotren and tonsilgon, as well as rinses, steam and ultrasonic inhalations with infusions and herbs: propolis, string, sage, chamomile and some other herbs.
- Emollient therapy is used symptomatically, when, against the background of exacerbation of tonsillitis, as well as taking medications, there may be dryness, rawness and soreness in the throat. In such cases, you can use peach oil, which must be instilled a few drops into the nose, throwing back the head. You can rinse your mouth with 3% hydrogen peroxide (VERY IMPORTANT! 6% and 9% hydrogen peroxide CANNOT be used!!!). To do this, you need to pour half a bottle of peroxide (10 ml) into a cup, put it in your mouth and rinse the entire solution once, for as long as possible. Then the solution is spat out and rinsed from foam and bitterness with warm boiled water. After gargling with hydrogen peroxide, you will feel a significant softening and comfort in your throat. You can gargle twice a day, but no more.
- Analgesic therapy is used if necessary, as symptomatic therapy, depending on the severity of the pain syndrome. Of the tablet forms, it is better to give preference to Nurofen or Ketanal and its derivatives: Ketarol, Ketalar, Ketanof, Ketanal.
- Diet therapy. Nutrition also plays a significant role in recovery. It is necessary to limit the intake of spicy, fried, sour, salty and peppery foods. During treatment, you should exclude hard foods from your diet. It is also recommended to protect yourself from very hot and very cold foods. Drinking alcohol, especially strong alcohol, is also contraindicated.
Surgical removal of tonsils
If we talk about the removal of the tonsils, then the operation to completely remove the tonsil tissue is called a bilateral tonsillectomy.
Partial removal of the tonsils is called a bilateral tonsillotomy.
It is extremely rare that the palatine tonsil is removed routinely on one side. There is also a practice of a number of hospitals (they like to do this in the Pirogov City Clinical Hospital No. 1) of removing the palatine tonsil or tonsils in case of a paratosillar abscess. This operation is called abscessonsillectomy. But it must be remembered that against the background of severe pain caused by an abscess, removal of the tonsil is extremely painful. Due to the purulent process, it is impossible to provide adequate anesthesia. Therefore, it is necessary to anesthetize the peri-almond tissue only with strong anesthetics: Ultracaine and Ultracaine DS-forte.
Routinely, palatine tonsils can be removed under local anesthesia or general anesthesia. Previously, this operation was performed only under local anesthesia.
Fortunately, there is now modern equipment that allows removal of palatine tonsils under general anesthesia or under anesthesia using cold plasma coagulation - Coblator.
Prevention of chronic tonsillitis
- Drug therapy
. If an ENT patient undergoes treatment courses in the clinic once every 6 months, then in addition to six-month procedures, he is recommended to take the drug Tonsilotren, with a frequency of once every 3 months, i.e. 4 times a year. The course of taking (resorption) of the drug is for 2 weeks (more precisely 15 days). It is also possible to instill 0.01% Miramistin solution, 4 pumps 4 times a day for 2 weeks, in courses 4 times a year. - Climatotherapy and spa therapy
. An important point in the prevention of chronic tonsillitis is visiting seaside resorts. Sunbathing, humidified sea air, swimming and, as a result, the inevitable entry of sea water into the mouth have a beneficial effect on the prevention of chronic tonsillitis. - Work and rest schedule
. In order for the periods of remission to be long, it is necessary to fully rest and not expose yourself to stress. It is not without reason that chronic tonsillitis, like sinusitis, is classified as a social disease, in which the more stress and workload there is at work, the higher the likelihood of exacerbation of chronic tonsillitis. - Diet
. It is very important to eat right. Under no circumstances should you get carried away with fried, salty, peppery, sour, bitter, i.e. that food that irritates the mucous membrane of the back of the throat and palatine tonsils. Citrus fruits are contraindicated. The consumption of alcoholic beverages, especially strong ones, is also contraindicated. It is not advisable to eat very hot and very cold and solid foods.
Forecast
The prognosis for patients with HPV-associated tonsil cancer is significantly better than for patients with other etiologies of cancer. It is impossible to predict with high accuracy the life expectancy of a particular patient, but there are average graphs that can be used to determine what percentage of patients with a certain stage are alive after n years: for example, almost 90% of patients with stage I HPV-associated oropharyngeal cancer are alive 4 years after diagnosis, while for HPV-unassociated oropharyngeal cancer at the same stage, only 80% are alive 4 years after diagnosis.
Overall survival of HPV-associated and HPV-non-associated oropharyngeal cancer according to TNM classification 7. ICON-S
Treatment or removal of tonsils?
Dear patients! If you have visited several specialists in this field, if a course of treatment for chronic tonsillitis has been carried out and none of the methods has brought the expected result, then only in this case should you think about removing the tonsils.
If a conservative approach gives lasting results for 4-6 months or more, then the palatine tonsils are able to fight on their own. Your task is to help the tonsils by regularly sanitizing them and stimulating their work physiotherapeutically.