Iron poisoning
· Iron Fe from lat.
Ferrum is the eighth element of the periodic table, with high chemical reactivity. · Poisoning occurs due to the ingestion of iron preparations in toxic (symptomatic) doses.
· The condition can be potentially fatal in high concentrations, especially in children.
· Early diagnosis of intoxication is essential to ensure proper treatment and prevent death.
· Poisoning is common in children under 5 years of age due to accidental overdose, usually due to irresponsible storage of medications.
· Most poisonings are unintentional and cause no acute symptoms or minimal toxicity.
· A dose of 20-60 mg/kg causes signs of moderate poisoning in an adult. Consumption of 30 mg/kg body weight is considered toxic to the body. The lethal dose is significantly higher and is more than 100 mg. In children, this threshold is several times lower.
Prevention
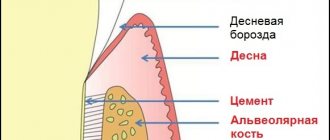
All pathologies require preventive manipulations that are aimed directly at removing plaque and strengthening the affected tooth enamel.
Preventive procedures.
- Professional teeth cleaning.
- Remineralization of enamel.
- Fluoridation of teeth.
The dentist consults with parents and the child to teach proper oral hygiene. The specialist also gives recommendations on the choice of dental care products. For general strengthening of the body and dental tissues in particular, a vitamin-mineral complex is prescribed.
Etiology and pathogenesis
· Free, unbound iron is toxic to living tissue and can locally destroy the intestinal mucosa.
· 10% of ingested iron (Fe 2+) is actively absorbed as ions in the small intestine. After absorption, iron accumulates as Fe3+ in the mucosal storage protein ferritin. From there, iron is transported to the liver, spleen and bone marrow for further storage in ferritin or for inclusion in the heme molecule.
· Iron is transported bound to the transport protein transferrin.
· When the blood's ability to bind iron is exceeded (serum iron > 90 µmol/L), free ions lead to tissue damage in most organs, including the liver and heart.
Causes: why it occurs in children
The causes of blackheads on baby teeth can vary from simple and minor to serious with serious consequences. Among the main reasons are:
- Priestley's plaque (it is not dangerous, goes away with age, and rarely transfers to permanent teeth);
- caries (first stage - yellow teeth, turning black if not treated);
- problems with intestinal microflora;
- little calcium in the body;
- a lot of iron in the body;
- heredity (if the parents had the same teeth);
- slight secretion of saliva (poorly protects tooth enamel).
With frequent colds, the development of various diseases, or taking antibiotics, bacteria begin to actively develop in the child’s mouth. If a one-year-old baby uses a rubber pacifier, then bottle caries begins to develop, which leads to the formation of black plaque on the teeth. A problem can also arise if you choose the wrong toothpaste - it must be appropriate for the child’s age.
Diagnostics
Diagnostic criteria
· History of toxic iron intake.
· Some patients develop symptoms after taking 20 mg Fe/kg body weight.
· Severe poisoning most often occurs after ingestion of > 40 mg Fe/kg body weight.
· S-Fe>90 µmol/l indicates severe poisoning, but it is also worth considering the clinic and the time elapsed after administration.
Patients with symptoms should be treated regardless of the amount consumed.
Disease history
Questions to ask the patient when taking a history:
- How many tablets were taken and for how long?
- What type of preparation?
- How long has it been since you used it?
- Has the patient also taken alcohol, drugs, or other pills?
- Does the patient have any signs of hematemesis or blood in the stool?
- Did you try to induce vomiting? How successful?
When calculating iron intake, it is necessary to take into account the iron content in the tablets (ferrous sulfate 20%, ferrofumarate 33%).
Estimating how many pills a child has taken is often wrong.
Other types of plaque depending on color
In addition to black, white or brown plaque may form on a child’s teeth. Green and orange deposits on tooth enamel are also possible. Normally, plaque appears on the teeth of all people; it usually has a light yellow tint. You need to keep this under control, brush your teeth regularly and periodically undergo ultrasonic cleaning - 1-2 times a year. If the plaque takes on any color, you should definitely see a dentist.
White plaque forms on the teeth after every meal. At night, if the oral cavity is not cleaned before bedtime, it continues to grow. Over time, it can harden and turn into tartar, which is a favorable environment for the proliferation of cariogenic microorganisms.
Brown plaque is caused by poor hygiene, overuse of coffee and tea, and smoking. Removing such pigmented plaque at home is problematic. You can use special toothpastes with abrasives, but they have contraindications. To completely get rid of brown plaque, you will have to visit the dentist's office and undergo professional teeth cleaning.
Orange or greenish deposits on the enamel indicate the growth of fungi in the oral cavity. Plaque forms not only on the teeth, but also on the inner surface of the cheeks, gums and tongue. Remove deposits in the dentist's office. Immunoenhancing therapy may also be required to eliminate the fungal infection.
Stages and characteristic symptoms
The manifestations of iron toxicity are usually described as five, often overlapping, phases:
- Gastrointestinal phase: from 30 minutes to 6 hours after oral administration. Symptoms: abdominal pain, vomiting, diarrhea, hematemesis, exhaustion, shock and metabolic acidosis. Vomiting is the most obvious indicator of severe poisoning at this stage. It occurs due to hypovolemic shock. Most patients with mild to moderate iron toxicity do not progress and symptoms resolve within 4 to 6 hours.
- Latent or relatively stable phase: 6 to 24 hours after administration. The latent phase gives the impression of improvement. It is short-lived or absent in people with severe poisoning.
- Shock and metabolic acidosis: 6 to 72 hours after ingestion. Shock, pallor, tachycardia, hypotension, coagulopathy may occur, and hepatotoxicity may further develop.
- Hepatotoxicity/liver necrosis: 12 to 96 hours after administration. Due to liver necrosis, intestinal obstruction occurs.
- Intestinal obstruction: 2-8 weeks after ingestion of Fe. Due to scarring of the gastrointestinal tract, especially at the exit from the stomach.
Clinical data
List of signs and symptoms
Stage 1 (1/2 to 1 hour after administration):
· Stomach ache.
· Vomiting and diarrhea, and bloody vomiting is not uncommon.
· Weakness, shock and metabolic acidosis may develop.
Stage 2 (6-12 hours after administration):
· Not everyone goes through this stage.
· Gastrointestinal symptoms may stop.
· This apparent recovery may provide false security.
Stage 3 (12-48 hours after administration):
· May occur early in case of serious poisoning or after the quiet phase of the 2nd course.
Metabolic acidosis and shock.
· Anemia.
· Necrosis.
· Kidney, liver and heart failure.
· Possibly fatal within 1-3 days.
Stage 4 (days to weeks after recovery):
· Obstruction of the gastrointestinal tract due to injury due to poisoning.
Additional Research
1. Determination of Fe concentration in the blood. Serum iron - useful to confirm Fe intake and to determine severity. High concentrations are not always associated with danger because they measure free circulating Fe while intracellular Fe causes systemic toxicity.
2. If serum Fe concentration is not readily available, the following may indicate serious toxicity:
Leukocytosis > 15 x 109.
· Hyperglycemia > 8.3 mmol/l.
· Diarrhea/vomiting.
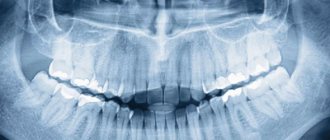
· Detection of tablet residues using abdominal x-ray.
· Serum electrolytes, blood urea and serum creatinine.
· Glucose level.
3. Coagulation parameters (INR, prothrombin), determination of leukocyte formula. Blood gases should be obtained from a patient with severe symptoms.
4. Other studies. X-ray of the abdomen. The tablets are often X-ray resistant.
Principles of therapy
The primary goal of treatment is to prevent complications. For this:
1. Aspiration and gastric emptying are performed. Vomiting is induced if <1 hour has passed since taking the tablet. This will remove iron from the digestive tract before it is absorbed. Radiologically proven Fe tablets in the stomach are indicative of lavage. Please note that the procedure is contraindicated if the patient is vomiting blood.
2. Patients who are asymptomatic when taken within 6 hours and who show no signs of clinical toxicity do not require treatment.
3. Patients with rare symptoms require only symptomatic treatment.
4. Intravenous hydration for all patients with significant symptoms. Treatment with intravenous fluid to maintain fluid balance is important because hypovolemic shock is a leading cause of premature death from toxicity.
5. Check your blood pressure and heart rate regularly, and control your breathing.
6. The antidote for poisoning is Deferoxamine. This drug increases iron excretion (Fe-binding antidote) and is indicated for severe iron poisoning.
7. If the patient is unaffected after several hours of observation and serum Fe remains low, he is discharged.
Treatment regimen
- Deferoxamine. It binds to Fe and forms a water-soluble compound, ferrioxamine, which is excreted in the urine. She turns pink.
- Deferoxamine is given intravenously in the hospital if severe gastrointestinal symptoms, shock, or coma develop.
- Continuously given equivalent to 15 mg/kg/hour. The dose may be increased to a maximum of 35 mg/kg/hour depending on severity.
Typically, treatment lasts about 24 hours. Side effects may include hypotension and acute respiratory distress syndrome.
A child has black teeth - what to do?
It is dangerous to ignore this symptom, since the pathology that caused it will develop further. In addition, plaque is a favorable environment for the active proliferation of bacteria, therefore increasing the risk of developing caries.
Diagnostics can take place in several stages. First, the dentist will examine the child's teeth for caries. If caries is excluded, examination using laser equipment and radiography are prescribed. You may need to consult with doctors of other specialties. In cases where no pathology is detected, plaque is simply removed during an ultrasound procedure.
Treatment depends on the cause of the black plaque. If a child is diagnosed with intestinal problems, he is prescribed medications that restore the balance of microflora and his diet is adjusted. If there is a lack of calcium and iron in the body, an appropriate diet is prescribed, including foods containing essential microelements. If caries develops, remineralization or filling is performed. It all depends on the stage of the carious lesion.
Progress, complications and prognosis
Gradient
The clinic is divided into four stages, which may overlap.
- Often transient symptoms such as lethargy, nausea, vomiting, diarrhea, abdominal pain. Leftover pills cause gray/black vomit and stool. Symptoms disappear after 6-8 hours. When consumed in large quantities, the local effect causes bloody diarrhea.
- Symptom of free interval pg transport and distribution of absorbed iron.
- The acute phase is observed in few patients. It manifests itself in the form of metabolic acidosis, shock, renal failure, and liver necrosis. Possible death within 1-3 days.
- Tension in the gastrointestinal tract due to damage. Complications: hypotension, shock, metabolic acidosis, liver and kidney failure, gastric fibrosis and pyloric obstruction.
Forecast
- The prognosis can be serious, but in most cases the poisoning is not life-threatening.
- Toxic doses for 2-3 years: 400 mg Fe2+.
- Lethal doses: 50 - 300 mg Fe2 + / kg.
- Patients who are alive 72 hours after administration make a full recovery.
Helpful information
Find out more about poisonings, their symptoms, treatment regimens, antidotes and consequences:
- Acetylsalicylic acid.
- Carbon monoxide: signs, symptoms, treatment.
- Benzodiazepines.
- Benzodiazepine-like hypnotics.
- Beta blockers.
- Lead, fluorine.
- Calcium antagonist.
- Cardiac glycosides.
- Ethanol.
- Ethylene glycol.
- Histamine