Problem: a woman came to the Family Dentistry for dental prosthetics. In addition to the main reason for the visit, the patient complained of pain in the lower jaw on the left, but could not indicate the exact location. Diagnostics showed that the wisdom tooth was destroyed by caries, and there was inflammation inside the tooth - pulpitis. The woman did not want to have the tooth removed.
Solution: pulpitis of the wisdom tooth (eighth tooth) was treated with a microscope, the tooth was restored with a composite.
What is special about wisdom teeth?
The maximum set of molars for an adult is 32. In this case, it is considered normal to have 28 teeth, since four teeth are the so-called eighth molars or wisdom teeth. For some, they do not erupt at all, for others, when “eights” appear, complications and pathologies arise, but in other cases, wisdom teeth occupy the correct position in the dentition and do not bother their owner. “Eights” usually appear between the ages of 17 and 27, that is, during the period when a person has already formed an attitude towards hygiene and his own dental health. Why is it important? Due to the remote position of wisdom teeth, it is quite difficult to carry out high-quality cleaning, so only very good hygiene can reduce the risk of dental damage. In reality, it is the third molars that are in the top in terms of the number of cases of caries and its common complication - pulpitis.
How to prevent the development of dental caries?
Good dental hygiene helps prevent the development of dental caries, and regular dental examinations detect caries at the very beginning and prevent complications. The distant teeth - wisdom teeth - can be difficult to access for self-cleaning. Maintaining a good level of hygiene requires professional teeth cleaning. Plaque removal using the Air Flow method cleans the most difficult to reach areas. Visiting a hygienist twice a year is a reliable prevention of caries and gum inflammation. Read more about caries prevention measures and dental hygiene here.
Pulpitis of the wisdom tooth: symptoms and treatment
Pulpitis affects the connective tissue of the tooth - the pulp. It has a crown and a root part: depending on the shape and degree of the disease, one or both parts may be affected. The symptoms of wisdom tooth pulpitis are exactly the same as in the case of other teeth.
- Painful sensations.
In acute pulpitis, the pain is acute and paroxysmal, and can be felt in the temples, ears and other parts of the jaw. The pain intensifies at night and when exposed to irritants (temperature, chemical or mechanical). With chronic pulpitis, the pain is dull and less pronounced, which makes it difficult to diagnose the disease, given the location of the wisdom tooth;
- Bleeding.
It appears only in chronic hypertrophic pulpitis, when granulation tissue grows;
- Change in tooth color.
Observed in the case of tissue necrosis with gangrenous pulpitis.
When a wisdom tooth hurts, pulpitis is just one of the options that could be the cause. To diagnose pulpitis, a visual examination, x-ray or EDI (electrodynamic diagnostics) is required. Of course, such procedures are carried out only by professionals, so if you suspect pulpitis, you should immediately make an appointment with a doctor. Most patients who face a similar problem have two questions: is wisdom tooth pulpitis treated and is it worth treating wisdom tooth pulpitis. The answer to the first question is yes, but to answer the second, you need to consider each clinical case separately.
In order to answer this question, let’s figure out what kind of wisdom teeth they are.
It is not without reason that wisdom teeth received such an interesting name; many beliefs and legends are associated with them. The ancients believed that a person develops these teeth (17 - 25 years old) only when his soul has strengthened, become mature, and life wisdom has appeared. The eruption of all 4 teeth indicated the protection of the clan, so they were practically not removed - because then the person was deprived of protection.
These teeth are also called “eights”, as they are the eighth in the dentition. Wisdom teeth are unique because they are the only group of teeth that do not have a clear anatomy, and for the most part they are all different. It is impossible to be unambiguously sure of the number of root canals and their patency.
Nature has endowed humans with “figure eights” so that the teeth are located closer to each other and to make chewing hard food easier. Now this problem has lost its relevance. In the modern world, we eat softer food, so wisdom teeth began to grow much later than others and not in all people, so “eights” are considered to be rudiments. According to data, 15 - 20% of the population have no wisdom teeth at all, not even the rudiments. The rest have rudiments, but often they prefer to remain in the thickness of the jaw and not rise to the surface. And only some “lucky” ones can experience the beauty of teething already in adulthood.
The unpleasant sensations that wisdom teeth sometimes cause can be safely blamed on the process of evolution. Over the millennia, the human body has transformed, and the jaw is no exception. Gradually it decreased, but the size of the teeth did not change. Because of this, wisdom teeth, which are the last to grow, do not have enough space in the mouth.
Wisdom teeth, indeed, are almost not involved in the chewing process. But you shouldn’t neglect them either, since a fully erupted wisdom tooth in the event of loss of other teeth can “save” a person from removable dentures.
In what cases is it worth fighting to preserve a wisdom tooth?
Arguments for"
A wisdom tooth that has completely erupted and is affected by caries can and should be treated. If the canals are well passable, not curved and can be filled with high quality, even complications of caries (pulpitis, periodontitis) are not a “sentence” for these teeth.
There is one advantage in the “eights”, because of which some patients try to save them. Erupting later than others, wisdom teeth can become a support for a bridge prosthesis - instead of damaged teeth. Without the figure eight, such permanent prosthetics will only be possible with the help of implants.
A wisdom tooth may definitely be required for prosthetics if: the seventh tooth in front is missing, both the sixth and seventh teeth are missing, or the sixth and seventh teeth have not yet been removed, but will soon be removed.
Definitely delete!
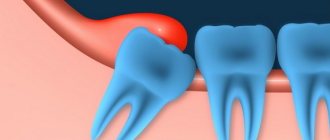
Delayed eruption (retention), incorrect position (dystopia) of the wisdom tooth
As a rule, this is a partially erupted wisdom tooth, lying horizontally or with its crown tilted towards the lingual, buccal, medial (inclined towards the “seventh” tooth), distal (towards the angle of the jaw) sides. The value of such a tooth for prosthetics and chewing food is zero. It happens that the crown of a wisdom tooth has a pronounced slope towards the cheek area. This leads to the person biting his cheek all the time. Chronic injury to the buccal mucosa can even lead to the development of an oncological process in this area. There is no point in preserving such teeth.
2) Destruction of the front (“seventh”) tooth
As mentioned above, wisdom teeth often erupt at an angle. The front cusps of the crown sometimes rest against the seventh tooth in front. Lack of adequate hygiene and constant pressure from the wisdom tooth on the enamel of the nearby tooth can cause its destruction and the occurrence of caries. Preserving the seventh tooth and its full treatment is sometimes not possible without removing the wisdom tooth.
3) Orthodontic indications (bite anomalies).
Previously, to correct the bite, “fourth” teeth (less often “fifth” teeth) were often removed for subsequent orthodontic treatment. These teeth are located in the smile line and from an aesthetic point of view, it is currently more advisable to preserve them. Therefore, removal of wisdom teeth is the right decision, since they can provoke relapse after early orthodontic treatment, due to later eruption. In addition to removing impacted wisdom teeth, orthodontists recommend removing even the rudiments of these teeth.
4) Pericoronitis (inflammation of the mucous hood).
A fully or partially erupted wisdom tooth occupies such a position that part of its crown is covered with an overhanging hood of mucous membrane. In this case, a space is formed between the hood and the tooth in which microbes multiply, which leads to inflammation. In such cases, patients, as a rule, note aching pain in the jaw, discomfort when opening the mouth (sometimes limited mouth opening caused by inflammatory muscle contracture), pain when swallowing, enlarged lymph nodes, and sometimes swelling of the cheek appears. In this case, to stop the inflammatory process, the mucous hood is excised, followed by anti-inflammatory therapy. Such inflammations can happen more than once, so the only correct solution is to remove the wisdom tooth.
There are situations when it is impossible to maintain the “eight”, and inaction is dangerous!
These are inflammatory processes caused by wisdom teeth. Periostitis (inflammation of the periosteum of the jaw). Initially, complaints appear of aching pain in the tooth, which intensifies when biting (a symptom of an “overgrown” tooth). If the patient ignores these pains, the inflammatory process spreads to the periosteum. In such cases, swelling appears and general health worsens. At the same time, pain in the tooth decreases. In case of extensive destructive process on the roots, the tooth is removed with dissection of the periosteum (periostotomy) and subsequent drainage of the lesion.
More serious complications are osteomyelitis (inflammation of the jaw), abscesses and phlegmons (limited and widespread purulent processes of soft tissues), abscessing lymphadenitis (purulent melting of the lymph nodes) and others. These diseases are an indication for the removal of wisdom teeth, followed by serious treatment in a hospital.
Summarizing all of the above, I would like to focus on the fact that everything is very individual, and only after carefully weighing all the pros and cons, having received a comprehensive consultation with a doctor, should you make a decision regarding treatment or removal of a wisdom tooth.
Pulpitis of the wisdom tooth: treat or remove?
In most cases, a wisdom tooth with pulpitis is removed. The main indications for removing a diseased “eight” are developmental pathologies, as well as being outside the bite (in this case, the tooth has no function). We are talking, first of all, about retention and dystopia. An impacted wisdom tooth is completely or partially hidden in the jaw, and a dystopic wisdom tooth has an incorrect position relative to the rest of the dentition. These pathologies in themselves are a good reason for removing the “eight”, however, if pulpitis occurs due to the impossibility of full treatment, such teeth are definitely removed.
Causes
The reasons for the development of pathology may be the following:
- Tooth injury, mechanical or chemical. Violation of the integrity of enamel and dentin makes the pulp extremely vulnerable to the effects of the external environment and pathogenic bacteria.
- Gum diseases. In this case, there is a high risk of infection entering through open periodontal pockets.
- Complications of caries. Uncured caries or its advanced form contribute to the entry of pathogenic microorganisms - streptococci - into the pulp through the dentin tubules.
- Incorrectly performed dental treatment - damage to dental tissue, opening of a tooth performed in violation of technique, burn of dental tissue by arsenic, etc.
- Incomplete removal of carious tissue during treatment. The infection persists in the dental cavity and continues to develop.
- Poor quality filling installation. It is dangerous because there is a gap between the tooth wall and the filling material. Through it, pathogenic microorganisms penetrate into the pulp.
Treatment of wisdom tooth pulpitis
Treatment of wisdom tooth pulpitis is carried out in the same way as on other teeth. In 90% of cases, the doctor performs complete removal of the pulp: only in the initial stages of chronic fibrous pulpitis is it possible to save part of the pulp. However, even if the wisdom tooth is positioned correctly and has completely erupted, very often the doctor suggests extraction rather than treatment. This is due to some features of wisdom teeth that reduce the likelihood of a successful treatment outcome.
- Location of position. Wisdom teeth are difficult to reach, and treatment of pulpitis requires almost pinpoint precision.
- Wisdom teeth have curved roots, which sometimes makes the depulpation procedure extremely difficult.
Despite the difficulty of treatment, sometimes preserving wisdom teeth is advisable. First of all, this applies to situations where, of all the molars, only “eights” remain (in the future, a prosthesis can be attached to them), as well as in the initial stages of the disease, when the chances of a successful and predictable result are higher.
Symptoms
- pain syndrome
. A typical sign of acute inflammation is spontaneous pain, intensifying at night, which spreads to the temporal/occipital area, cheekbones, and ear. It occurs unexpectedly and does not depend on the influence of external stimuli. The attack can be long with short intervals, short with long intermissions. As the infection spreads, unpleasant sensations appear during palpation and percussion of the tooth. The chronic disease is characterized by an asymptomatic course, in 10-15% of cases there is a weak reaction to solid/hot foods; - bad breath
; - the presence of tooth deformations
- enamel cracks, caries; - Body temperature
and enlarged regional lymph nodes are rarely recorded.
Acute inflammation is accompanied by hyperemia and swelling of the connective tissue, which occurs against the background of deep caries. The development of hyperemia is manifested by moderate paroxysmal pain that passes after 1-2 minutes. During diagnosis, a depression filled with softened dentin is revealed; the patient experiences unpleasant sensations when probing its bottom.
Modern techniques
- Gutta-percha lateral condensation method.
In clinics in the West, this option is used to treat roots for acute and chronic pulpitis in approximately 80% of cases. The bottom line is that the canal, after removing the tissue and mechanical processing with special instruments, is filled with thin flexible gutta-percha pins in combination with a special hardening paste. Gutta-percha is the dried sap of the gutta-percha tree, growing in Brazil and Malaysia. It has an antiseptic effect, working in the canal similar to a sealant. All drugs used are non-toxic and non-irritating. A positive result is possible only with strict adherence to technology. It is important that the filling paste does not extend beyond the root tip. If the doctor says that nothing bad happened and it will resolve over time, this is not true. Some substances irritate the periodontium, which can lead to complications in the jaw; - Thermafil system.
The roots are processed with a special apex locator device, which controls the approach to the apex and prevents damage. Flexible nickel-titanium instruments allow you to restore even curved canals, giving them the correct conical configuration. Then one gutta-percha pin of the required thickness, heated in a special oven, is placed into the canals. Pros: accuracy, reliability, low time consumption. With the help of equipment, treatment of pulpitis of a three-canal tooth (premolar) takes only 30 minutes, while manual treatment can take more than one hour, which is difficult for the patient. The only negative is the high cost; - Resorcinol-formalin.
This conservative technique in dentistry was invented almost 100 years ago and is considered obsolete. Is it possible to help patients who have already been treated with the resorcinol-formalin method? It is much more difficult to cure a resorcinol-formalin tooth. The complexity arises, since in 70% of cases there are complications in the form of chronic periodontitis, cysts, granulomas. The question of the possibility of re-treatment of the affected canals and elimination of dangerous complications is decided individually, after a thorough diagnosis.
Diagnosis of pulpitis
The disease is diagnosed after consultation, analysis of the patient’s complaints and a dental examination and x-ray examination of the problem tooth. During an instrumental examination, carious lesions, a painful reaction to thermal stimuli, and softened dentin are detected. Percussion is painless. To clarify the diagnosis, the doctor prescribes additional medical tests. Using a special apparatus, the electrical excitability of the pulp and the degree of its damage are determined. An X-ray is required to identify a diseased tooth and determine the depth of periodontal damage.
Classification
- Acute (focal, diffuse).
Characterized by changes in the horn area, outside the coronal part. Discomfort occurs under the influence of external irritants. Timely initiation of therapy guarantees a 100% positive result. This phase lasts about 2 days, progressing to the diffuse stage - the roots and coronal segment are affected. Characterized by paroxysmal pain that occurs without the influence of internal/external factors; - Chronic (hypertrophic, purulent, gangrenous, fibrous).
The disease becomes permanent, the intensity of the pain syndrome decreases. The fibrous appearance does not produce pronounced symptoms; a diagnostic examination by a dentist reveals a depression extending to the chamber. Against the background of constant hypertrophic inflammation, it connects with the chamber, a process appears - a polyp, occupying all the free space. The patient experiences pain while eating, and blood may ooze from the organ. Serious consequences in the form of gangrenous pulpitis of permanent units develop due to putrefactive decay. At this stage, putrid breath appears, prolonged aching pain from irritants, which intensifies after eating hot food. In the retrograde form, periodontal pockets are diagnosed, which occupy a large part of the root. The source of infection is located in this place. Inflammatory processes begin to cover the root segment, gradually moving to the coronal segment.