Any punctured, chopped, torn or cut wound can be complicated by the process of suppuration. Even if you cut your finger with a knife in the kitchen, you should not think that this is a trifle, because an insufficiently treated wound can fester. Everyone should know the first symptoms of wound suppuration for the reason that in most cases this problem has to be solved exclusively by surgery.
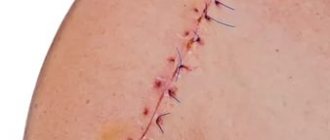
This problem is especially relevant for those who have undergone any surgery and were discharged home after rehabilitation. If postoperative sutures are not cared for at home as prescribed by the doctor, then if an infection occurs, suppuration may begin. Contrary to the generally accepted opinion of patients, suppuration after operations begins not because of the conditions during the operation, but precisely due to the fault of patients who irresponsibly approach the doctor’s prescriptions when they find themselves at home.
During surgery, it is essential to maintain absolute sterility, and this principle is never violated. Medical doctors recommend that you always fully follow the prescriptions they make to avoid such serious complications.
How does the process of wound suppuration develop?
Typically, suppuration begins when a clean wound becomes infected, swelling around the wound develops, tissue necrosis and purulent discharge appear. If redness begins around the wound, which is accompanied by a tugging pain that gets worse at night, then this means that you are dealing with the first symptom of wound suppuration, and urgent measures need to be taken.
When examining the wound, dead tissue and pus are visible. The situation is dangerous because the decay products are absorbed by the body, and this leads to increasing intoxication of the body. As a result, the following symptoms appear:
- significant increase in temperature;
- chills;
- headache;
- weakness;
- nausea.
Why you don't need to remove white plaque
Careless performance of oral hygiene procedures can cause damage or removal of the protective film. A number of negative processes result from the destruction of the barrier:
- Opening a wound for access of pathogenic microorganisms that provoke inflammation and infect the body’s circulatory system;
- Increased pain caused by the sensitivity of unprotected tissues to any form of external influence;
- Reopening of bleeding and increasing the duration of healing of the alveolar socket.
Accidental damage can be avoided by following medical recommendations.
How to maintain the integrity of white plaque after tooth extraction?
Reducing the risk of developing complications that occur against the background of exposure of the tooth extraction site involves following the following instructions:
- Abstain from drinking and eating for three hours from the end of the operation;
- Avoiding increased temperature in the affected gum area, including overheating as a result of taking a bath or visiting a sauna;
- Temporary cessation of bad habits, including smoking and drinking alcohol;
- Observe a daily break in relation to the procedure of rinsing the mouth and brushing the teeth;
- Reduce physical activity for the entire recovery period.
In situations where the pain after removal of the unit remains noticeable and causes severe discomfort, it is permissible to take painkillers prescribed by the attending physician. If you detect uncharacteristic discharge, which is a liquid mass, the spread of swelling to the gum tissue, as well as an increase in temperature to 38 degrees, you should immediately seek help, since these symptoms may indirectly indicate the development of infection or complications.
Causes of wound suppuration
Any wound, small or large, is considered infected because bacteria will get into it anyway. However, this does not always lead to suppuration. In order for this destructive tissue process to develop, additional conditions are required:
- sufficient tissue damage;
- the presence of non-viable tissue in the wound cavity;
- the presence of foreign bodies in the wound cavity;
- the presence of bleeding blood in the wound cavity;
- high concentration of pathogenic microorganisms.
Therefore, the first symptoms of wound suppuration can appear even after an ordinary splinter, provided that a piece of it remains in the body tissue, and at the same time there are pathogenic microorganisms on the foreign body itself. The latter include those that are responsible for the development of the purulent process: staphylococci, streptococci, E. coli and similar microorganisms.
In addition, there is a high risk of suppuration when the patient has a history of diabetes mellitus, vascular and somatic diseases, excess weight and old age.
The nature of the wound also matters for the development of this process. Thus, a puncture wound can fester due to the wound channel being too narrow and due to which there is no normal outflow. In the case where the wound is accompanied by crushing of surrounding tissues, suppuration occurs due to too much dead tissue in the wound and excessive contamination. At the same time, wounds on the head and neck heal faster and better, and worst of all – on the feet.
Purulent wound - symptoms and treatment
An infected wound should be treated immediately. It requires an integrated approach, i.e. it must affect both the wound and the body as a whole.
To combat the causative agent of wound infection, use:
- antibacterial drugs;
- antiseptics (miramistin, chlorhexidine, prontosan, betadine);
- immunological preparations (pentaglobin, gabryoglobin, imbioglobulin).
On the first day, empirical antibacterial therapy (amoxicillin/clavulanic acid, ciprofloxacin) is most often prescribed. Therapy is then adjusted depending on the results of bacterial cultures, taking into account the sensitivity of the identified infection to antibiotics. In addition to antibacterial drugs, patients are prescribed bacteriophages (viruses that selectively kill bacterial cells).
Also, in the case of a purulent wound, a comprehensive detoxification of the body :
- hemodilution - dosed dilution of blood with plasma-substituting fluids;
- accelerated neutralization, destruction and elimination of toxins, metabolites and biologically active substances using forced diuresis (increased urine volume), intravenous administration of solutions and blood purification methods - plasmapheresis, hemofiltration and hemodialysis.
Symptomatic therapy includes pain relief and correction of damaged organs and systems.
In addition to surgical treatment, wound drainage . It allows you to improve the outflow of pus. To do this, various tubes, half-tubes and glove drains are installed in the damaged area.
Hypertonic solutions, hydrogels, proteolytic enzymes in the form of powders or solutions, UHF therapy, various methods of cavitation (ultrasonic exposure), plasma and laser treatment of the wound can be used locally to cleanse the wound. In particular, proteolytic enzymes, acting as a “biological scalpel,” help remove dead tissue from the wound [14].
Treatment of a purulent wound should only be carried out under the supervision of a physician, since the drugs used can cause an allergic reaction [6].
To stimulate regeneration, zinc-containing ointments, vitamins, ultraviolet irradiation, sea buckthorn and rose hip oil are used. The method of applying secondary sutures is also widely used . They are applied only after the wound has been cleansed of pus. To speed up healing and prevent the formation of a hypertrophic scar, it is possible to use a laser, a pulsating magnetic field and electrophoresis with lidase (a special enzyme).
Modern treatment methods include systemic ozone therapy . It improves the utilization of oxygen in the body, has a detoxifying and immunostimulating effect [16].
There are several methods of ozone therapy. The most commonly used in the treatment of purulent wounds include:
- external use of a gaseous ozone-oxygen mixture (direct exposure to a device that supplies ozone to the wound);
- the use of special caps with normal or reduced gas pressure (for example, “ozone boots” - the limbs are placed in a hermetically sealed plastic bag, into which an ozone-oxygen mixture is then supplied at a certain pressure for 15-30 minutes).
Hyperbaric oxygenation (HBO) has also shown good results in the treatment of purulent wounds . It is carried out in special medical pressure chambers: the patient is placed for a certain period of time in a pressure chamber containing oxygen under high pressure. In addition to eliminating tissue hypoxia (lack of oxygen), HBOT suppresses the proliferation of anaerobic bacteria and destroys aerobic bacteria. This method also reduces the formation of toxins and increases the body's immunity.
Dermoplastic surgeries are used:
- with extensive defects against the background of a satisfactory general condition of the patient;
- after cleansing the wound;
- in the absence of inflammation and circulatory disorders in the tissues surrounding the wound;
- when bright granulations appear (young connective tissue with an abundance of blood vessels);
- in the presence of a small amount of serous discharge from the wound;
- when self-healing is impossible.
There is full-thickness skin grafting, which allows you to completely restore the skin, providing good cosmetic and functional results. It is divided into plasty using local tissues and a displaced skin flap (Indian plasty, Italian plasty on a feeding pedicle, as well as microvascular plasty techniques). These methods of surgical wound closure are not always feasible (for example, with extensive soft tissue defects, localization of wounds in sedentary areas of the skin). Therefore, in some cases, plastic surgery with a free split skin flap is used [12]. After this operation, the wound heals through a scar - the skin is not completely restored.
The choice of skin grafting method is carried out taking into account the type and location of the wound, the individual characteristics of the patient, the condition of the surrounding skin and the nature of the tissue.
The modern and most effective method of treating purulent wounds is the VAC (vacuum therapy) method [18]. Due to the effect of negative pressure on the bottom and edges of the wound, it accelerates the formation of granulation tissue, improves local blood supply and reduces swelling. All this promotes rapid wound healing and enhances the effect of drug treatment [20].
Vacuum therapy is carried out as follows:
- to begin with, dead and damaged tissue is completely removed from the wound;
- the cleaned wound cavity is filled with special foam (polyurethane sponge);
- a drainage tube is attached to the surface of the sponge to remove air and exudate;
- to fix the bandage and maintain the vacuum, the resulting structure, together with the edges of healthy skin, is covered with an adhesive transparent film;
- the drainage tube is connected to an aspirator (VAC device), which creates the required level of pressure and draws fluid from the wound [19].
Unlike aseptic gauze dressings, which need to be changed every day, vacuum dressings can be left in the wound for 3-7 days. Due to their tightness, they reduce the risk of new infection [17]. In this case, the destruction and removal of pathogenic microorganisms occurs two times faster than with other methods of treating a purulent wound [20].
Contraindications to vacuum therapy:
- incomplete cleansing of the wound;
- osteomyelitis (inflammation of bone tissue);
- blood clotting disorder;
- malignant tumor in the wound;
- skin fistulas;
- allergic reaction to the components used [20].
Operations
If there is phlegmon or an abscess, namely acute suppuration, surgical intervention cannot be avoided. The area is opened and non-viable yellow tissue is excised. This color indicates their death. Then they are sent for examination. Surgeons dry and wash the problem area several times.
Then special tampons are used. They are soaked in saline solution. In case of severe pain against the background of fibrinous plaque, you cannot do without formulations with novocaine. After the operation, stitches are placed. They can be removed after nine days, but only if healing is good and fast.
What is a surgical site infection?
An SSI is an acute or chronic inflammation that develops at the site of an incision or in an area that has been iatrogenic during surgery. In 67% of cases, the infection affects only the surgical incision area, and in 33% it spreads to the implanted joint.
Factors for the development of SSI:
- the duration of the operation is more than 3 hours;
- technical difficulties during surgery;
- intraoperative blood loss more than 1 liter;
- instability of the installed endoprosthesis;
- the use of additional synthetic and biological materials during the operation;
- the presence of severe chronic diseases.
Inflammatory processes that do not spread to the operated joint can be overcome without revision arthroplasty. If the infection affects bone tissue, components of the endoprosthesis, remnants of the joint capsule or other parts of the knee or hip joint, it will be extremely difficult to treat. In this case, the patient will most likely require repeat arthroplasty.
There are a number of factors that aggravate the patient’s condition, slow down recovery and worsen the prognosis: decreased immunity, previous surgeries, frequent treatment with antibiotics. The resistance of the detected microflora to antibacterial agents, poor blood circulation in the joint area, and massive purulent lesions also complicate therapy.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Minimally invasive endoprosthetics in the Czech Republic: doctors, rehabilitation, terms and prices.
Find out more
Wound care at home
- Do not remove the wound dressing for __________ hour(s) after the procedure. Keep it clean and dry.
- If your doctor or nurse tells you to ice the wound, you can apply an ice pack every hour while you're awake for _____minutes, or as directed by your healthcare provider. You can do this for the first 24 to 48 hours after the procedure. This will help reduce bleeding, pain and swelling.
- You may shower __________ hours after the procedure. Let a weak stream of soul flow over the wound.
- Pat the wound dry with a clean gauze pad or a clean, dry terry cloth.
- Do not bathe, swim, or use a hot tub until the wound has healed.
Cleaning the wound
Clean the wound every day. Do this for _____ days/weeks after the procedure or until your next doctor's appointment. Follow the instructions below when cleaning the wound.
Prepare everything you need
To clean the wound you will need the following:
- one package of cotton swabs (Q-tips®);
- one package of non-stick gauze pads;
- solution ______________________________;
- ointment ______________________________;
- adhesive tape (Band-aid®), cut to fit the wound;
- paper patch.
- a clean gauze pad or a clean, dry terry cloth.
Instructions for cleaning a wound
- Prepare everything you need.
- Wash your hands with warm water and soap for at least 20 seconds or use an alcohol-based hand rub.
- Clean the wound with ______________________________ solution.
- Gently pat the wound dry with a clean gauze pad or a clean, dry terry cloth. Do not rub this area.
- Using cotton swabs, apply ointment ______________________________ to the wound.
- Cover the wound with non-stick gauze cut to fit the wound or Band-aid. If you are using non-stick gauze, secure it with paper tape.
- When finished, wash your hands with warm water and soap or use an alcohol-based hand sanitizer.
Follow these instructions for __________ days/weeks, or until the wound has healed.
Additional instructions:
to come back to the beginning
Lab tests
Taking tests helps identify acute and chronic inflammatory processes in the body. An increase in indicators is not a reliable sign of SSI. To make a diagnosis, it is necessary to take into account the presence of certain clinical symptoms, radiographic data and other research methods.
Clinically significant laboratory parameters:
- Leukocyte count. It is important in the diagnosis of acute paraprosthetic infection. A clear sign of inflammation is an increase in the total number of leukocytes and neutrophils, a shift in the leukocyte formula to the left.
- ESR. It is a non-specific indicator. A normal erythrocyte sedimentation rate indicates the absence of inflammatory processes, an increased rate indicates their presence.
- C-reactive protein. CRP is an acute phase protein and a highly sensitive marker of SSI in people who have undergone arthroplasty. When diagnosing paraprosthetic infections, you need to pay attention to this indicator.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Minimally invasive endoprosthetics in the Czech Republic: doctors, rehabilitation, terms and prices.
Find out more
Pain relief after the procedure
- You may experience pain or discomfort after the procedure. To relieve these symptoms, take acetaminophen (Tylenol®) or strong acetaminophen (Extra Strength Tylenol®).
- Do not take aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil®) or naproxen (Aleve®). These medications make it harder for your blood to clot and may increase bleeding.
- Follow dosage directions on the package. If the recommended dosage does not relieve pain, call your doctor.
- If you are allergic to acetaminophen or have a medical condition that prevents you from taking it, ask your healthcare professional what medicine you can take instead.
- If you are participating in a clinical trial for cancer treatment, ask your oncologist (cancer treatment doctor) what pain medications you may take.
- You can also apply an ice pack to the wound to reduce pain, swelling, and bruising. Apply an ice pack to the wound for 15 to 20 minutes every hour or as directed by your healthcare professional.
to come back to the beginning
Prosthetic joint infections
In pathology, inflammation spreads to the cavities and membranes of the operated joint, remnants of the synovial membrane, bones at the site of fixation of the endoprosthesis and adjacent soft tissues. The cause of the complication is the colonization of joint surfaces by pathogenic microflora. Bacteria can come from the external environment or be introduced hematogenously.
This is what an infection looks like on an x-ray.
Prosthetic joint infections are the most serious complication among all SSIs. They do not respond to conservative therapy, so they have to be treated surgically. Doctors replace the endoprosthesis, but sometimes they still manage to save it.
There are three methods for treating infections of a prosthetic joint: wound revision without removing the implant, one-stage revision and two-stage endoprosthetics. The choice of technique depends on the patient’s condition, the time of manifestation of the infection, the stability of the prosthetic components and the nature of the pathogenic microflora.
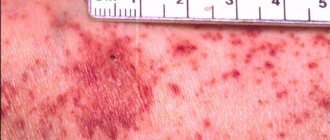
Diagnosis of trophic ulcers and pathologies that became the root cause of its development
- The following features indicate that the patient’s leg is not just an infected wound, but a trophic ulcer:
- The typical localization of a trophic ulcer is the lower third of the leg
- The skin around the wound surface is usually thickened
- The skin in the immediate vicinity of the wound has pronounced pigmentation
- With intense palpation, characteristic “pits” form in the soft tissues
- The wound surface itself and nearby tissues show signs of inflammation (redness, swelling)
- The wound oozes, the ejected contents have an admixture of pus and a specific smell of rotting
If a person has pronounced manifestations of vascular pathologies (for example, dilated tortuous veins resembling bunches of grapes), then it makes sense to talk not just about the vascular cause of trophic development, but about an advanced stage of varicose veins.
Often patients with trophic ulcers are admitted to the hospital after suffering thrombophlebitis.
By the way, sometimes a person does not even realize that he has suffered thrombosis - because the pathology proceeded without pronounced signs. However, with increased blood clotting, episodes of surgical interventions, or prolonged immobility of the patient, it makes sense to talk about a high probability of thrombosis.
To assess the condition of the venous system of the lower extremities, doctors at the ANTIREFLUX Center use high-precision innovative technologies: the “gold standard” for diagnosing venous diseases - ultrasound angioscanning, as well as spiral computed tomography, which provides images in three-dimensional implementation. This research method allows us to identify even hidden vascular pathologies.
Treatment
In order for the wound to heal as quickly as possible, it is necessary to suppress the infection. At the initial stage it is important:
- Ensure drainage of pus. If it is present under a crust formed on the wound, it must be soaked in hydrogen peroxide. Then the upper fibrinous layer is removed with a bandage, which is applied for 30 minutes. It is also soaked in peroxide or other antiseptics.
- Get rid of pus accumulated under the skin and fibrin plaque. To do this, it is squeezed out of the hole, which is made along the edges where areas of the skin have dried.
- Be sure to treat the problem area with hydrogen peroxide every day. The pus is disposed of as it accumulates, so that the wound does not become covered with fibrin again.
IMPORTANT! It is recommended to use Levomekol. This is an effective remedy that promotes healing of fibrinous plaque. It will be useful to use a bandage with it every day.
X-ray studies
X-ray fistulography plays an important role in the differential diagnosis of fistulous forms of infection. With its help, you can determine the size, shape and location of fistulas, identify purulent leaks and their connection with foci of bone destruction. This makes it possible to distinguish superficial from deep SSIs.
Photo: X-ray fistulography, fistula in the lower third of the thigh.
X-rays are most often used to diagnose prosthetic joint infection. The method does not give 100% correct results, but it allows one to suspect pathology. The presence of a paraprosthetic infection is indicated by the sudden appearance of a periosteal reaction and osteolysis. If these signs appear suddenly, soon after a successful operation, there is reason to suspect something is wrong.
Curious! MRI, ultrasound and radioisotope scanning are rarely used for diagnostic purposes due to their low information content. For example, an installed endoprosthesis interferes with magnetic resonance imaging, which makes the image blurry and unclear.
Healing process
- After some time, a crust may form on the wound. If a crust forms, do not remove it. She'll get off on her own. Continue applying Aquaphor® or Vaseline® until the wound is completely healed.
- You may notice a thin, pale yellow film on the wound. It may also have a thin pink rim (less than ¼ inch (6 mm)) around it. This is fine.
- The skin color in the wound area may change (pink or red) for up to 1 year after the procedure. For some people it may last even longer.
- After the wound has healed, apply a broad-spectrum sunscreen with an SPF of at least 30. This will help protect your skin from sun exposure.
to come back to the beginning
Why do complications occur after tooth extraction?
The most common reason for the development of complications is the patient’s failure to comply with medical prescriptions. Normally, the hole should heal within a few days. She shouldn't be sick for a long time. As a result of the fact that the blood clot closes it, it is reliably protected from viruses and food debris.
It happens that a person actively rinses the wound or constantly touches it with his tongue, fingers, and tries to remove the light coating. Then the clot displaces or does not form completely, the tissue becomes infected and alveolitis develops.
Untreated neighboring teeth can also lead to disease (which is why all carious “cavities” need to be treated before removal), and failure to comply with the rules of oral hygiene. If you properly prepare for extraction and follow all the doctor’s instructions, the risk of developing alveolitis after removal will be minimal.