Enlarged lymph nodes in the neck indicate their inflammation - lymphadenitis. It can occur for various reasons, but often develops against the background of dental diseases and their complications. The list of these pathologies also includes caries. In the article we will tell you what lymphadenitis is and what role the carious process plays in its development.
In this article
- What is caries and why does it occur?
- Stages of caries
- Caries and other diseases
- Caries and submandibular lymph nodes - what is the connection?
- Inflammation of the submandibular lymph nodes and diseases of the oral cavity
- Gingivitis and lymph nodes
- Periodontitis and lymph nodes
- Pulpitis and inflammation of the lymph nodes
- Stomatitis and inflammation of the lymph nodes
- Purulent tooth abscess and lymph nodes
- Other causes of inflammation of the submandibular lymph nodes
- What are the symptoms of inflammation of the lymph nodes?
- Types and forms of submandibular lymphadenitis
- Diagnosis of submandibular lymphadenitis
- The main directions of treatment of submandibular lymphadenitis
- Treatment of submandibular lymphadenitis with caries
- What not to do if you have swollen lymph nodes
Lymph nodes serve as a filter in the body. They accumulate harmful substances and neutralize them, preventing them from passing into other parts of the body. Lymph nodes are located in various parts of the human body: on the arms, legs, neck, behind the ears, etc. An increase in the size of the lymph node indicates the presence of some kind of disease or pathological process. In the presence of inflammation, pain occurs, skin redness, swelling and other symptoms are observed. With their help, this small peripheral organ of the lymphatic system signals the need to check your health.
Often the inflammatory process that originates in the lymph nodes is a consequence of infectious diseases. It can also be provoked by other reasons, for example, caries and other dental ailments: periodontitis, periodontal disease, gingivitis, etc. To understand how this happens and why a carious lesion should not be left untreated, we will talk about its main features.
What is caries and why does it occur?
Caries is a slowly progressive disease in which tooth enamel and dentin are destroyed. It occurs due to the impact of cariogenic microbes and their metabolic products on the teeth. Bacteria feed on carbohydrates and secrete harmful acids that upset the balance of minerals in the oral fluid and enamel, gradually corroding it and leaching calcium, fluorine and other trace elements from it.
It becomes soft, loose and porous, as a result of which it cannot fully resist microorganisms.
- Cariogenic microbes live in the oral cavity of almost every person. But caries occurs only under certain conditions. These include:
- Poor hygiene. Food debris, plaque and tartar stuck between teeth are favorable factors for the spread of bacteria.
- Anatomical features of the teeth and jaw: malocclusion, deep and narrow fissures, crowded teeth, etc. Because of this, it is more difficult to carry out hygiene procedures.
- Presence of braces or other orthodontic structures. They also complicate hygiene: food debris gets stuck between the teeth and braces, which feeds bacteria.
- Disorders of saliva production. It neutralizes acids secreted by cariogenic microbes and maintains the pH of the oral fluid. If saliva is not produced in sufficient quantities, the balance of minerals is disrupted, which makes the enamel vulnerable to external factors.
- Abuse of sweets. The bacteria that cause caries live off carbohydrates, more precisely, sucrose. It is found in large quantities in confectionery products. People who eat a lot of sweet foods are more likely to suffer from tooth decay.
These are the main factors that increase the risk of caries. However, this list cannot be called exhaustive; it can also include poor ecology, genetic predisposition to dental diseases, abrasion of enamel, drinking water with a low mineral content, etc. When diagnosing caries, it is much more important to determine its stage, on which the treatment method depends.
Inflammation of the lymph nodes with carious lesions is not always observed. They often become inflamed due to advanced caries. We will tell you how this pathology occurs and why it causes other diseases that are not directly related to teeth, including lymphadenitis.
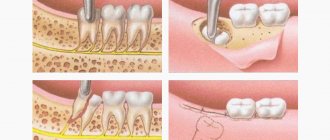
Why can a lymph node become inflamed after tooth extraction and what to do about it?
An enlarged lymph node signals the occurrence of an inflammatory process in the body. Typically, during inflammation, the lymph nodes increase in size and some pain appears. Swelling of the lymph nodes of the neck, head and lower jaw is associated with the development of inflammation in the area of the extracted tooth. In this article you will learn how to avoid complications and how to help the body cope with infections faster.
Lymph nodes and where they are located
Let's start with the lymphatic system. It is represented by a collection of vessels of various diameters that permeate our body. The lymphatic system is closely related to the circulatory system (this plays an important role in the development of complications). Lymph, the fluid that flows through the lymphatic vessels, transports tissue fluid and protein molecules. There are large numbers of lymphocytes and granulocytes - cells that are the first to fight pathogens. They are produced in the lymph nodes; when an inflammatory process occurs in the body, the lymph nodes work more intensely, increasing in size.
Photo 1 shows inflammation of the lymph node
But how does this relate to tooth extraction?
Most of the lymph nodes are concentrated in the head and neck area. Surprisingly, it is true: inflammation in the lymphatic system in 60% of cases occurs due to dental pathologies. The process of tooth extraction is a very traumatic event. In addition, a large number of opportunistic microorganisms live in the oral cavity.
Attention: Opportunistic pathogens are those that are normally present on the surface and inside the human body, but do not cause harm to it. However, when conditions change, they can become pathogenic and lead to the development of diseases.
So, bacteria entering the wound formed after tooth extraction can cause an infectious process. The nearby lymph nodes of the jaw, neck and head will react most quickly to it, actively producing cells of the immune system. Therefore, the patient can feel enlarged lymph nodes, which in some cases can be painful.
Why does the problem occur after tooth extraction?
After tooth extraction, in 99% of cases the lymph node swells. Dentists identify two main reasons:
1. This is a defensive reaction to interference, and it is the norm. As a rule, after tooth extraction, the lymph nodes in the neck or under the jaw become enlarged.
Attention: When wisdom teeth, or numbers of eights, are removed, the lymph nodes in the neck become enlarged. The procedure is quite traumatic and affects a large number of tissues, so in 90% of cases the lymph node becomes enlarged. It may also be accompanied by fever, soreness, inability to open the mouth wide, and general malaise.
- Tooth extraction was carried out against the background of an existing purulent-inflammatory process. In some cases, tooth extraction is a necessary step in solving advanced dental inflammatory diseases of the oral cavity, which include:
- fistula;
- periodontitis;
- flux;
- granuloma;
- cyst.
- In this case, the inflammatory process can result in a number of complications, so it is recommended to fight the infection with the help of antimicrobial drugs, rinsing with furatsilin or chlorhexidine, potassium permanganate or salt solution, as well as applying lotions.
Attention: Prevention is easier than cure!
Reasons for the development of lymphadenitis.
So, we have already found out that when teeth are removed, especially wisdom teeth, the lymph nodes become inflamed. This process is called lymphadenitis. The development of lymphadenitis in the head and neck area is promoted by:
- tonsillitis (inflammation of the tonsils);
- laryngitis (inflammation of the larynx);
- stomatitis (damage to the oral mucosa);
- gingivitis (inflammation of the gums).
What to do if the lymph node under the jaw is inflamed?
When the lymph node under the jaw becomes inflamed, the following symptoms occur:
- a significant increase in the size of the inflamed lymph node;
- when pressed, a dense movable tubercle is felt;
- severe pain in the gums and inflamed lymph nodes, which can spread to the head and neck;
- limited jaw movements;
- difficulty chewing and swallowing;
- general weakness, malaise;
- sleep disturbance;
- chills, increased body temperature up to 40 ◦C.
In such cases, the doctor identifies the degree of inflammation and prescribes appropriate treatment.
The dentist identifies the source of pathology by palpation (feeling with fingertips) of an enlarged lymph node, which is easily detectable. In some cases, pressure even causes pain. It is interesting that the skin first acquires a reddish tint due to increased blood flow in the area of inflammation, and then changes to bluish.
The body’s immune capabilities play a major role in activating the lymph nodes under the chin and in the lower jaw area. Lymphatic tissue, as the main part of the immune system, protects the body from pathogenic environmental factors. However, there are some diseases in which the immune system itself suffers. They are called autoimmune.
Such diseases include, for example, systemic lupus erythematosus, rheumatoid arthritis and serum sickness. With these pathologies, the protective function of the body is sharply reduced and, for example, if a child suffers from this serious illness, the lymph nodes under the lower jaw can increase even when baby teeth erupt.
What complications may arise?
Complications of an inflamed lymph node can be:
- angina;
In the photo on the left - healthy tonsils, in the photo on the right - inflammation of the tonsils - laryngitis or pharyngitis;
The photo shows dental flux
- laryngitis or pharyngitis;
In the photo on the left - healthy tonsils, in the photo on the right - inflammation of the tonsils
The photo shows laryngitis
- otitis.
Otitis. The photo shows an inflammatory process in the ear
They occur when pathogenic microflora spreads to other nearby areas. There is no way around this without a course of antibiotic therapy. In order not to struggle with complications later, it is necessary to diagnose and properly treat inflammation in a timely manner.
Complications of extraction
A separate group of complications are those that arise during tooth extraction. There may be, for example,
- alveolitis;
- flux;
- abscess;
- phlegmon;
- osteomyelitis.
The most insidious of them is considered to be alveolitis, or inflammation of the socket of an extracted tooth. It develops due to a dentist’s mistake or when the patient’s postoperative regimen is violated. The cause of the development of alveolitis is the destruction of a blood clot that should form at the site of the extracted tooth. Without it, the hole becomes as if unprotected and pathogenic microorganisms enter it. This is how alveolitis develops.
The photo shows alveolitis (inflammation of the socket of an extracted tooth)
In addition, the tooth socket may begin to fester. Severe pain, swelling, uncharacteristic discharge and bad breath occur. It is necessary to treat the inflammation, since with its further progression, nearby tissues suffer: gums, periosteum, mucous membrane and others.
To treat alveolitis, you must immediately seek medical help. The dentist will clean the hole, removing all foreign elements, and treat it and other foci of infection that may also arise in the oral cavity with an antiseptic solution.
Dentists also consider dry socket to be a complication of extraction. As mentioned above, a blood clot must form, which will promote tissue restoration and wound healing. If the hole remains dry, then the risk of infection in the wound increases, the pain intensifies and an unpleasant taste appears.
With wisdom teeth, things are even more complicated - due to their distant location, the patient cannot always see that the blood clot has disappeared. Therefore, he seeks help only when pain develops. In the case of a dry socket, the doctor places a cotton swab on the wound, soaking it with antiseptics and an antibiotic solution. That is, a cotton swab literally replaces a blood clot. Thanks to this, the hole is protected and its regeneration is accelerated. The cotton swab must be changed every day until the hole is completely healed.
Treatment of lymphadenitis
Diagnostic measures aimed at eliminating the problem include:
- dental treatment
- drug therapy
- special regime.
1. Dental treatment involves getting rid of the causes that cause the lymph nodes to enlarge. The doctor may suggest:
- professional teeth cleaning;
- treatment or filling of root canals;
- sanitation of abscesses;
- cleaning the hole;
- resection of damaged parts of teeth;
- replacement of fillings and crowns.
Attention: After appropriate treatment, the lymph nodes do not return to normal immediately. Their increased size can last up to 2 weeks. If enlarged lymph nodes cause pain and discomfort to the patient, he may additionally be prescribed physical therapy, as well as choose medications.
2. Drug therapy consists of the dentist prescribing medications when inflammation is detected. Typically it is:
- antibiotics to eliminate pathogenic bacteria;
- immunostimulants and multivitamin preparations (to speed up the body’s recovery);
- home treatments in the form of lotions and rinses.
In case of fever, antipyretic drugs are prescribed, and in case of severe pain, which often accompanies dental surgery, analgesics are prescribed. Thus, etiotropic (antimicrobial drugs) and symptomatic (to relieve symptoms) therapy is carried out.
3. To speed up the relief of inflammation, the patient should follow a special regimen. These include:
- reduction of physical activity;
- in case of severe lymphadenitis, even bed rest is recommended; the need to drink up to 3 liters of warm liquid (herbal teas, fruit drinks and plain water help well - they help get rid of intoxication caused by inflammation as quickly as possible);
- rinsing (you can rinse your mouth with a decoction of chamomile or calendula);
- salt lotions (a concentrated salt solution is prepared, a large piece of cotton wool or a cotton pad is soaked in it, and it is placed behind the cheek where the dental procedure was performed. The hypertonic solution will help the cotton wool absorb metabolic products during inflammation).
Patients will have to make extensive adjustments to their teeth brushing. If there is inflammation in the oral cavity and, as a result, in nearby lymph nodes, it will not be enough to use only a brush and paste. It is recommended to use an irrigator and dental floss, and after all these procedures, use a mouth rinse.
Caution: Buy a paste that contains antiseptics such as chlorhexidine, chlorine, silver and zinc. It will provide you with additional sanitation of the operated area and will not allow inflammation to develop.
The basic principles that ensure effective treatment of inflamed lymph nodes are:
- good timely diagnosis;
- bed rest;
- the use of alternative medicine methods in the form of lotions and rinses;
- antibiotic therapy;
- adequate sanitation of the oral cavity.
Attention: Treatment of inflamed lymph nodes should not be delayed, as pathogenic organisms can enter the circulatory system, which will cause sepsis.
What medications are prescribed?
Often, antibiotic therapy for enlarged lymph nodes and inflammation includes penicillin antibiotics, for example, Amoxiclav, Ampicillin or Amoxicillin. In case of allergy to antibiotics of the penicillin group, antibiotics of other groups may be prescribed. The most effective of them are macrolides and fluoroquinolones.
Attention: The course of antibiotic therapy should not exceed 5, and in some cases – 7 days. Carefully read the instructions prescribed for this antibiotic and follow them! To avoid developing resistance, follow your doctor's recommendations.
Stages of caries
There are 4 stages of carious lesions, each of which differs in the number and intensity of symptoms. The first (initial) stage is called the chalky (or white) stain stage, in which an area of demineralization forms on the tooth surface. Outwardly, it looks like a white speck, lacking shine. Under a microscope, you can see that in this area the enamel is rough, loose and porous. However, there is no carious cavity yet, so it is possible to cure the tooth without filling. The person is not bothered by any symptoms. Caries can be detected at the initial stage only during an examination.
At the second (superficial) stage, the carious process penetrates into the deep layers of the enamel, but remains within its limits, without spreading to the dentin. The white spot darkens and becomes brownish. The pathology can already be noticed independently if it develops on the outside of the tooth or fissures. Complaints appear: tooth sensitivity to sweets increases, sometimes to hot and cold, and there is discomfort when chewing food. However, it disappears as soon as the irritating factor is eliminated.
The third (middle) stage of caries is characterized by the penetration of the carious process into dentin. A brown or dark yellow cavity is formed, which is easy to see with the naked eye. Discomfort while eating is an almost constant concern, especially when a diseased tooth interacts with sour or sweet foods. The sensitivity of dental tissues to temperature changes also increases. The pulp is not yet involved in the pathological process, but this stage of caries can already be considered complex. At this stage it will not be possible to avoid preparation and filling. There is a risk of complications, possibly inflammation of the lymph nodes.
The fourth (deep) stage of caries is considered an advanced form of the disease, in which the carious cavity covers almost half of the tooth. It usually looks like a black hole with sharp edges. Pain occurs not only when eating, brushing teeth or temperature changes, but also at rest. The likelihood that caries will spread to nerve tissue and cause pulpitis is quite high. Moreover, the tooth may break into several parts, resulting in the need to remove it. This happens in cases where there is no treatment for the disease.
You can cure caries and save your tooth at any stage. But its loss is not the only complication of the carious process. There is a risk of developing other pathologies that are not dental.
Caries and other diseases
With caries, especially advanced ones, cariogenic microbes actively multiply in the oral cavity. There are several types of them, many of them are dangerous not only because they cause the development of caries. These bacteria can end up on the tonsils, get into the lymph nodes, soft tissues, pulp, etc. Caries can be complicated by pulpitis, periodontitis, periodontal disease, meningitis and chronic tonsillitis.
Such a combination of circumstances is facilitated by factors such as weak immunity and high susceptibility to certain pathologies. For example, people with chronic tonsillitis who do not treat caries are more likely to suffer from tonsillitis. There are other patterns that are determined by the interconnectedness of all processes occurring in the body.
In some cases, for example, with diabetes, cardiovascular diseases and problems with the digestive system, treating caries alone is not enough. Carious lesions and other oral diseases will constantly recur. For this reason, an integrated approach to treatment is required. Of course, caries rarely causes complications, but it is better to reduce the likelihood of their occurrence as much as possible than to then deal with the treatment of several pathologies.
Let's move on to the next question and find out why inflammation of the lymph nodes occurs, what role dental diseases, including caries, play in this.
Caries and submandibular lymph nodes - what is the connection?
The main function performed by the lymph nodes is to filter and protect a person from harmful microbes that enter the body from the external environment. The virus that enters it causes a reaction from the immune system, and it begins to resist the onslaught of the pathogenic agent, producing a large amount of lymph. Because of this, the size of the lymph nodes changes. In a normal state, it is almost impossible to see or feel them; they are no larger in size than a pea. In an inflamed state, the lymph nodes can be felt by palpation. Plus they start to get sick. If we are talking about the submandibular lymph nodes, then pain occurs when swallowing, as with a sore throat.
But inflammation of the submandibular lymph nodes develops not only due to viruses. There are many diseases that are also accompanied by an inflammatory process in the lymph nodes, that is, lymphadenitis. These include caries. Nodes with carious lesions, especially deep ones, become inflamed under the jaw and behind the ears. If the carious process develops on the right side, then the lymph node also begins to increase in size on the right.
Thus, lymphadenitis, which is not an independent disease, tells a person that pathology is beginning to develop and he needs to undergo examination. Many patients do the wrong thing when they begin to rub, massage, warm and lubricate the skin in the area of the inflamed lymph nodes. This can cause bacteria to spread even more and increase inflammation. To take treatment measures, you must first accurately determine the cause of lymphadenitis.
Function of the lymphatic system
The lymphatic system works closely with the circulatory system. With the help of a network of capillaries, vessels and nodes of the lymphatic system, various substances that are not able to penetrate the walls of blood vessels enter the blood.
So, before new particles enter the bloodstream, they are “tested” by the lymphatic system. If a certain element turns out to be potentially dangerous, it will be attacked by lymphocytes.
This filtration occurs precisely in the lymph nodes, where particles are brought with the lymph flow from the surrounding tissues. There are several types of lymphocytes in the human body and they all perform their function in protecting the body.
Lymph nodes are located in groups. They take on the task of protecting nearby tissues and organs.
What are the submandibular lymph nodes responsible for?
Lymph nodes on the lower jaw collect fluid from the intercellular space of nearby tissues and filter it. All infections that enter them are destroyed, provided that the person’s immune system works adequately. Cell waste products and decay products are also filtered out.
Important: one of the important tasks of the lymph nodes is the fight against cancer cells.
In the lymph nodes, new lymphocytes are produced and matured, which will fight infection in this area. Also in the lymphatic system of this area, harmful substances circulate from the blood to the lymph, and beneficial and nutrients are transferred from the lymph to the blood.
The correct functioning of the nodes in the lower part of the face is very important, because they have to deal with common diseases.
The most common diseases that lymphocytes of the submandibular space have to fight:
| Respiratory diseases | Oral diseases | Dental and gum diseases | Diseases of bones and joints |
| Tonsillitis | Stomatitis | Gingivitis | Inflammatory processes of the bone structures of the jaw |
| Laryngitis | Inflammation of the salivary glands | Periodontitis | Inflammatory conditions of the temporomandibular joint |
| Rhinitis | Advanced caries, often with multiple foci | ||
| Pulpitis |
Important: submandibular nodes can become inflamed as an independent phenomenon, without a primary extraneous factor.
Location of submandibular nodes
Submandibular lymph nodes, location and proximity to other lymph nodes
Lymph nodes on the jaw, that is, local formations of lymphatic tissue, are located along the path of the vessels of the lymphatic system, parallel to the course of the blood vessels. There are six to eight lymph nodes in the submandibular space.
They are located in a triangular zone under the lower jaw, slightly in front of the salivary gland, as well as in the thickness of its tissue. Lymph nodes surround the facial vein, located in front and behind it.
Vessels with lymph tend to the node from the following parts of the face:
- from the skin of the upper and lower lips;
- from the neck;
- from the chin and cheeks;
- from the outer part of the nose and its internal space;
- from the inner surface of the lower eyelid;
- from teeth, gums and palate;
- from the tongue and sublingual space;
- from all salivary glands;
- from the submandibular lymph nodes.
The video in this article and photos will clearly demonstrate which lymph nodes are responsible for which organs and tissues of the human body.
External features of nodes
Diagram of the structure of a lymph node
The lymph node in the jaw is a bean-shaped collection of lymphatic tissue. The nodes have different sizes.
In normal condition, the node has the following characteristics:
- it is soft to the touch;
- does not cause pain when touched;
- a normal size does not prevent the head from lowering to the chest, and the nodes are not felt;
- visually, the submandibular lymph nodes are not visible under the skin.
The lymphatic tissue itself is pink-gray in color. The nodes are arranged in groups and covered with a protective capsule of connective tissue.
Important: in the absence of acute inflammation in the surrounding tissues, only one, the largest submandibular node can be felt.
Lymph enters the node through incoming vessels - the gate, which is a hole on the upper part of the protective capsule. Along with the lymph flow, nerve fibers enter the node. Purified lymph exits through the efferent vessels.
The entrance and exit of lymph are arranged in such a way that each node includes 2-4 vessels, and at the exit there are only 1-2 vessels, and their diameter is larger than that of the incoming ones. The inner part of the node is equipped with parenchyma, a loose connective tissue layer in which lymphocytes of various types are based.
Gingivitis and lymph nodes
Gingivitis is an inflammatory disease of the gums that occurs due to the formation of plaque on the teeth and the spread of microbes. It often develops in people who do not take good care of their oral hygiene. Typical symptoms of gingivitis are itching and bleeding of the gums, swelling, and pain, especially when soft tissue comes into contact with hard objects, such as a toothbrush.
This pathology can occur in various forms. If the lymph node is inflamed, it may be ulcerative-necrotizing gingivitis. Its other signs are:
- strong pain;
- copious amounts of saliva;
- formation of ulcers;
- increased body temperature;
- loss of appetite;
- headache.
One of the complications of gingivitis if left untreated is periodontitis.
Prevention of inflammation of the lymph nodes
To avoid inflammation of the lymph nodes under the jaw, you must:
- strengthen the immune system (eat right, lead a healthy lifestyle and exercise);
- monitor oral and ear hygiene;
- correctly treat diseases of the throat and nose, colds and acute respiratory viral infections;
- be sure to visit the dentist 2 times a year for preventive examinations;
- avoid sudden hypothermia and overheating of the body;
- immediately treat damaged skin in the area of the face and neck with antiseptic agents.
If a disease is detected, you must immediately seek advice from a specialist in order to prevent an acute purulent form of inflammation, and begin treatment using the given traditional medicine as an auxiliary therapy.
Periodontitis and lymph nodes
Periodontitis is an inflammation of the connective tissue between the tooth root and the alveolar plate. One of the main reasons for the development of this pathology is untreated caries. If periodontitis is not treated, it takes on a purulent form, which is accompanied by an increase in body temperature to 38 degrees, severe pain in the tooth and the formation of an abscess from which pus can flow directly from the jaw. Also characteristic signs of purulent periodontitis are an increase in the size of the lymph nodes and painful sensations under the jaw during palpation.
Pathological conditions of the lymph nodes
Since the submandibular nodes perform a protective function, their increase indicates the occurrence of some problem in the tissues subordinate to the nodes.
Appearance of normal and inflamed submandibular lymph node
Important: when inflammation occurs, the lymphoid tissue reacts immediately, the nodes increase in the first hours of the disease.
Acute condition
In some cases, there is a slight increase in the size of the nodes. Such changes indicate the preparation of the lymphatic tissue to destroy a serious infection that begins to come from nearby tissues.
Tissue proliferation will lead to an increase in the number of lymphocytes, a condition called reactive lymphadenitis. Reactive changes in the submandibular nodes are most often provoked by inflammatory changes in the salivary glands.
Important: with purulent abscesses, the submandibular nodes are capable of growing and merging together; the neoplasms are painful for the patient.
Chronic condition
If the lymph node struggles for a long time with chronic inflammation of the tissues for whose health it is responsible, the acute condition transforms into a chronic one. Chronic lymphadenitis of the submandibular nodes occurs.
The submandibular node does not cope with its duties, its shape and condition undergoes changes:
- the size of the node increases;
- it becomes harder;
- touching the nodes is painful;
- the patient’s body temperature may increase;
- with severe inflammation, pain from the node will radiate to the ear area;
- swallowing movements become painful, until the patient completely refuses to eat;
- you can see the contours of the node on the skin, swelling and discoloration of the skin over the node are possible;
- with advanced inflammation, the skin over the node will have a bluish tint, this indicates the beginning of purulent processes in the tissues of the node.
These symptoms appear as the severity of the condition develops.
Strong changes are a consequence of untreated acute lymphadenitis. If at least one of the above symptoms appears, you should consult a doctor as soon as possible. If there is a strong increase in body temperature and increasing lethargy of the patient, you need to call a doctor at home; the cost of delay in such situations is too high.
Important: if left untreated, serious complications may occur—purulent changes and death of the submandibular node.
Condition during oncological processes
When the submandibular lymph node has to fight cancer cells, its tissue grows to increase the number of fighter cells. At first, the defense system copes successfully and cancer cells are destroyed.
With prolonged entry of pathological cells into the space of the node from the oral cavity or from the nose, there are too many of them, and the protective system can no longer cope. The oncological process begins to develop in the lymph node itself.
Pulpitis and inflammation of the lymph nodes
Pulpitis is an inflammation of the pulp - the nerve tissue inside the tooth. It often occurs in people with advanced caries at a deep stage. The following symptoms are characteristic of pulpitis:
- Acute pain that occurs both at rest and when the tooth is exposed to various irritants: food, brushes, water, etc. After eliminating the factor that provoked the pain, the symptom persists for some time, but gradually subsides. The pain is usually sharp and intense; it cannot be eliminated with analgesics.
- Headaches, pain in the ear area from the affected tooth, general malaise and increased fatigue. The pain may radiate to the temple and eyebrow.
- Increase in local and general temperature. In adults it can rise to 38°C, and in children even higher.
- Swelling of the submandibular lymph nodes, pain when swallowing and chewing food.
With pulpitis, as a rule, it is necessary to remove the diseased nerve, after which the tooth becomes dead and noticeably darkens.
Stomatitis and inflammation of the lymph nodes
Stomatitis is an inflammation of the oral mucosa that occurs against the background of infectious diseases, after burns, as a result of trauma, due to an allergic reaction, etc. Traumatic stomatitis is often diagnosed, for example, when the mucous membrane is injured by crowns or braces.
After an injury, bacteria enter the wound and cause inflammation, which is accompanied by:
- painful sensations;
- the appearance of rashes and ulcers on the mucous membrane;
- release of translucent exudate;
- the formation of a white film on the surface of the wound;
- inflammation of the lymph nodes;
- high temperature, chills and fever;
- hyperemia and swelling of the gums.
As a rule, stomatitis goes away without consequences. However, it can be complicated due to weak immunity, alcoholism or smoking. There is a risk that the disease will cause inflammation of the lymphatic system.
Purulent tooth abscess and lymph nodes
A tooth abscess is a purulent inflammation that is localized inside the tooth after pulp removal, in the periodontal area or under the gum. This pathology is characterized by shooting, throbbing pains that intensify with pressure and heat on the tooth. Inflammation of the lymph nodes under the jaw is possible, which is sometimes even noticeable from the outside: the patient develops a slight swelling in the neck. In rare cases, the abscess spreads to the bone tissue and causes swelling on the face. Some complain of migraines. The disease is complicated by the presence of other dental diseases, such as caries.
Other causes of inflammation of the submandibular lymph nodes
The lymph node is an important component of the entire lymphatic system, which performs many different functions. It is involved in maintaining immunity, protects against pathogenic microorganisms, transports nutrients, and removes harmful components from the body, for example, dead red blood cells and bacteria. Lymph nodes respond to many changes that occur in the human body. Almost any pathology or its complications can provoke lymphadenitis. We list the common causes of inflammation of the lymph nodes:
- Infectious diseases: chronic tonsillitis and tonsillitis, otitis, sinusitis, mumps, alveolitis, streptococcal infections.
- Pathologies that strongly affect the state of the immune system: lupus, HIV and AIDS, leukemia, arthritis, tuberculosis.
- Toxoplasmosis is a parasitic disease that often occurs in a chronic form and is accompanied by symptoms such as low-grade fever, swollen lymph nodes, decreased performance due to fatigue, headache, etc.
- Diseases that usually occur in childhood: chickenpox, measles, mumps. They affect the state of the entire lymphatic system.
- Tumors. If the lymph node is inflamed, but the person does not notice any other symptoms, has not been injured and does not suffer from chronic diseases, then it is necessary to undergo a systemic examination. Lymphadenitis can be the initial symptom of oncology.
If your lymph node is inflamed, do not try to eliminate the inflammation using folk remedies. Thus, the inflammatory process may be a consequence of the development of a bacterial infection, which must be treated with antibiotics. Many people apply cold or, on the contrary, hot lotions to the swollen area, and this causes even more active growth of bacteria. As a result, complications may develop. There are many causes of lymphadenitis, so deciding on self-treatment is dangerous.
Causes of inflammation
The structure of the lymphatic system is very complex and intricate, but the mechanism of its operation is simple: when an infection enters the body or a failure of internal organs is caused by the growth of new cells or the synthesis of an atypical protein, the brain signals this to the nearest lymph nodes, which immediately react with increased production of lymphocytes that attack atypical cells and removing their waste products from the body using lymph.
At the same time, the lymph nodes working at an increased rate may become enlarged, and if the problem is serious, an inflammatory process may develop, accompanied by severe pain and suppuration. The causes of inflammation of the lymph nodes under the jaw are:
- chronic bacterial infections of the upper respiratory tract or ear canals;
- ARVI, diseases of the nose and throat: otitis media, tonsillitis, laryngitis, sore throat and others;
- dental pathologies: purulent abscess, dental flux or cyst, alveolitis, oral wounds and deep caries;
- endocrinological diseases;
- parasites;
- piggy;
- chicken pox;
- infected wounds located near the jaw;
- neoplasms: both benign and malignant;
- diseases of the immune system.
According to statistics, inflammation of the lymph nodes under the jaw in a child is caused in 60% of cases by diseases of the teeth and bone tissue of the jaw, in 30% by inflammation of the upper respiratory tract and ENT organs, and 10% of cases are due to all other causes.
What are the symptoms of inflammation of the lymph nodes?
The submandibular lymph nodes become inflamed against the background of other pathologies, each of which has its own specific symptoms. We list the most common signs of lymphadenitis:
- sudden enlargement of the lymph nodes under the lower jaw, their pain when pressed and hardening;
- first slight and then severe redness of the inflamed areas, they become burgundy and sometimes bluish;
- swelling at the site of inflammation on one or both sides, depending on the etiology of lymphadenitis;
- sharp and short-term attacks of pain that radiate to the ear, temple or eyebrow;
- discomfort when chewing food, increased pain during swallowing;
- inflammation of the oral mucosa, which is accompanied by redness and increased sensitivity;
- increased body temperature, general weakness, sleep disturbance, fatigue.
To make a diagnosis, it is important to determine not only the cause, but also the type of lymphadenitis, since the clinical picture of each of them may be different.
Types and forms of submandibular lymphadenitis
Inflammation of the lymph nodes occurs in acute or chronic form. The first is characterized by high intensity of symptoms, the disease develops quickly, and it is almost impossible to ignore it. The patient suffers from pain, fever and other symptoms. Immediate medical intervention is required, especially if the pain increases and cannot be relieved with painkillers.
Chronic submandibular lymphadenitis is characterized by a long incubation period, during which a person may not be bothered by any symptoms. In such cases, he usually does not see a doctor, which allows the pathology to progress. An exacerbation may occur at any time, which will require urgent diagnosis and treatment.
Depending on the nature of the contents of the lymph nodes, inflammation can be purulent or non-purulent. The first occurs with great complications and is accompanied by an increase in temperature, the second - in a milder form. Based on the causes of inflammation, it is divided into simple, hyperplastic and destructive. Downtime is accompanied by classic symptoms and tends to become chronic.
Hyperplastic submandibular lymphadenitis is a more complex type of inflammatory process, which is accompanied by redness of the skin and significant enlargement of the lymph nodes. Pathology covers not only the node, but also the tissues surrounding it.
Destructive lymphadenitis is characterized by the destruction of lymph nodes, as well as adjacent tissues, which occurs against the background of a purulent process. This is the most dangerous type of disease that requires urgent treatment.
In most cases, the type and form of inflammation of the lymph nodes is determined by etiological factors and the patient’s state of health, his immunity. Let's consider how it is possible to identify the cause of the inflammatory process in the lymph nodes.
Symptomatic therapy
Before prescribing special treatment, rinsing with antiseptic solutions is effective in order to more quickly restore the size and density of the submandibular lymph nodes in case of ARVI, sore throat, and other inflammatory processes in the oral cavity. In the presence of combat syndrome, it is possible to take analgesics. In other cases, therapy is selected only after the causes of the condition have been established. The combination of lymphadenopathy with fever, rapid deterioration in health, headache, or detection of tumor formations in the head area is an indication for emergency medical attention.
Diagnosis of submandibular lymphadenitis
You can determine that inflammation of the submandibular lymph nodes has begun on your own. It is enough to simply feel the areas of the neck directly under the lower jaw, closer to the ears. Normally, the nodes are almost impossible to palpate; they are small, have a dense structure, do not hurt and move easily under the fingers. If you notice a change in the structure of the lymph nodes, or feel discomfort or pain during palpation, you should consult a doctor. It is impossible to independently identify the cause of inflammation. First, you can go to a therapist. After the initial examination, which includes examination and collection of tests, he will refer you to another specialist: otolaryngologist, phthisiatrician, surgeon, infectious disease specialist, immunologist or dentist. If caries is suspected, the doctor will diagnose using the following methods:
- Coloring. A solution is applied to the tooth enamel, which turns the areas of demineralization purple.
- X-ray. Photographs of the teeth or the entire jaw are taken, from which the location and extent of the caries process can be determined.
- Laser diagnostics. This method is the most modern. It allows you to accurately identify the extent of the spread of pathology.
Based on the results of the examination, treatment is prescribed. First, we will describe the general features of the treatment of submandibular lymphadenitis, after which we will tell you what to do if the lymph nodes become inflamed due to caries.
The main directions of treatment of submandibular lymphadenitis
The direction of treatment is determined by the etiology of the inflammatory process. If the disease is infectious, antibiotics, antifungal and anti-inflammatory drugs, sprays and ointments are prescribed. Purulent inflammations are treated promptly under local anesthesia. The doctor cleans the lymph node of purulent masses and installs drainage. After this, the patient is prescribed appropriate medications.
Often, after eliminating the underlying pathology that led to inflammation of the lymph nodes, all its symptoms, including lymphadenitis, disappear. If this does not happen, the patient undergoes a course of physical therapy. Immune-boosting therapy may be needed. The patient needs to stop smoking, start eating right and taking vitamins.
Lymphadenitis is inflammatory changes in one or a group of lymph nodes. Lymphatic formations of all areas of the body can be affected. Lymphadenopathy of the cervical and submandibular region is most often observed in medical practice. This disease usually has a secondary genesis. If the inflammation becomes purulent, then the infection may break through with the development of abscesses and phlegmons. From the submandibular region, inflammation can move along anatomical formations to various sections. Such situations can be life threatening.
A huge number of diseases can indirectly or directly lead to inflammation of the lymph nodes, especially infectious diseases. The human lymphatic system belongs to the body's immune system and is represented by lymphatic vessels and lymph nodes. Immune cells circulate in this system. Lymph (fluid that flows from organs and tissues through lymphatic vessels to the lymph nodes) carries particles of pathogenic microorganisms for recognition by immune cells. In the lymph nodes, preparation and activation of immune cells (mainly lymphocytes) take place, which migrate to the pathological focus, destroy bacteria and other pathogens, resulting in recovery. There are other possible causes of lymphadenopathy: tumors of the immune system, systemic diseases, helminthic infestations, tumor metastases and others, but they are much less common and their main symptoms dominate over enlarged lymph nodes (which, by the way, is not always inflammatory in nature). Most often, inflammation of the regional lymph nodes of the submandibular region is odontogenic. This means that the main source of infection is the inflammatory process in the oral cavity. These are most often dental problems - periostitis, periodontitis, periodontitis, pulpitis. Inflammatory diseases of the respiratory system lead to enlargement of the lymph nodes in the cervical region - parotid, tonsillar, occipital and others. There are catarrhal and purulent forms of inflammation. Depending on the type of process, treatment tactics will change.
Having discovered such changes, patients usually first turn to a therapist. However, as mentioned earlier, if the inflammation is localized specifically in the submandibular nodes, one should assume an odontogenic nature and consult a dentist.
The clinical picture may differ depending on the location of the primary lesion. Lymphadenitis itself is accompanied by palpable formations in the submandibular region. They will have an elastic consistency, and painful sensations occur upon palpation. There may be discomfort while eating, but the general condition usually does not change. Such symptoms are characteristic of the catarrhal (serous) process. If inflammation progresses, the lymph node can be completely destroyed by a purulent process. In this case, the skin over the node becomes hot to the touch, turns red, and body temperature rises depending on the type of inflammation (an abscess or phlegmon develops). strong painful sensations of a tugging or pulsating nature occur already at rest.
Lymphadenitis can be diagnosed by inspection and palpation of the affected area. Depending on what the doctor suspects as the cause of the inflammation, appropriate diagnostic methods will be prescribed. Be sure to conduct an examination of the oral cavity: inflammatory changes in the teeth, oral mucosa, tonsils, pharynx, larynx and other organs can be noted. The dentist may prescribe a panoramic X-ray or an X-ray examination of the sinuses. All patients are shown a general blood test. In the absence of pathology on the part of the dentofacial apparatus, a consultation with a therapist or otolaryngologist is indicated. In some situations, consultation with an oncologist is required.
Additional methods include smears from the oropharynx to determine the causative agents of the infectious process, biochemical blood tests, ultrasound of regional areas (will reveal an increase in nodes inaccessible to palpation), various methods of visualization of the head and neck organs (for the presence of oncological pathology), puncture biopsy of the affected lymph node with cytological and histological examination and other methods.
Treatment depends on the type of inflammation. In the case of a purulent process, surgical treatment is indicated - opening and draining the lesion. If the inflammation is catarrhal, then a dentist or otolaryngologist treats the underlying disease (pharyngitis, tonsillitis, laryngitis, periodontitis, periostitis, pulpitis and others). In such a situation, the lymph nodes are not opened under any circumstances, but conservative therapy is carried out: UHF therapy, ointment dressings, heating using a dry heat source.
Treatment of submandibular lymphadenitis with caries
Caries is treated with various methods depending on the stage. At the first stage, in which you only need to eliminate the white spot, remineralization of the tooth surface is carried out. With the help of special preparations, the enamel is saturated with minerals - calcium and fluorine. Therapy is prescribed in a course lasting 5-15 procedures. For home use, the patient is prescribed hygiene products that help restore enamel and the balance of microelements in the oral fluid. Such means include:
- toothpastes: Marvis Orange Blossom Bloom, Dentissimo Complete care, Apadent Perio;
- gels: Stomysens® Desensitizing Repairing Treatment 4, DRC ROCS (ROCS) Medical Minerals, Dental Resources Inc Sorbet Revive;
- rinses: Vivax “Remineralization”, CURAPROX Perio Plus Forte chx 0.20%, Biorepair Delicate Gums Mouthwash.
If a carious cavity has formed on a tooth, then remineralization will not help; filling is necessary. First, the dentist cleans the hole from necrotic tissue and food debris, after which he places a protective gasket and fills the cavity with filling material. If caries is complicated by pulpitis, the nerve has to be removed.
After treatment of the carious process, the inflamed lymph node should return to normal. If this does not happen, it is necessary to re-diagnose. Perhaps the inflammation is not a consequence of caries, but of another disease.
More often, the submandibular lymph nodes become inflamed during the chronic course of the carious process, in which slow tooth destruction is observed. It is not accompanied by severe symptoms, but with exacerbations or the presence of certain factors, inflammation of the lymph nodes occurs.
What not to do if you have swollen lymph nodes
On the one hand, lymph nodes become inflamed quite often, and often the inflammation goes away on its own without any treatment, so many people do not take this problem seriously. In most cases, it really does not cause any consequences.
On the other hand, submandibular lymph nodes can make themselves felt in severe pathologies that cannot be left without treatment. Doctors recommend not delaying a visit to the hospital if inflammation and pain do not go away within 2 days or occur systematically. Experts also advise:
- Do not try to cure inflammation on your own. It is not possible to find out what caused it at home. In some cases, this cannot always be done quickly and in a medical institution, as a result of which the patient undergoes many examinations. Attempts to cure inflammation with folk remedies can lead to the development of complications.
- Do not heat inflamed lymph nodes. They cannot be heated even in the absence of elevated temperature. Warming up can increase swelling and pain. With the bacterial nature of lymphadenitis, heat stimulates the proliferation of bacteria and causes the infection to spread through the lymphatic system.
- Do not apply ice to the sore area. Cold is contraindicated in inflammatory and infectious processes, since hypothermia can greatly aggravate the situation and lead to even more severe inflammation.
However, a person can take certain measures on his own. You need to switch to proper nutrition, quit smoking and alcohol and make an appointment with a doctor. To reduce the risk of developing inflammation of the lymph nodes, treat all diseases in a timely manner, visit the dentist every six months, exercise and carefully observe hygiene rules.
How to treat inflammation of the lymph nodes under the jaw
First, it is necessary to identify the disease that led to inflammation of the lymph nodes under the jaw and begin its treatment. As a rule, after treatment of the underlying disease, the inflammation also disappears: the node gradually decreases in size and stops hurting. But you can also speed up the healing process if, together with the main treatment, you use measures that improve the functioning of the entire lymphatic system . Such measures include:
- bed rest or restriction of physical activity;
- eliminating hypothermia and overheating, especially in the neck and head area;
- compliance with the drinking regime (you need to drink a lot of warm liquid);
- exclusion of sweet, spicy and salty foods from the diet;
- use of traditional medicine: infusions, decoctions, tinctures, juices and lotions.
To treat inflammation of the lymph nodes under the jaw and restore the lymphatic system, the following folk remedies are used internally:
- Echinacea . Mix pharmaceutical tincture (10-15 drops) with water (50 ml) and take orally.
- Echinacea tea . Dried echinacea herb can be brewed as tea. To prepare tea, take 1/2 teaspoon of crushed raw materials and pour hot water (200-250 ml cup). Wrap the tea and let it brew for half an hour. Drink this tea in the morning.
- Echinacea root syrup . Pour crushed echinacea root (4 tablespoons) with water (400 ml) and cook over low heat for 20-25 minutes, after a while add mint (50 grams) to the pan and cook for another 5 minutes. Add honey (50 grams) to the cooled, strained broth and stir. Take 20 grams of the resulting syrup daily.
- Licorice root decoction. Pour crushed licorice root (30 grams) with hot water (200 ml) and simmer in a water bath for a quarter of an hour. Remove the broth from the heat and let cool completely. Filter and squeeze the raw material through a bandage. Bring the broth to its original volume by adding boiled water. Drink 1/3 of a cup 30 minutes before main meals.
- Infusion of knotweed herb . Pour dried knotweed herb (1 tablespoon) with hot water (300 ml) and leave for 20 minutes. Take the entire portion of the resulting filtered infusion three times a day, half an hour before main meals. The time for taking knotweed herb infusion is a week, and then you need to switch to taking horsetail herb infusion, prepared in the same proportions as in the previous recipe with knotweed herb. The course of using horsetail infusion is also a week according to the same dosage regimen. The general treatment regimen with weekly alternation of herbal infusions is 2 months.
- Herbal decoction . Mix yarrow and oregano herbs, nettle leaves and hop cones (take all ingredients in a tablespoon), add horsetail herb (3 tablespoons) and mix the collection. Separate a tablespoon of the mixture, fill it with water (300 ml) and leave the product to simmer in a water bath for 15 minutes. Take the cooled, strained broth, 10 ml three times a day, 30 minutes before main meals. A decoction of yarrow herb is used to increase heart rate at home.
To relieve inflammation of the lymph nodes under the jaw, the following traditional medicines are used externally:
- Dandelion juice. Grind fresh dandelion grass into a pulp and squeeze the juice out of it. Soak a piece of bandage with the resulting juice and apply it to the inflamed site for 2 hours, securing it with a bandage or plaster. Use dandelion juice twice a day for 3-5 days in a row.
- Fresh mint leaves . Wrap mint leaves in cheesecloth and crush to release juice. Apply the product to the affected area for 2 hours, securing with a bandage. Carry out the procedure 2 times a day, each time preparing a new bandage. Peppermint tea is used to treat loose stools in adults.
- Chicory roots . Pour boiling water over crushed chicory roots (the amount should be enough to cover the surface of the lesion) until they are just covered with water, and let stand for 20-30 minutes. Crush the steamed roots, drain the liquid, and wrap in gauze or bandage. Apply the product to the affected lymph node, cover the top with film and secure with a bandage. Keep the compress for 2 hours. Carry out the procedure twice a day.
- Walnut leaves . Grind fresh or dried walnut leaves and steep them in boiling water until just covered. Let the product sit for 20 minutes. Soak the bandage with the resulting infusion and wrap the steamed leaves in it. Apply the product as a compress for 2 hours twice a day.
- Aloe juice ointment. Squeeze the juice from a three-year-old aloe leaf (a tablespoon) and mix it with goose fat (30 grams). Apply the resulting ointment to the site of inflammation 2-3 times a day.
- Vinegar 9% . Dilute 9% table vinegar in half with water and apply the product to the inflamed area for 1 hour, 2-3 times a day.
- Celandine juice infused with alcohol . Grind fresh celandine grass into a pulp and squeeze out the juice. Mix the resulting juice (1 tablespoon) with alcohol (100 ml) and leave in a warm place overnight. Moisten a bandage or cloth in the resulting tincture and apply to the affected area until completely dry.
- Saline dressing . Dissolve salt (2 teaspoons) in slightly hot water (a glass). Moisten the bandage in the resulting solution and apply to the affected area until completely dry twice a day. Saline solution is also used to rinse the nose to treat runny nose in children.