From the history
The mention of the first means for cleaning teeth dates back to the 3rd-5th millennium BC. The ancient Egyptians ground eggshells, pumice, ashes of ox entrails, and myrrh and prepared a product from this, which was the progenitor of tooth powder. The Greeks, Romans and Persians improved the recipe by adding shellfish shells ground into powder, crushed chalk, honey, and dried plants. The Slavs contributed to the development of dentistry by starting to brush their teeth with birch charcoal. Powders and pastes, more or less similar to modern ones, appeared in Great Britain only in the 18th century, when their use was considered the prerogative of the nobility.
Modern people are luckier - everyone can choose a product to suit their taste and budget or for medical reasons. Nowadays there are toothpastes that are not only hygienic, but also therapeutic and prophylactic, which include special additives. Let's look at them in more detail.
Hollywood smile. How to whiten teeth at home? More details
Best toothpaste
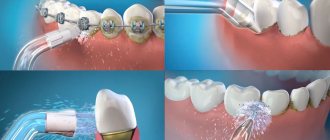
Which toothpaste is better? Definitely one that meets a person’s needs and suits his indications. Until recently, the main task of toothpaste was to help the brush clean teeth from plaque. Today, modern manufacturers of hygiene products have expanded its functionality and began to offer special medicinal toothpastes, both complex and for targeted solutions to specific problems. Today you can find tubes not only for the prevention of caries, but also for bleeding gums, against the formation of tartar, paste for implants or smoker’s plaque, for fresh breath or restoring the pH balance of the oral cavity, as well as for much more. But, in fact, all pastes are divided into several varieties, which we will consider.
Hydroxyapatite
It’s not for nothing that this supplement stands out. The fact is that tooth enamel consists of 96% of this mineral, and dentin (the hard, main part of the tooth) consists of 70%. The pastes use an artificially synthesized analogue of a natural substance, which is completely identical to it. Once on the surface of the teeth, it solves the following problems:
- fills microcracks, restoring the integrity of the protective shell;
- resists incipient caries, reduces the risk of its occurrence;
- reduces sensitivity to temperature stimuli;
- have a slight whitening effect.
The pioneer in this direction is the Japanese company Sangi, whose scientists managed to synthesize artificial hydroxyapatite and create a toothpaste containing it.
Article on the topic
What are the dangers of chipped teeth and what to do about them? Dentist advice
Competition "bio/mol/text"-2013
This article was submitted to the competition of popular scientific works “bio/mol/text”-2013 in the “Best Review” category.
The competition is sponsored by the visionary Thermo Fisher Scientific. The sponsor of the People's Choice Award is Helicon.
Modern science sets one of its main goals to extend the duration of human life. New methods of treating diseases are being developed, the lives of the elderly are being made easier, many diseases that were previously considered incurable have been almost completely defeated by humanity. However, some age-related changes are genetically embedded in the body, and it is almost impossible to combat them using conventional methods.
Bone diseases occupy one of the first places in the ranking of the most common problems among older people. Bone mass loss increases with age. Women especially suffer from this - due to the more active leaching of calcium cations from the body, which serves as the basis of our skeleton. Bone loss can reach 40% in women over 70 years of age [1]!
This disease is called osteoporosis. The bones affected by it become fragile, having difficulty coping with the load placed on them. In the event of a fracture, such a bone will take much longer to heal than a healthy one. As mentioned above, the main reason for such changes is the gradual leaching of calcium from the body. Throughout our lives, two equilibrium processes occur in our body: the continuous formation of new bone tissue and the resorption (dissolution) of old bone tissue. With old age, the balance shifts towards resorption, and new tissue simply does not have time to take the place of dissolved tissue. And excess calcium cations, which is the main product of this process, are eliminated from the body naturally.
What is a human bone? Figure 1 schematically shows the structure of human bones. The base consists of a composite (a material made up of other materials and having properties different from those of the “parents”), which are crystals of non-stoichiometric hydroxylapatite with the chemical formula:
Ca10−x−y/2(HPO4)x(CO3)y(PO4)6−x−y(OH)2−x,
and long chains of collagen protein [2]. This composite is a spatial matrix filled with osteoblasts, osteoclasts, macrophages, a network of capillaries and other things, but within the framework of this article we will not consider the structure of bone in more detail.
Figure 1. Structure of tubular bone. It is clearly visible that the bone consists of successive layers: the outer one - the periosteum - then there is compact bone substance, spongy bone substance and yellow bone marrow.
“Structure of a long (tubular) bone”
There are different ways to simulate bone tissue using different materials. For this, ceramic, metal, plastic and even glass prostheses are used, but all of them are far from ideal. Such a replacement cannot be called a complete replacement. One of the problems, for example, is the difference in the strength of real and artificial bone. If the material is too strong, then the load to which this part of the skeleton is exposed begins to be distributed unevenly. The strongest part “takes” the lion’s share of the load, and excessive destruction of bone tissue occurs at the junction of the prosthesis and the real bone. Therefore, the artificial bone must match the mechanical properties of the replaced part of the skeleton as closely as possible.
Obviously, the material should not be toxic and cause the death of the tissue surrounding the prosthesis. But many materials, even though they are not toxic to humans, begin to become covered with connective tissue when they enter the body. This is how the body isolates the foreign object. The thickness of such a capsule, also called a scar, is used to judge the biocompatibility of the material. Ideally, artificial material should fuse with the body and not leave any traces. Such material is called bioactive. An example is the glass material BIOGLASS [3]. This “glass” is used both for attaching implants made of other materials and as an independent bioactive material for simulating bone. It is used mainly in dentistry. When an implant enters the body’s environment, bone tissue cells “grow” into its surface layer, firmly connecting the implant to the bone. To increase the number of such bonds and, therefore, the strength of the connection, it is necessary to increase the surface area of the material. The more porous it is, the stronger the bond between the bone and the artificial element [4].
Thus, complete replacement of bone with artificial material is undesirable. The most preferred way to regenerate bone tissue today has been to replace the damaged part of the tissue with a bioactive prosthesis, which will fuse with the surrounding tissues, then accelerate natural regeneration and gradually dissolve without a trace, leaving new tissue on the bone defect.
Figure 2. Individual prosthesis of a fragment of the lower jaw for a patient with sarcoma of the lower jaw. The prosthesis is made of polymer and hydroxyapatite.
Traditionally, hydroxylapatite is used for these purposes in orthopedics. Stoichiometrically, hydroxylapatite (hereinafter, for brevity, we will call it HAP) is the closest in composition to the mineral component of bone (compared to other calcium phosphates). Its formula:
Ca10(PO4)6(OH)2.
Later in the article we will tell you what the advantages and disadvantages of this material are compared to others.
Fluorine-containing components
There are several of them: tin fluoride, amino fluoride, sodium monofluorophosphate, sodium fluoride. The latter is most common as an additive in toothpastes. Numerous studies and practical experience over several decades have proven the effectiveness of this compound in preventing caries and maintaining enamel resistance to acids. However, in recent years there has been a split in the scientific community regarding the advisability of using such pastes. The fact is that fluorine compounds in high concentrations are very toxic, which is fraught with abnormal bone mineralization, kidney failure, liver inflammation, impaired secretion of insulin and thyroid hormones, and general poisoning. It is impossible to get such doses by simply brushing your teeth, but opponents of fluoride-containing products appeal to the fact that in some regions people receive fluoride from other sources (mainly from water) and it can accumulate in the body. In general, the benefits of using fluoride-containing pastes do not outweigh the potential harm to the body, so they should be used with caution and for a short time without a doctor’s prescription.
Reliable shield. Which toothpaste should you choose for children? More details
How to give new properties to GAP?
Not all properties necessary for prosthetics are inherent in hydroxyapatite by nature. However, some therapeutic effects can be added to the materials by complicating the composition of the composite with additional substances. However, this is not very convenient, as it will complicate clinical trials, and it is much more difficult to develop such material. But progress can be made and unique properties obtained by slightly modifying the composition and introducing impurities of other cations and anions into the hydroxyapatite lattice. By changing the composition of ceramics, you can vary its strength, size and shape of crystallites, dissolution rate and many other parameters.
Calcium phosphate ceramics can be modified by introducing many components. The possibilities for choosing such a modifier (doping component) are quite wide: depending on the size of the replaced ion, you can change the composition by either fractions or tens of percent. For example, low concentrations of silicon ions activate bone tissue regeneration, playing the role of an antigen for the corresponding cells.
Of interest, for example, are the biological properties of lanthanide cations [7]. The use of lanthanide ions in oral medications is limited by their low ability to pass through the walls of the stomach and intestines. To improve the availability of lanthanide cations, lipophilic shells of complexes can be used. Substances that can penetrate cell membranes are called ionophores. (You can read more about them in the article “Unknown peptides: the “shadow” system of bioregulation” [8].) Such a shell will allow them to penetrate the cell membrane. This method of delivering ions to osteoblasts could become a fundamentally new approach to the treatment of a number of bone diseases.
Due to their high affinity for phosphates, lanthanides are firmly bound in the structure of minerals that form the basis of bone tissue, without disturbing their structure. Lanthanides can even replace calcium in bones, while simultaneously suppressing the development of cells responsible for the rupture and resorption of bone tissue. This ability to “mimic” the functions of calcium ions allows lanthanides to be considered as a component for the therapy of bone diseases.
The partial exchange of calcium cations for lanthanide cations opens up broad prospects for a number of different materials based on calcium phosphates. With the help of lanthanides, it is possible to influence the physical properties of the resulting ceramics, regulate the rate of resorption, and even use this material as a drug for the treatment of osteoporosis.
In practice, HAP is used in the form of cement or porous inlays to fill cracks, cavities and other defects in orthopedics and maxillofacial surgery. In the form of a film, it is applied to prostheses made of other materials (most often metal or polymer) to reduce the risk of rejection and better fixation due to the formation of new tissue around the prosthesis. As a rule, these are hip joint prostheses and various dentures.
Of course, artificially synthesized hydroxyapatite is far from ideal, and it cannot yet be used as an implantation material to create full-fledged prostheses for large bones or joints. But the use of its remarkable properties, such as relatively simple regulation of the composition and morphology of crystallites, bioactivity and the ability to accelerate natural regeneration, makes it possible to make drugs based on it for the correction and prevention of bone defects right now. This means that in the foreseeable future we will be able to significantly simplify the treatment of osteoporosis, speed up the healing of fractures, and, perhaps, even return lost limbs using artificial bones.
Anti-caries additives
The most common:
- Calcium glycerophosphate. Calcium salt, designed in toothpastes to compensate for the deficiency of this microelement in dental tissues. It is possible to saturate the enamel in adulthood with the necessary microelements only locally, so brushing teeth with a paste containing calcium glycerophosphate will be many times more effective in this regard than using specialized medications. In addition, the substance activates anabolic processes and strengthens the crystal lattice of the enamel.
- Xylitol. This is a natural sugar substitute, which in addition has properties that are beneficial for teeth and gums. The main benefit is the elimination of bacteria in the oral cavity that are not able to process the substance. As a result, there is a pronounced anti-caries effect (everyone knows that caries appears due to the fault of bacteria that live in large numbers in the human oral cavity). In addition, xylitol helps strengthen enamel and gums, has antifungal activity, enhances salivation and increases the protective properties of saliva.
- Enzymes. The most applicable are mutanase, invertase, peroxidase, protease, carbohydrase. The anti-caries effect is due to the same properties as the previous substance - enzymes fight pathogenic microflora in the mouth. At the same time, they do not damage the mucous membranes, have a beneficial effect on periodontal tissue, dissolve soft plaque and soften hard plaque.
The effectiveness in the fight against incipient caries and the preventive effect of elements from this group are lower than, for example, sodium fluoride, but they do not pose a threat to the body.
Article on the topic
Are yellows better than whites? Seven myths about teeth
Anti-inflammatory substances
Aluminum lactate, triclosan, chlorhexidine, biosol are names that can most often be found in descriptions of pastes that have antimicrobial and anti-inflammatory properties. The effectiveness of these elements is quite high, but it should be understood that, together with pathogenic microflora, they destroy or reduce the activity of beneficial ones. For this reason, their prolonged uncontrolled use may have a negative impact on health in the long term. Such pastes, like all therapeutic and prophylactic pastes, should be used after consultation with a dentist and according to his instructions.
Ideally, therapeutic and prophylactic pastes with additives should be used on the recommendation of a dentist, who will select the appropriate product for each specific case and tell you how and how much to use. In addition, it should be understood that such pastes are not an alternative to professional hygiene, remineralization and lamination at the dentist, but only an effective addition to these procedures.
There are contraindications, you should consult your doctor