October 27, 2019
Many people are interested in whether a tooth can hurt their ear. Indeed, such a situation can easily happen, because everything in the body is interconnected. And we should not forget the fact that almost the entire maxillofacial apparatus is covered by branches of the trigeminal nerve, which can react to any disturbance with inflammation or pain. And because the tooth hurts the ear, the clinical picture may be unclear, so some patients are in no hurry to visit the dentist, which only aggravates the course of the disease, believing that the cause lies elsewhere. The editors of the UltraSmile.ru portal offer for consideration the most common situations when these two phenomena - ear and tooth pain at the same time - are interconnected.
Often pain in the tooth and ear are interrelated
Comments
I can’t understand, my tooth hurts and that’s why it radiates into my ear. Or, on the contrary, the ear hurts and it hurts the tooth. Which doctor is better to go to?
Nathan (02.11.2019 at 16:37) Reply to comment
- Dear Nathan! After reading our article, you should have realized that pathology can be caused by completely different reasons. Only a doctor after examination can determine the true one. In your case, it is recommended to first visit two specialists: a dentist and an otolaryngologist. If these doctors do not find anything, then further examination by an orthopedist or neurologist may be required.
Editorial staff of the portal UltraSmile.ru (09.11.2019 at 09:14) Reply to comment
Ear and tooth hurt. I did an independent examination in front of the mirror, all the teeth in my mouth were intact, there were no holes. I haven’t gotten my ticket to the ENT specialist yet; in our city it’s a big problem to get to see this specialist for free. To avoid pain, I take pills, my grandmother also advises warming my cheek, supposedly this helps. Is it possible to do this?
AlisaV. (11/26/2019 at 12:19 pm) Reply to comment
- Dear Alisa! If you have not noticed any pathologies externally, this does not mean that you do not have dental problems. For example, it is almost impossible for the patient to notice a cyst in the early stages on his own. Therefore, it is still recommended that you go to the dentist. As for warming up the cheek, this is strictly forbidden, because... if the inflammatory process is to blame, then the infection, when warmed up, can spread through the bloodstream to the surrounding tissues, and your condition will only worsen.
Editorial staff of the portal UltraSmile.ru (01.12.2019 at 09:21) Reply to comment
Write your comment Cancel reply
Why does toothache radiate to the ear?
The cause of illness does not always lie in viruses, as a result of the flu. The culprit may be a growing unit or the removal of a masticatory organ. Discomfort on the left side is associated with advanced caries or periodontal disease when the same side is affected. Through the canals of the teeth, bacteria quickly penetrate into the ENT organs. The provoking factors by which oral diseases provoke ear tingling or lumbago are varied.
- Pathologies of the extreme molars of the upper jaw affect the hearing aid, since their roots are located nearby.
- Inflamed soft tissues and nerves of abnormal units have an adverse effect on the ears. Ripple, which intensifies when pressing on the diseased crown, indicates problems in the oral cavity.
- Pathological eights, which have a powerful branched root system, can negatively affect the hearing aid. For example, wisdom tooth decay can cause tingling in the ear. When third molars grow abnormally, soft tissues and facial muscles become inflamed.
- Complications to the hearing organs are caused by injuries to the crowns, roots or soft tissues of the oral cavity. In such a situation, swelling occurs.
- Removal of molars when the surgical socket swells and festers.
- The ear canals suffer from cysts of the masticatory organs.
- Inflammation of the nerve fibers of the tooth.
- Malocclusion.
- When the anatomical integrity of the crowns or roots on the right side is damaged, there will be a tingling sensation in the ear on the same side. Mechanical impact aimed at the soft tissues of the oral cavity or the root of the unit provokes swelling and pulsating pain in neighboring organs, on half of the face.
Of course, the inflammatory process can be localized in the middle ear. With otitis media, discomfort can be traced in the jaw.
Traditional methods of treatment
If you have pain in the ear and tooth at the same time, you can additionally use folk methods and remedies for treatment. Most often, mouth rinses are used with water infusions and decoctions of chamomile, sage and calendula, and also a few drops of aloe juice and propolis are instilled into the ear canal. It is advisable to consult your doctor first.
What happens if pericoronitis is not treated?
It is important to understand that pericoronitis will not go away on its own. Even if after 4-5 days the symptoms subside, this does not mean that the inflammatory process is over. From time to time the disease will go into the acute stage and cause a lot of inconvenience. In addition, pericoronitis can cause serious complications.
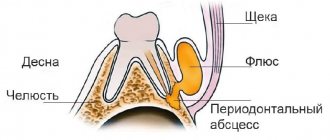
- Periostitis, or flux, as well as osteomyelitis. The spread of the inflammatory process to the periosteum and bone tissue can be explained by a decrease in local and general protective forces and other factors. Such complications will require serious medical intervention.
- Mobility of adjacent teeth.
- Cellulitis, abscess, lymphadenitis.
- Formation of fistula tract, cysts. The appearance of ulcerative stomatitis.
- Damage to nearby tissues, otitis, pharyngitis and other inflammatory complications in the area of ENT organs.
- Sepsis.
Therefore, treatment of pericoronitis is mandatory, regardless of the area in which the inflammation has spread. Lack of timely medical care can lead to inflammatory consequences and even loss of healthy adjacent teeth.
Characteristic features of inflammation of the trigeminal nerve
The trigeminal nerve has branches throughout the face, so even the slightest inflammation of its branches can provoke quite severe pain in the face. Unfortunately, painful attacks cannot always be distinguished from other diseases.
The first branch has a “process” in the form of the nasociliary nerve, which supplies nerve fibers to the frontal sinus, nasal dorsum and eyeball. Any injury to the face or disease of the paranasal sinuses can cause damage to this nerve, which will lead to severe pain in the nose and forehead. The attack of pain may last for several hours, and lacrimation may occur. In the intervals between painful attacks, aching and dull pain is observed.
The second branch has a “shoot” called the alveolar nerve, which supplies nerve fibers to the gums and upper teeth. This nerve is usually damaged during dental procedures or trauma to the jaw. The pain syndrome will be directed only to the upper teeth and gums, which is not associated with changes in the temperature of food or drinks. In the intervals between painful attacks, a dull ache is felt.
The origin of the third branch is called the mandibular nerve. It can be damaged due to trauma to the jaw, as well as during surgery or removal of lower teeth. The pain can be localized in the lower lip, teeth, chin and even ears. The pain is quite strong, so in the intervals between attacks the painful sensations are dull. Drinking hot or cold drinks or food does not cause pain.
Does your tooth or ear hurt? How to identify the source of discomfort and alleviate your condition
The roots of the chewing teeth of the upper jaw are located next to the ear canals, so discomfort caused by diseases of the hearing organs is often mistaken for pain in the molars. If you have tooth and ear pain at the same time, you need to undergo appropriate diagnostics from a specialist. Only with the help of a professional examination can one differentiate the pathology and choose the appropriate treatment vector. Read further in this article about how to understand whether your ear or tooth hurts, and what to do in such a situation.
Inflammation of the trigeminal nerve
Among the causes of the inflammatory process of the trigeminal nerve are the following:
- Compression of the nerve, as well as the ganglion. This usually occurs due to pathology of the artery itself. That is, due to the close proximity of the nerve passage next to the blood vessels, at the point where it exits the brain stem, it is compressed by the vessel wall. The reason for this may be an arterial aneurysm and high blood pressure. In rare cases, trigeminal neuralgia occurs in pregnant women, which usually goes away on its own after childbirth.
- There may also be a defect in the myelin sheath of the nerve. This happens if a person has any myelin diseases that cause inflammation of the trigeminal nerve.
- Another dangerous disease that can contribute to the development of neuralgia is the presence of tumor neoplasms, benign or malignant. It can originate from nerve tissue or the meninges.
- The most common cause of inflammation of the trigeminal nerve is post-traumatic neuralgia. It can develop after a severe concussion, brain contusion, or a sufficiently long period of unconsciousness. Such conditions can provoke the formation of cysts, which will compress the tissue, causing unbearable pain to the person.
- Postherpetic neuralgia is quite rare, which is the result of damage to the nervous tissue by the herpes simplex virus. The onset of the disease vaguely resembles infection with chickenpox, but the blisters are localized only on the face along the passage of the trigeminal nerve. After the virus infects the nerve tissues, a person begins to experience severe pain attacks, which are expressed in the form of an unbearable burning sensation.
Typically, pain during the inflammatory process in the trigeminal nerve is sudden, like a discharge of electric current, localized on one side and of a shooting nature. The pain syndrome is superficial, but quite strong. Surprisingly, a person suffering from trigeminal neuralgia thinks that they experience painful sensations all the time. They actually last about 2 minutes, but happen several times a day.
The provocative action is individual in nature for each person; it can be touching the face, brushing teeth, or even smiling. Pain due to the affected superior branch is localized in the orbits, temporal or frontal parts. Second branch neuralgia results in soreness of the upper jaw and teeth, as well as the area starting below the eyes and ending with the lower cheeks. Neuralgia of the third branch contributes to pain in the lower jaw and teeth, as well as the lower lip.
Preventive measures
We found out why an alarming symptom may appear and what to do about it. Now let's move on to the question of how to prevent an unpleasant situation.
The main preventive measure is regular visits to the dentist for prevention, as well as taking care of your health. It is advisable to undergo a comprehensive examination of the body every year and take all necessary tests. Such a responsible approach will allow timely recognition of the pathological process and initiation of treatment.
Preventative dental examinations will help avoid problems.
Neuralgic diseases usually develop against the background of serious injuries, viral infections, tumors and other systemic disorders. To reduce the risk of developing inflammation, you need to try to eliminate all traumatic factors and strengthen the immune system. Proper nutrition, physical activity and giving up bad habits are the basic rules of a healthy lifestyle.
If a symptom has already appeared, do not delay visiting a doctor. Painkillers only mask the discomfort, while the pathological process continues to progress. If the problem is an infection, it can easily spread through the bloodstream throughout the body, and then there is a serious risk of developing life-threatening conditions.
1Zhuravlev V.P. Etiology, pathogenesis, clinical picture, diagnosis and treatment of true trigeminal neuralgia, 2001.
Which specialist should I go to?
If you are completely sure of the cause of the ailment, you can consult a doctor of the appropriate profile. For example, if a wisdom tooth is erupting, you should go to the dentist; for chronic otitis media, you should go to an otolaryngologist; for arthrosis or displacement (trauma) of the jaw joint, you should go to an orthopedist or gnathologist; and a neurologist treats neuralgia.
If the true cause is unknown, and the pain continues to increase, you need to visit both a dentist and an ENT doctor. In any case, in the absence of pathology on the part of a particular organ, further consultations with other specialists will be required.
Types and forms of the disease
There are acute and chronic pericoronitis. Acute, in turn, is classified into the following types:
- Catarrhal. The disease begins with swelling and redness of the gums, pain, and itching. This is the simplest form of the disease.
- Ulcerative. It is characterized by the formation of ulcerations covered with a white coating on the mucous membrane of the gums, necrotization of tissue along the edges of the ulcer.
- Purulent. In the area of inflammation, serous and subsequently purulent contents are released. It is characterized by throbbing pain, general intoxication of the body, and bad breath.
Chronic pericoronitis is a consequence of an untreated acute period. With it, the symptoms become less pronounced, but serous or purulent contents continue to form. It can lead to the formation of a pathological passage through which the contents are discharged into the oral cavity. Chronic pericoronitis is characterized by periodic exacerbations; they can be provoked by tooth movement and other unfavorable factors, a general decrease in the body's defenses.
In the chronic form, lymphadenitis is often observed. The mucous membrane, even in the absence of unpleasant symptoms, is swollen and has a reddish tint. Despite the absence of serious difficulties when speaking, chewing, or opening the mouth, it is important to get help from a dentist, since the risk of complications is quite high, and the disease may not go away on its own.