In addition to pain, TMJ arthritis can manifest itself:
- swelling and redness of the skin over the joint;
- an increase in the patient's general body temperature;
- restriction of mouth opening and inability to completely close the teeth.
Diagnosis of inflammatory processes affecting the TMJ consists of analyzing the patient’s medical history, palpation examination of the area of the joint, as well as the results of radiography and CT scans of the affected joint. Therapeutic tactics aimed at eliminating this disease involve the use of jaw immobilization, complex antibacterial therapy, chondroprotectors, physiotherapeutic procedures, intra-articular injections of corticosteroids, as well as muscle exercises.
This disease is represented by acute and chronic forms, any of the forms is accompanied by dysfunctional disorders of the TMJ. Among all diseases of the temporomandibular joint, inflammatory lesions occupy about 18%. The category of the population most often suffering from this disease is young and middle-aged people. Based on the etiological factors contributing to the development of this disease, rheumatologists, dentists and traumatologists can treat it.
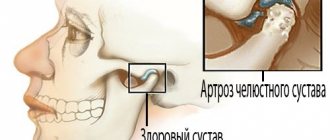
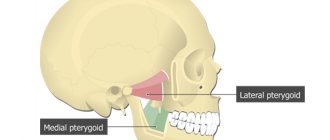
Anatomically, the TMJ is represented by a paired joint of the mandibular and temporal bones; its main function is to ensure mobility of the lower jaw. The joint itself consists of the head of the joint of the lower jaw, the articular tubercle, the mandibular fossa of the temporal bone, the articular disc, the ligamentous apparatus and the articular capsule. At the onset of the disease, periarticular tissues and the joint capsule are exposed to the pathological process. During the gradation of the disease, inflammation spreads to the surface of the joint, synovial membrane and areas of bone structures, accompanied by deformation of the cartilage and the appearance of connective tissue in the joint cavity. This disease can be complicated by deforming arthrosis, muscle contractures or bone ankylosis of the temporomandibular joint.
Characteristics of the disease
In medicine, the disease is called arthritis of the temporomandibular joint (TMJ). With the help of this joint all movements of the lower jaw occur.
The inflammatory process can occur in acute or chronic form. The main sign of the development of pathology is restriction in the movement of the lower jaw.
Such a pathology requires complex treatment and intervention by specialists of various profiles.
Depending on the area of localization, there are several forms of arthritis:
- disease of the lower or upper joint;
- arthrosis of the upper jaw joint.
Osteoarthritis occurs when a joint is severely deformed. The lesion affects both areas of the jaw node, the cartilage tissue is destroyed. In the first stages, the joint capsule becomes inflamed, then the cartilage tissue is affected.
Arthritis of the TMJ
Acute arthritis
The leading symptom in the clinic of acute TMJ arthritis is sharp pain in the joint area, which intensifies when trying to open the mouth or move the jaw.
As a rule, the pain is local, pulsating, but can often radiate to the tongue, ear, back of the head, and temple. With TMJ arthritis, the patient can open his mouth no more than 5-10 mm; when trying to open the mouth, the lower jaw shifts to the painful side. In the projection of the affected temporomandibular joint, hyperemia of the skin, swelling of soft tissues, and pain on palpation are determined. When serous exudate accumulates in the joint cavity, patients complain of a feeling of fullness in the jaw and the inability to close the teeth tightly.
Suppurative arthritis
Purulent arthritis of the TMJ occurs with symptoms of fever, the formation of a dense infiltrate in the joint area, hyperesthesia and hyperemia of the skin. Patients complain of acute local pain, hearing loss, and attacks of dizziness. Upon examination, a narrowing of the external auditory canal is revealed. It is possible to form abscesses that rupture into the parotid region or the external auditory canal.
Chronic arthritis
With chronic arthritis of the TMJ, pain occurs to a lesser extent; The leading complaints are joint stiffness of varying severity, a feeling of stiffness in the joint, glossalgia, and tinnitus. The amplitude of mouth opening is 2-2.5 cm; When the jaw moves, there is a crunching and clicking sound in the joint. Deformation of the articular head and cortical plate of the cavity during chronic inflammation can lead to subluxation and dislocation of the lower jaw.
Rheumatoid arthritis
Rheumatoid arthritis of the TMJ occurs with multiple arthralgias, symptoms of polyarthritis, and fever; At the same time, acquired heart defects may be detected in patients. Laboratory examination reveals positive rheumatic tests (CRP, sialic, diphenylamine, etc.).
Traumatic arthritis
With traumatic arthritis of the TMJ, the moment of injury is accompanied by sharp pain in the joint, followed by trismus and limitation of passive and active movements of the lower jaw. Often, traumatic injuries cause rupture of the ligamentous apparatus and hemorrhage into the joint, which subsequently leads to ankylosis of the temporomandibular joint.
Tuberculous arthritis
Arthritis of the TMJ of a specific etiology has a chronic course. Thus, with tuberculous arthritis of the TMJ, fistulous tracts often develop, and a secondary bacterial infection occurs. Diagnosis is facilitated by a history of contact with a tuberculosis patient, positive tuberculin tests, and characteristic changes in the lungs.
Gonorrheal arthritis
The course of gonorrheal arthritis of the TMJ is acute, with pain and infiltration in the joint area, low-grade fever, and intoxication. Syphilitic arthritis of the TMJ is characterized by the formation of gumma in the periarticular tissues and the formation of contracture of the lower jaw. With actinomycotic arthritis of the TMJ, periodic exacerbations of the chronic process also lead to the development of pronounced contractures of the masticatory muscles.
Diagnosis of TMJ arthritis
Risk factors
Main reasons:
- Injury. The cause in this case may be a bruise, a blow, or a sudden opening of the mouth.
- Infection of ENT organs. Arthritis of the maxillary joint can be caused by streptococci, chlamydia or tuberculosis.
- Osteomyelitis.
- Untreated caries.
- Periodontal diseases.
- Otitis.
In addition, the following conditions may also affect the development of jaw arthritis:
- Gout.
- Systemic lupus erythematosus.
- Diabetes.
- Thyroid diseases.
- Rheumatoid and reactive arthritis.
Sometimes inflammation can be caused by general hypothermia of the body.
Development factors
In infectious arthritis, pathogens affect the joint in several ways:
- contact (for otitis, osteomyelitis, furunculosis of the external organs of hearing, etc.);
- direct (infection enters the joint due to puncture of the TMJ, fracture of the movable jaw, injury, etc.);
- hematogenous (for sore throat, tuberculosis, measles, diphtheria and other infectious diseases).
The reactive form of arthritis is observed with chlamydia, rubella, viral hepatitis and other infections. Rheumatoid arthritis can spread to other joints. An acute traumatic form of pathology can develop due to mechanical damage to the joints.
How does the disease manifest itself?
- pain in the jaw area, radiating to other parts of the face and intensifying when opening the mouth;
- restrictions in joint movement;
- dizziness, chills;
- general weakness;
- increased body temperature (may be over 38 degrees);
- sleep problems;
- jaw clicks;
- joint pain on palpation;
- deformation of the oval of the face due to the fact that the chin begins to move to the side;
- hearing problems.
The important thing is that with arthritis of the jaw joint, purulent inflammation can begin! In such a situation, the joint turns red, swells and becomes very sensitive. A compaction is felt in the area of the mandibular joint. The skin changes its color, speech is impaired, and the process of chewing food becomes difficult.
Diagnosis and treatment methods
Modern methods used to identify the primary source that caused the development of pathology involve a set of procedures, which include radiography, CT and CBCT, PCR and DFA diagnostics. The key feature that distinguishes arthritis from other diseases is changes in the structure of the joint space (widening in the acute form and narrowing in the chronic form), as well as the formation of marginal lesions.
The treatment cycle involves immobilization of the joint for several days - a state of rest, combined with the use of compresses and painkillers, allows to reduce the load and relieve pain. Further recovery includes physical therapy using myogymnastics and electrophoresis, sanitation and local prosthetics. For the purulent form, a prerequisite is opening and cleaning the joint cavity.
Type of pathology
The clinical picture of arthritis depends on the form in which the disease occurs:
Acute form.
It is expressed by swelling of the soft tissues and severe pain in the affected area. As a rule, the acute form is the result of some kind of injury.
Chronic form.
This form is manifested by aching pain and difficulty opening the jaw, especially in the morning.
Infectious form.
Most often it is a consequence of a previous illness (flu, ARVI). Infectious arthritis is characterized by severe pain that makes it difficult to open the mouth. The pain radiates to the ears, temples and back of the head.
Traumatic appearance.
The most common form of the disease that occurs against the background of trauma.
Specific arthritis.
Rare disease. As a rule, it occurs as a consequence of syphilis, tuberculosis or gonorrhea.
Purulent form.
It is a consequence of acute arthritis in an advanced form. A compaction forms in the area of the mandibular joint, and body temperature may increase.
Rheumatoid form.
Constant pain in the maxillary joint area. With this form, the clinical picture may be supplemented by pain in the knee, hip or elbow joint.
Depending on what caused the inflammation, the following routes of infection are distinguished:
- Hematogenous. Bacteria enter the joint along with the blood (syphilis, tuberculosis, measles, etc.).
- Contact path. The disease develops due to damage to areas located near the maxillary joint (otitis, phlegmon, abscess).
- Straight way. Develops due to direct penetration (wound, jaw fracture).
The form of pathology can be identified only after examination and diagnostic testing.
Diagnosis and treatment methods
Inflammatory processes of the TMJ can be diagnosed in the early stages, but this requires timely treatment. Initially, the lesion is localized in the capsule, but as the problem progresses, it spreads to the surrounding tissues. If left untreated, joint mobility may be completely lost.
Diagnosis is made during the initial visit to the dentist. Additionally, consultations with a traumatologist, otolaryngologist, infectious disease specialist and other specialists may be required. The basic methods are CT, radiography, CBCT. Using an x-ray, the dentist is able to determine the presence of arthritis, widening or narrowing of the joint gap. The following types of examinations are also carried out:
- Schüller and Bordes techniques for lateral examination of the affected area;
- plain radiographs;
- layered tomography;
- zonography;
- contrast arthrography;
- magnetic resonance imaging;
- diagnostics ELISA (enzyme-linked immunosorbent assay);
- PCR study.
Treatment begins with analyzing the data obtained and drawing up a treatment regimen. The jaw is immobilized and the affected organ is kept at rest for 2-3 days. If necessary, a sling bandage, splint or interdental plate is applied. The patient should follow a semi-liquid diet, relieving tension on the joint. The treatment regimen depends on the form and degree of the lesion; physiotherapy and myogymnastics are usually prescribed.
In the acute form, injections of antibiotics, corticosteroids, and chondroprotectors are prescribed. In case of purulent form, surgical intervention, opening of the cavity, and drainage through an external incision are indicated. Chronic arthritis requires the use of physiotherapy methods, sanitation of the oral cavity and nasopharynx. In some cases, dental prosthetics are indicated.
Manifestation of jaw arthritis
In this case, the disease causes a feeling of pressure on the jaw joint or both joints. Later it becomes impossible to fully open the mouth. As the disease further develops, the patient's body temperature can rise to 39 degrees. Often at this stage even intoxication occurs.
The affected joint or both joints become very painful and swollen. The mucous membrane around the joints becomes inflamed. Then the pain intensifies and begins to radiate to the ears and temples. Bursts of pain are felt even when walking or tilting the head.
Causes of the disease
The causes and factors contributing to the occurrence of arthritis of the maxillofacial joint are very diverse and consist of both causes common to any joint and those that determine the specificity of jaw arthritis. We can highlight:
- infections;
- chronic and endocrine diseases;
- genetic predisposition;
- violation of metabolic processes;
- lack of nutrients;
- congenital dental defects;
- maxillofacial injuries.
What are the causes of arthritis of the jaw?
Nowadays, this disease rarely occurs due to bacterial or viral exposure. However, in not so distant times, when oral hygiene products were not as high quality as they are now, this happened often. Nowadays, arthritis of the jaw more often occurs as a result of injury to the jaw joint. This also often happens due to inflammation of the organs adjacent to the jaw joints. In particular, diseases such as osteitis, otitis and phlegmon can cause jaw arthritis. It is extremely rare that it occurs due to blood diseases.
Classification
TMJ arthritis can be:
- Spicy;
- Chronic;
- Bilateral;
- Unilateral;
- Infectious;
- Rheumatoid;
- Purulent;
- Deforming osteoarthritis;
Infection may result from direct spread or hematogenous spread. The area becomes inflamed, movement is limited, and pain appears. Bone destruction may be diagnosed. Acute traumatic arthritis can sometimes be associated with severe removal of the masticatory organ. Creaking and stiffness can occur in old age when bones rub against each other. Common manifestations of rheumatism are pain, swelling, and limited movement. Secondary degenerative pathology most often develops after injury. The patient has difficulty opening his mouth, and the pain is usually one-sided. The disease code according to ICD-10 (International Classification of Diseases) is K07.6.
Prevention
To prevent arthritis of the jaw, it is necessary to carry out timely sanitation of purulent chronic foci, as well as proper treatment of acute diseases of an infectious nature. Injury to the nodes must not be allowed. Specific infections in the body should be quickly eliminated. Muscle pain will decrease if the action of central and peripheral pathological factors is prevented, namely: occlusion disorders, strong impacts, prolonged depression. You cannot self-medicate so as not to provoke the development of the disease. Only an experienced doctor will be able to conduct a professional consultation and give practical advice to the patient.
So, due to education, they distinguish:
- infectious arthritis of the TMJ - is caused by infections and bacteria entering the bloodstream, which stimulate the inflammatory process of the joint. In turn, an infectious disease may be of a rheumatological nature or be a consequence of the presence or transmission of diseases such as tuberculosis, syphilis, gonorrhea, etc.;
- dystrophic arthritis of the TMJ - develops as a result of constant heavy physical labor;
- traumatic arthritis of the TMJ - is a consequence of a severe bruise or injury.
Treatment of temporomandibular joint arthritis with traditional medicine
If it is impossible to get an appointment with a doctor or the initial stage of the disease, traditional medicine recommends applying compresses and rubbing externally.
- Mix the beaten egg yolk with a teaspoon of turpentine and a tablespoon of apple cider vinegar. Rub the mixture into the sore joint.
- Squeeze the juice of grated black radish through cheesecloth, mix it with ¾ tbsp. honey, 1 tbsp. l. salt and 100 g of vodka. Rub the resulting mixture into the sore joint, then wrap it in something warm.
Traditional healers also have remedies for internal use in the treatment of TMJ arthritis.
- Displace 2 tbsp. buckthorn bark with 2 tsp. fennel fruits, 2 tsp. dandelion roots and 2 tsp. mint leaves. Pour the resulting mixture into 0.5 liters of water and simmer over low heat for 15 minutes. Take 2 tbsp before meals once a day.
- Pour 1 cup of boiling water over lingonberry leaves (20 g) and place in a water bath for 20 minutes. Drink 1 tbsp decoction. l. 4 times a day.
Before using folk remedies in the treatment of TMJ arthritis, you should definitely consult with your doctor.
Prognosis and prevention
Due to the seriousness of the pathology, it is recommended to immediately visit the clinic at the first problems and symptoms indicating the presence of negative changes in the structure of the jaw. Proper treatment can prevent the development of bone ankylosis, which can only be eliminated through surgery. Preventive measures recommended by experts include compliance with standard hygiene procedures, periodic sanitation of the oral cavity and timely treatment of infectious diseases.