Temporomandibular joint dysfunction is a pathological process that is caused by changes in the jaws, articular surfaces and muscle tissue. In this case, uncoordinated movement of both jaws in relation to each other is diagnosed with clear signs of a violation of static and dynamic occlusion. The pathology occurs quite often, accounting for about 75% of all patients in dental offices. Many oral diseases are a consequence of TMJ dysfunction. Also, nearby organs and tissues are involved in the destructive process, which complicates its clinical signs with additional symptoms.
Specialists usually diagnose a chronic form of pathology in the temporomandibular joint, which in some cases accompanies a person for many years and is compensated by other components of the maxillofacial apparatus. Without therapeutic measures, complete or partial ankylosis may occur; therefore, a timely visit to the dentist will prevent impaired chewing function, visual unattractiveness and many other problems, the development of which can be caused by TMJ dysfunction.
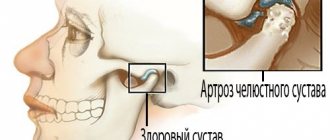
Definition of temporomandibular joint
The temporomandibular joint is a fairly mobile joint that connects the lower jaw and the temporal bone, located on either side of the skull, in front of the ears.
This hinge joint provides the following functions:
- sedate jaw movements characteristic of conversation;
- maximum opening of the mouth, for example, when yawning;
- movement of the jaw during chewing.
The main assistants to the joints of the maxillofacial apparatus are the masticatory muscles, which help keep the lower jaw in the correct anatomical position, while easing the load on it.
Prevention
Preventive measures require the fulfillment of such conditions as:
- maintaining proper and at the same time maximally balanced nutrition;
- optimization of the patient’s motor activity;
- rejection of bad habits;
- ensuring the proper level of oral hygiene;
- systematic attendance at preventive medical examinations.
Do not delay the treatment of arthrosis of the jaw joint, because in the first stages the disease is treatable, which allows us to talk about the complete restoration of jaw functionality.
Causes of dysfunction of the temporomandibular joint
Modern dentistry has facts that have not been fully studied about the causes of pathologies of the temporomandibular joint. However, based on the available data, experts suggest that the main problem lies in the destructive processes of the muscles and altered components of the joint itself.
Orthodontists identify the following pathologies and situations as the main causes and provoking factors for impaired mobility of the joint connecting the lower jaw (mandible) and the temporal bone:
- trauma to the lower jaw, which can provoke a violation of static and dynamic occlusion;
- damage to the facial muscles, which is accompanied by an increase in the load on the joint;
- pinching of the facial nerve causes excessive muscle tension, which, in turn, disrupts the functioning of the joint and mandible as a whole;
- involuntary contraction of the chewing muscles, which is usually accompanied by damage to the dentition, periodontal disease and inflammation of the TMJ;
- damage to the temporomandibular joint due to the progression of osteoarthritis or rheumatoid arthritis;
- inadequate prosthetics;
- congenital anomalies of the structure of the lower jaw;
- malocclusion, which in 95% is caused by destructive manifestations;
- pathologically low alveolar processes;
- inflammatory processes of the articular surface of infectious etiology;
- incorrect position of the disc at the junction of the head of the joint and the corresponding notch;
- prolonged tension of the facial muscles, clenching of teeth due to strong emotional stress.
The information provided about the probable causes of TMJ dysfunction is confirmed by clinical studies and the results of collected anamnesis about the disease.
Risk factors
Main reasons:
- Injury. The cause in this case may be a bruise, a blow, or a sudden opening of the mouth.
- Infection of ENT organs. Arthritis of the maxillary joint can be caused by streptococci, chlamydia or tuberculosis.
- Osteomyelitis.
- Untreated caries.
- Periodontal diseases.
- Otitis.
In addition, the following conditions may also affect the development of jaw arthritis:
- Gout.
- Systemic lupus erythematosus.
- Diabetes.
- Thyroid diseases.
- Rheumatoid and reactive arthritis.
Sometimes inflammation can be caused by general hypothermia of the body.
Characteristic symptoms
Symptoms characteristic of the manifestation of a destructive process in the joint, which ensures the mobility of the lower jaw, can be pronounced or blurred, which is typical for a protracted chronic process. Periods of remission followed by exacerbations are also likely, that is, symptoms can suddenly appear against the background of imaginary well-being.
Specialists in the treatment of TMJ destruction identify the following characteristic symptoms of this pathology:
- severe soreness of the muscles of the face, neck, shoulder girdle and parotid region with irradiation into the ear cavity;
- toothache;
- pain tends to intensify during speech, eating or yawning, that is, when the amplitude of movement of the lower jaw increases;
- there is pronounced stiffness and limitation in the movement of the jaws;
- partial ankylosis (immobility) may occur as a result of jamming or blocking of the joint;
- there is a pronounced sound when opening the mouth, for example, clattering, clicking or creaking, which, in most cases, is accompanied by sharp pain;
- tension and fatigue of the facial muscles;
- sometimes swelling of the affected joint increases;
- difficulty chewing, accompanied by a feeling that the jaws are not touching each other.
The patient's general condition also shows deterioration, characterized by headache, dizziness, noise and aching pain in the ears, and decreased performance. Acute pathological processes in the temporomandibular joint sharply reduce a person’s quality of life with debilitating manifestations, disrupting many vital functions.
Diagnostic methods
Medical diagnosis is carried out using x-ray examination, the results of which make it possible to determine the type and stage of changes occurring.
In addition to radiographic diagnostics, in order to make the most accurate diagnosis, laboratory tests of urine and blood, as well as additional instrumental research methods, can be used.
Self-diagnosis reminder
Changes such as:
- the appearance of crunching/clicking sounds when performing various types of movements;
- decreased jaw mobility, manifested when eating, yawning, etc.;
- hearing impairment;
- decreased visual ability;
- pain of a pressing or bursting type, localized mainly in the temporal or parotid-masticatory region of the head;
- periodic convulsions accompanied by painful sensations;
- dysfunction of the vestibular apparatus;
- increased fatigue when chewing food, difficulty eating solid foods;
- partial loss of facial expression;
- numbness of the skin and mucous membranes in the area of the affected joint.
Who treats TMJ dysfunction?
Degenerative processes in the lower jaw joint are a disease that is treated by dentists and specialists in treating problems of the maxillofacial apparatus, for example, orthodontists and orthopedists. However, the etiological factor may necessitate intervention in the treatment process by specialists from other areas of clinical medicine. Thus, to ensure maximum effectiveness of therapeutic measures, the direct participation of such doctors may be necessary:
- a traumatologist is needed when the temporomandibular joint is displaced due to injury;
- consultations with a neurologist will be needed, first of all, if the facial nerve is pinched, as well as when exposed to many other factors, since the disease often involves nerve endings in nearby tissues and organs;
- a psychologist will be needed to stabilize the patient’s psycho-emotional state if destruction in the lower jaw joint has occurred due to prolonged tension in the facial muscles caused by psychological trauma or stress.
Of course, dental specialists play a leading role in the treatment of temporomandibular joint dysfunction, and representatives of related areas act as consultants.
If you have pathological symptoms, you should immediately contact any specialist, for example, even a therapist. The doctor will definitely conduct an examination and coordinate the patient’s further actions if he detects signs of dental pathology. The variety of manifestations of the disease of the maxillofacial apparatus, in most cases, causes difficulties in diagnosis even for an experienced specialist. An accurate diagnosis is established after additional examinations.
Differentiation of diagnosis
The symptoms of pathological processes in the joint, which provides movement of the lower jaw, are similar to the manifestations of other diseases. Doctors, using special examinations, must accurately differentiate the diagnosis so as not to miss the development of the following serious pathologies:
- myocardial infarction, which is also characterized by pain radiating to the neck, lower jaw and shoulders;
- otitis media of unknown etiology can be suspected when there is severe pain and hearing loss;
- cerebrovascular accident may occur with dizziness, flashing of flies and nausea;
- cervical and thoracic osteochondrosis are similar in localization of pain;
- pinching of the facial nerve is also caused by unilateral tension of the facial muscles and swelling;
- complicated diseases of the gums and teeth, which are accompanied by inflammation and immobility of the lower jaw.
To avoid making an incorrect diagnosis, the doctor carefully studies the patient’s life history and illness, conducts a visual and palpation examination, and also prescribes the necessary tests.
[slide-anything id=”3470"]
Features of diagnostic measures for TMJ dysfunction
For the most accurate diagnosis of damage to the articular surface of the lower jaw at the junction with the temporal bone of the skull, specialists use the following methods and the following examination plan:
- clarification of the patient’s vital functions (work specifics, presence of chronic diseases, psycho-emotional background);
- questioning the patient about the probable cause of pathological changes in the jaw (trauma, inflammatory processes in the oral cavity, past dental history, the presence of neurological pathologies);
- visual inspection of the outer surface of the projection of the joint and the oral cavity, if possible;
- palpation examination of the joints of the mandible, which helps to identify muscle tension, swelling and displacement;
- listening to sounds when opening the mouth, which can be in the form of clicks or crackling sounds;
- determination of the amplitude of jaw mobility;
- identifying the scope of possible movements;
- assessment of the functionality of the masticatory muscles;
- determining the correct bite;
- X-ray examination of the dentofacial apparatus, which will be the most informative for excluding other pathologies of teeth and gums;
- the magnetic resonance imaging method allows you to examine the soft structures of the jaw, for example, intra-articular cartilage and its physiological position, the correctness of which determines the condition of the TMJ;
- CT scan results will provide a layer-by-layer image of the bone structure of the jaws.
The results of these examinations may require consultation and treatment with a dental surgeon, traumatologist or orthodontist.
Classification
Based on the results of an X-ray examination, in accordance with the diagnosed changes, it is customary to distinguish between two types of arthrosis:
- sclerosing - changes suggest sclerotic changes in bone surfaces, accompanied by a significant narrowing of the gap between the heads of the bones;
- deforming – there is a significant loss of texture and inherent forms of bone tissue, as well as a significant proliferation of osteophytes.
According to their origin, there are two types of pathology:
- primary – forms independently, without previous diseases/damages, mainly in old age;
- secondary - has a close connection with previous trauma, inflammation or metabolic disorders.
Therapeutic measures for diseases of the temporomandibular joint
When an accurate diagnosis of TMJ dysfunction is established, the doctor prescribes a course of therapeutic measures, the features of which are determined by the degree of the pathological process and the etiological factor. The disease requires complex treatment. The most lasting effect in restoring the functions of the maxillofacial apparatus is provided by the following recommendations, methods and means:
- complete exclusion of solid food, which will make it possible to maintain conditional rest for the mandible joint;
- maximum restriction of mobility (no yawning, no talking);
- alternating warm and cold compresses in combination with certain exercises to warm up the joints, which is performed under the supervision of a physiotherapist;
- for pain relief, the doctor prescribes non-steroidal anti-inflammatory drugs in a certain dose and at the recommended dosage interval;
- in case of extremely severe pain, it is possible to take narcotic analgesics;
- muscle relaxants are used to eliminate tension in the muscles of the face, neck and shoulder girdle, if any;
- to restore harmony in the patient’s psycho-emotional background, it is possible to take antidepressants in small dosages;
- physiotherapeutic procedures (laser, electrophoresis with novocaine, ultrasound, radio wave therapy, neurostimulation);
- installation of a special design on the teeth (mouthguard, orthopedic splint), which allows you to prevent the closure of the dentition as much as possible, correct the bite and restore the movement of the TMJ joint in the physiologically correct position;
- orthopedic treatment involves the installation of crowns and bridges to align the dentition and ensure comfortable static and dynamic occlusion;
- avoidance of foods that irritate tooth enamel to prevent relapse of exacerbation;
- a slightly open position of the mouth, which is carried out using the tongue located between the front teeth, will ensure relaxation of the masticatory muscles and jaws;
- in some cases, doctors use the injection of analgesic drugs into the muscle tissue of the projection of the pathological joint.
Complex treatment using the listed methods and means, in most cases, gives a positive effect and long-term remission.