Why was a sponge placed after tooth extraction?
To understand why the doctor put a sponge in an open wound on the gum after removing a tooth, it is worth understanding the processes that occur during and after the operation.
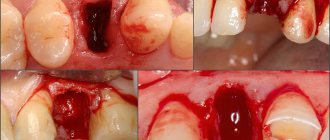
Tooth extraction is a traumatic surgical procedure. When roots are pulled out of a bone socket, numerous blood vessels and capillaries are torn. And the larger the tooth, the more serious the bleeding.
Normally, the blood stops on its own within 15-30 minutes. During this time, a blood clot forms in the hole - a natural thrombus to seal the wound.
But there are times when the bleeding does not stop, the blood clot does not form or falls out. The main reasons for this are the patient’s failure to comply with recommendations after tooth extraction. After deletion you cannot:
- rinse your mouth;
- drink drinks through a straw;
- eat in the first two hours after surgery;
- experience intense physical activity;
- heat the injured area.
The listed factors can easily provoke new bleeding or intensify existing bleeding.
Also at risk are patients who:
- blood diseases;
- high blood pressure;
- Prescribed medications that reduce blood clotting.
The situation with bleeding from the socket is also aggravated by difficult removal, when the dentist has to cut through soft tissues and drill into the jaw bone.
In all cases, the doctor will need a medicated sponge after the tooth extraction to solve the problem. A local hemostatic agent will completely replace the blood clot - block the wound and speed up healing.
Rules of application
GG is used topically for wound packing. So, first you need to cut off the required amount of the product and place it in an empty hole. Within 5–7 minutes, the sponge fills with blood, increases in size, and completely covers the wound. If one layer of GG was not enough to stop the bleeding, you can put another agent on top. The “lower” sponge remains in the hole until the end, but the upper ones can be changed until the bleeding from the wound is completely stopped.
When the blood has stopped, the GG is fixed with a suture and treated with thrombin solution to enhance the clinical effect. It is noteworthy that in addition to dentistry, hemostatic sponges are widely used in other medical fields to stop local bleeding. Self-resorbable GG with medication is also used for preventive purposes.
What kind of sponge is placed in the hole after tooth extraction?
Local hemostatic agents are quite simple in composition and structure. Outwardly they resemble a piece of foam rubber, a sponge. Shade - white or yellow. Dimensions - depend on the manufacturer, 50x50 mm and 100x100 mm. The sponges are easy to cut, so the doctor simply separates a piece according to the size of the hole and places it in the wound.
Hemostatic sponges are produced from donor blood and based on cattle bone tissue. On this basis, the drug is divided into three types:
- collagen sponges - based on cattle bones and tendons;
- gelatinous - only animal bone tissue;
- amben - from donor blood plasma.
To make the drugs more effective, manufacturers supplement the basic composition with various substances:
- antiseptic - a sponge with iodine after tooth extraction, with chlorhexidine, furatsilin, silver-based or boric acid;
- painkillers - the effect of the sponge is enhanced by lidocaine;
- to accelerate the regeneration of bone tissue - calcium phosphate is injected into the sponge to quickly heal the holes;
- antibacterial - the sponge layer is impregnated with antibiotics.
Natural substances such as propolis and eugenol can also be injected into the hemostatic collagen sponge.
Therapeutic components in the self-absorbing sponge:
- stop bleeding;
- accelerate healing;
- protect against bacterial infection;
- reduce swelling of soft tissues;
- prevent the development of inflammation;
- relieve pain.
Restoration of dental defects is inextricably linked with the use of dental implants. The basic principles of dental implantology that determine the future: achieving an optimal result with minimal trauma for the patient, reducing the duration of treatment, the number of stages, and the cost for the patient. Unfortunately, ideal conditions for installing a dental implant are quite rare. With the loss of chewing teeth of the upper jaw, there is an increase in pneumatization of the maxillary sinus, which leads to thinning of the bone tissue in this area [1, 2]. When the height of the alveolar process decreases in a number of clinical cases, a local increase in bone mass in the area of proposed implantation is necessary.
When analyzing defects in the dentition of the upper jaw, it was found that it is often impossible to do without a sinus lift. Sinus lifting is indicated in cases of insufficient bone tissue height when it is impossible to install a 10 mm dental implant. According to J. Rosenlight [3], generally accepted recommendations for the implementation of this technique are as follows: if there is 3 mm of bone tissue or less, an open sinus lift with implantation delayed for 6 months is indicated; if there is more than 3 mm of bone in height, an open sinus is indicated -lifting with immediate implantation, with a bone height of 5 mm or more - closed sinus lifting with immediate installation of dental implants. A separate group includes patients with teeth that need to be removed due to periodontal diseases, caries and its complications. In such cases, most clinicians take a wait-and-see approach after tooth extraction until the healing process of the sockets is completed. In our clinic, we have been studying the possibility of immediate implantation of extracted teeth into the sockets with a simultaneous sinus lift for many years. An analysis of the literature on the topic showed that in few cases the doctor decides to implant extracted teeth into the sockets in the presence of inflammatory processes in the tooth and to combine such an operation with an open sinus lift operation.
This study was made possible after a thorough analysis of the physiological processes occurring during blood clot reorganization and implant integration, as well as an analysis of the influence of the properties of the hemostatic sponge on the healing process.
It has already been proven that inflammation at the site of tissue damage triggers the mechanism of reparative regeneration and at the same time helps fight infection and eliminate dead tissue. Due to the increase in the permeability of the vascular wall in the area of inflammation, the migration of leukocytes, mainly neutrophils, begins. Studies have shown that the longer the neutrophilic stage of inflammation, the worse the regeneration process. When the macrophage stage prevails, normotypic regeneration occurs, ending with morphogenesis inherent in a particular tissue.
According to the latest data published in the Georgia Institute of Technology, Atlanta, the differentiation of mesenchymal cells into osteoblasts occurs on a microstructured titanium surface without the participation of exogenous factors and depends on the method of processing this surface, but this mechanism has not yet been studied well [7]. After implantation, the interaction of proteins, carbohydrates, fats, blood ions and serum with its surface occurs. Such interactions are determined by the chemical composition, surface energy and micro-nanotopography of the implant surface. Osteoblasts do not come into direct contact with the material, but interact with proteins absorbed by the surface through signaling proteins responsible for osteoblast differentiation. As a result of a series of parallel observations by R. Olivares-Navarrete, L. Postiglione [7, 8], it was established that the layer of absorbed proteins also affects the result of differentiation of progenitor cells. Differentiation into osteogenic cells directly depends on tissue oxygenation, i.e. on the degree of restoration of the microcirculatory network at the site of surgery. It should be noted that macrophages produce an angiogenic factor that stimulates vascular growth. The construction of new bone begins with the synthesis of collagen matrix by osteoblasts. Necessary organic and mineral substances enter the surgical area due to the rapid restoration of the microcirculatory network, the continuity of which is restored in the first 2 weeks. When creating an extracellular bone matrix, osteoblasts synthesize non-collagenous proteins, including bone growth factors - osteocalcin and osteonectin. The latter triggers the mineralization of the organic bone matrix, while osteocalcin stimulates the activation of osteoclasts at the final stage of reparative regeneration. As a result of the actions of osteoclasts, bone morphogenetic protein is released.
When analyzing recent publications on the topic of raising the floor of the maxillary sinus using osteoplastic materials, an increase in rehabilitation time after grafting of bone material was noted. In the bone plastic material there are no living cells - osteoblasts, there is no bone morphogenetic protein, which is why the material has neither osteogenic nor osteoinductive properties, but is precisely a frame, i.e. directly functions as an osteotransducer. The use of D. Sohn, J. Moon [5, 6] of a collagen hemostatic sponge during sinus lift in animal studies showed stable formation of bone tissue 5 months after surgery. The hemostatic collagen sponge, introduced into the cavity during sinus lift, performs several important functions. Firstly, it is a source of collagen, necessary for building bone tissue. Secondly, due to the porous structure of the sponge, its adhesion to the edges of the wound increases; The sponge stabilizes the blood clot in the cavity and induces the process of thrombus formation due to the calcium salts included in its composition, accelerating the processes of clot reorganization.
Material and methods
The study included 878 patients aged 18 to 72 years who were treated at the hospital of the Central Clinical Hospital named after. A.A. Vishnevsky in the period from 2004 to 2009. Patients with a complicated medical history were not excluded from the study. For the convenience of data analysis, patients were divided into 2 groups: group 1 included patients who underwent open sinus lift using a hemostatic sponge with simultaneous implantation, group 2 included patients who underwent open sinus lift using a hemostatic sponge with immediate implantation into the sockets of extracted teeth (see table).
Diagnostics.
The degree of atrophy of the alveolar process, the volume of the maxillary sinuses, and the degree of tooth destruction were determined clinically and radiologically, using orthopantomography data and targeted X-ray images. In cases of difficult diagnosis, computed tomography data was used.
Surgical technique.
Treatment was divided into 2 stages - surgical manipulations and orthopedic therapy.
The technique of surgical intervention can be considered in 2 clinical examples - open sinus lift using a hemostatic sponge and immediate implantation, and open sinus lift using a hemostatic sponge and immediate implantation into the sockets of extracted teeth.
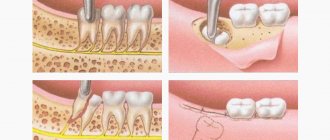
Open sinus lift using a hemostatic sponge and immediate implantation into the sockets of extracted teeth (Fig. 1-8, Fig. 4-6, see color plate).
Figure 1. Orthopantomogram (OPTG) before treatment.
Figure 2. Initial situation in the oral cavity.
Figure 3. Incisions are made, the mucoperiosteal flap is detached; after removing 2.4, 2.7, access to the maxillary sinus was achieved.
Figure 4. After lifting the Schneiderian membrane, dental implants, Xive system, are installed. The cavity is filled with a hemostatic sponge and several granules of the Kollapan material are added.
Figure 5. Adapted PRP membrane.
Figure 6. Wound edges aligned. The wound is sutured with a continuous suture.
Figure 7. OPTG after surgery.
Figure 8. OPTG 5 months after surgery; formation of bone tissue in the area of surgical intervention is observed; during this time, dental implants were installed in the area of missing teeth in the lower jaw, and orthopedic structures were made.
Results and discussion
The study group consisted of 878 patients: 465 (53%) women and 413 (47%) men aged 18 to 72 years (average 44.3±2.1). Of these, 527 (group 1) underwent sinus lift operations using a hemostatic sponge with simultaneous implantation, and 2,371 dental implants were installed. 325 patients (2nd group) underwent sinus lift operations using a hemostatic sponge with simultaneous implantation into the sockets of extracted teeth, 1581 dental implants were installed (see table)
. The implant failure rate in both groups was 2%; it was observed in 17 patients of group 1 (47 implants) and in 11 patients of group 2 (32 implants). Both groups included patients of the older age category, people with a burdened medical history: diagnosed osteoporosis, diabetes mellitus types 1 and 2, chronic sinusitis. There was no statistically significant implant rejection in this group of patients. In the postoperative period, not a single patient complained of significant discomfort in the intervention area. Patients with a history of maxillary sinusitis complained of mild discomfort.
A combined technique was used to perform open sinus lifting operations using a hemostatic sponge with one-step installation of dental implants and open sinus lifting using a hemostatic sponge with one-step installation of dental implants in the sockets of extracted teeth. The goals of using this technique are to show the effectiveness of using a hemostatic sponge as a material that can replace osteoplastic allogeneic and xenogeneic materials, which are traditionally used during open sinus lift surgery, to reduce treatment time, and reduce its cost for the patient.
Based on the results of the study, it can be concluded that the hemostatic sponge used to raise the floor of the maxillary sinus can be recommended as a material replacing allogeneic and xenogeneic osteoplastic materials. Open sinus lift operations using a hemostatic sponge to lift the floor of the maxillary sinus with the simultaneous installation of dental implants both in the edentulous areas of the upper jaw and in the sockets of extracted teeth, followed by prosthetics, can be recommended as a safe and effective method for restoring dentition defects.
Sponge in the hole after tooth extraction: when will it resolve?
A hemostatic agent placed in the socket of an extracted tooth dissolves on its own. There is no need to remove it. Moreover, if for some reason the wound is exposed ahead of time, it is necessary to urgently visit a doctor for antiseptic treatment and re-placement of the sponge in the hole.
The rate of absorption of the drug depends on its composition. The average is 2-3 weeks. The longest period is 1.5 months. If the sponge has not resolved within 6 weeks, you should consult your doctor for advice.
Release form
GG is a soft elastic porous plate with a faint odor of acetic acid. After the hemostatic sponge is inserted into the hole, it absorbs liquid, swells, and increases in size. As a rule, GGs are produced in 2 standard sizes - 50 X 50 mm, 100 X 100 mm.
Since this product has a characteristic porous structure, it can absorb a volume of liquid 30-40 times larger than its own. At the same time, the collagen sponge does not allow the formed protective blood clot to dissolve (thanks to the Ambien present in its composition).
Treatment after tooth extraction: application of a hemostatic agent
After wisdom tooth removal, a self-absorbing sponge in the socket is almost always necessary. The sequence of drug administration takes place in several stages immediately after tooth extraction:
- separating a cube or plate of hemostatic sponge with sterile scissors and fixing the drug with tweezers;
- placement of the substance in the hole - for stability and tightness of fit, the sponge is pressed for a while with a flat tool;
- applying a second layer of the drug - in case of severe bleeding.
If necessary, the hemostatic agent is additionally fixed:
- with a tampon - applied for a day, then it is rejected on its own or removed by a doctor;
- U-shaped suture - with additional treatment of the wound with drugs to accelerate blood clotting.
If the blood clot falls out, or bleeding resumes after some time after removal, all manipulations will be preceded by cleaning the hole. An experienced surgeon will clean out dead tissue, remove pus, and treat the wound with antiseptics. After this, the hemostatic agent will be reapplied and secured.
Sponge in an extracted tooth: indications
The medicinal composition performs many tasks, which makes it especially in demand in surgical dentistry. The doctor uses the drug for:
- difficult removal;
- extraction of wisdom teeth, “eights”;
- the need for accelerated healing with simple tooth extraction;
- plastic surgery on gums;
- curettage of gum pockets;
- removal of dead tissue in osteomyelitis.
The use of a hemostatic agent in preparing the patient’s oral cavity for dental implantation is also indicated. The drug not only reduces the risk of complications during the extraction of mobile and destroyed units, but also accelerates the process of formation of new tissues. This allows you to significantly reduce the time between tooth extraction and installation of a dental implant.
Contraindications
Contraindications to the use of the drug are minimal. Usually these are allergic reactions to the substances used to impregnate the sponge composition. Before placing a sponge into the hole, the doctor will definitely check whether there is an allergy to medications and only after that will select the drug.
The sponge in the hole is completely inert. It does not cause side effects. If swelling, pain, itching is observed, then you should consult a doctor and check the quality of healing, to exclude the development of complications after removal.
A hemostatic sponge is an excellent tool for stopping primary and secondary bleeding after tooth extraction. This is a safe drug that replaces a blood clot, helps speed up healing, and protects the open wound from pathogenic microflora.
Precautionary measures
Absorbable GG is not used for heavy bleeding resulting from damage to large vessels. A contraindication to the use of a sponge is the patient’s individual intolerance to certain components of the product (for example, Furacilin). When used independently, it is not allowed to place (remove) GG into the inner layers of the socket; only surface application is permissible. When the hemostatic effect is achieved, the sponge is carefully removed from the postoperative wound.