From this article you will learn:
- what is dental pulp and its functions,
- structure and architectonics of pulp layers,
- histological preparations.
Dental pulp (pulpa dentis) is a specialized type of loose fibrous connective tissue rich in blood vessels and nerve fibers that fills the cavity of the tooth, i.e. pulp chamber and root canals. Due to the presence of a large number of receptor nerve endings in it, the pulp provides very high pain sensitivity of tooth tissue to the effects of mechanical, physical, and chemical stimuli.
Inflammation of the pulp (pulpitis) most often develops as a result of pathogenic bacteria entering it. This occurs when the carious process spreads to the deep layers of dentin surrounding the pulp chamber, but in some cases the cause of inflammation can be physical trauma to the tooth or a thermal burn (for example, due to errors when preparing a tooth for a crown). Most often, pulp inflammation occurs acutely, with severe pain, but in some cases the course can be asymptomatic - with a predominance of hyperplastic processes.
Structure of the dental pulp (diagram) –
Due to the abundance of blood vessels in the pulp, as well as due to the presence of narrow apical openings at the apexes of the roots, with the development of acute pulpitis, inflammatory edema always increases rapidly. Since the volume of the pulp is limited by the walls of the pulp chamber, inflammatory edema leads to compression of the veins and lymphatic vessels, thereby disrupting the outflow of fluid. This leads to the development of necrosis and death of the pulp. In addition, swelling also leads to compression of nerve endings, which actually causes the development of acute pain.
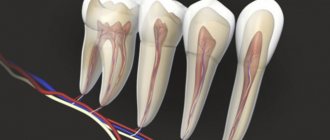
It should be noted that the dental pulp contains entire nerve plexuses, including a large number of receptors that are capable of perceiving stimuli of any kind - pressure, temperature, chemical and physical influences. But at the same time, effector nerve endings are also described in the pulp. Part of the nerve fibers of the pulp (together with the processes of odontoblasts) exits it into the predentin and the inner zone of the peripulpal dentin, located in the dentinal tubules.
The structure of the dental pulp –
Speaking about the structure of the dental pulp, we will first analyze its structural elements - after which we will move on to a description of its layers, which you could see in Fig. 2. You can see the appearance of the pulp removed from the tooth (wound on a pulp extractor) in the photo below.
1) Structural elements of pulp –
The pulp consists of loose fibrous connective tissue (with a large number of nerve endings, blood and lymphatic vessels). Accordingly, its structure will consist of collagen fibers, the main amorphous substance, as well as a large number of various cellular elements. The total collagen content is from 25 to 30% of the dry mass of the dental pulp, and it is mainly collagen types I and III. In the coronal part of the pulp, collagen fibers are located more loosely, but in its root part they form denser clusters.
As for the main amorphous substance located between the collagen fibers, it consists of water, glycosaminoglycans, as well as glycoproteins and proteoglycans. The intercellular substance has a high ability to diffusion, which allows nutrients from the blood to enter the cellular elements, and metabolic products to be excreted into the venous circulatory system. There is also a wide variety of cellular elements in the pulp - primarily odontoblasts and fibroblasts (fibroblasts are responsible for the formation of intercellular substance and the synthesis of collagen fibrils), as well as dendritic cells, macrophages, lymphocytes, mast cells, etc.
Cellular elements of the pulp -
| Cells | Odontoblasts – form dentin and provide its trophism. Neighboring odontoblasts are interconnected by intercellular connections, which allows the layer of odontoblasts to also perform a barrier function (regulating the movement of molecules and ions between the pulp and predentin). Some authors call these cells “dentinoblasts.” |
| Fibroblasts are the most numerous cells in the pulp (their number decreases with age). Their function is to produce and maintain the composition of the intercellular substance of the pulp, as well as to absorb and digest the components of the intercellular substance. | |
| Macrophages - participate in the renewal of the cellular composition of the pulp, capturing and digesting dead cells and components of the intercellular substance. They phagocytose microorganisms and participate in the development of immune reactions as antigen-presenting effector cells. | |
| Dendritic cells – they are antigen-presenting cells whose function is to absorb various antigens, process them and present them to lymphocytes. They also induce the proliferation of T lymphocytes. The content of dendritic cells increases as the pulp matures, as well as with antigenic stimulation. | |
| T-lymphocytes are contained in the pulp in small quantities, but during inflammation their number increases sharply (of all types of this population of lymphocytes, T-suppressors predominate in the pulp). B-lymphocytes are not normally found in the pulp, and appear only when it is inflamed (they synthesize IgG immunoglobulins and provide humoral immune responses). | |
| Mast cells – they are located around blood vessels; are characterized by the presence in the cytoplasm of a large number of granules with biologically active substances (histamine, heparin, eosinophilic chemotactic factor, etc.). The release of these components causes an increase in vascular permeability. | |
| Poorly differentiated cells - can give rise to odontoblasts and fibroblasts. The content of these cells decreases markedly with age. | |
| Fibers and glycoproteins | Type I and III collagen fibers, reticular fibers, fibronectin. |
| Basic intercellular substance | Glycosaminoglycans, chondroitin, proteoglycan. |
Architectonics of dental pulp layers –
In the coronal part of the pulp, there are several layers that differ in their structure and functions - 1) the outer layer, consisting of odontoblasts, 2) the subodontoblastic layer, which in turn consists of several zones, including the Weil and Rinaggio zones, as well as the Rashkov plexus, 3) central pulp zone. Below we will analyze in detail the structural components of each layer.
Architectonics of dental pulp layers (diagram) –
- The outer layer (peripheral) - consists of several layers of odontoblasts, which are elongated cells with basophilic cytoplasm (24stoma.ru). In “young teeth” the pulp may contain 6-8 layers of odontoblasts, but the older a person gets, the fewer the number of layers will be (at least one layer). Odontoblasts are highly differentiated cells that are specific to the dental pulp.
Long processes (the so-called “Toms fibers”) extend from the odontoblasts, which penetrate the dentinal tubules to the entire depth of the dentin. Odontoblasts and their processes play a very important role in the nutrition of the tooth and the delivery of mineral salts to the dentin and to the enamel-dentin border. In addition, they perform the function of dentin synthesis both during the period of tooth development and throughout a person’s life (we are talking about the synthesis of secondary and tertiary dentin). In the root part of the pulp, a layer of odontoblasts is also present, but it is thinner than in the coronal part of the pulp.Odontoblasts are closely connected to each other by strong intercellular connections, but capillary loops penetrate through their layer, as well as the finest nerve fibers (branches from the Rashkov plexus). These nerve fibers form tree-like branches around the odontoblasts - they are often called the “superodontoblastic nerve plexus”. It is interesting that part of the nerve fibers will end around the odontoblasts, but the other part will be directed along with the processes of the odontoblasts into the dentinal tubules.
- Subodontoblastic layer - morphologically it is usually divided into 2 zones.
The first zone is the more superficially located “light Weil zone” (a layer poor in cell nuclei). This zone mainly consists of collagen fibers, as well as cell processes penetrating from the inner zone of the subodontoblastic layer. This layer contains a large number of capillaries, which form an extensive capillary plexus that nourishes both odontoblasts and the pulp as a whole. Also in this layer there are many myelinated and unmyelinated nerve fibers, forming the so-called Rashkov nerve plexus. The deeper zone of the subodontoblastic layer is the Rinagio zone (a zone rich in cellular elements). This zone consists of a large number of diverse cellular elements, for example, poorly differentiated cells are located here, which can give rise to odontoblasts and fibroblasts. In addition, fibroblasts themselves, lymphocytes, as well as capillaries and nerve fibers are located in this layer.
- The central zone of the pulp is a loose fibrous connective tissue rich in cells (primarily fibroblasts and macrophages). Also contains larger blood and lymphatic vessels, and larger bundles of nerve fibers. In the central zone of the pulp, dendritic cells, lymphocytes, plasma cells, mast cells, and blood granulocytes are constantly present in small quantities.
Summary: below, for convenience, we have arranged the structural elements of the pulp layers - in the form of a single table. Once again, we draw your attention to the fact that the intermediate (subodontoblastic) layer is well developed only in the coronal part of the pulp.
| Peripheral layer | Intermediate layer | Central layer | |
| outer zone (Reil) | inner zone (Rinagio) | ||
| – odontoblasts, – Toms’ processes, – capillary loops, – nerve fibers. | – processes of cells of the inner zone of the intermediate layer, – collagen and reticular fibers, – Rashkov’s nerve plexus. | – fibroblasts, – lymphocytes, – preodontoblasts, – poorly differentiated cells, – capillaries, – myelinated and non-myelinated fibers. | – PBST *, – large blood and lymphatic vessels, – bundles of nerve fibers. |
* PBCT is loose fibrous connective tissue.
Histological specimen (dental pulp and peripulpal dentin) –
Where 1 is dentin (where 1a is calcospherites, 1b is predentin). Where 2 is the dental pulp (where 2a is the peripheral layer consisting of odontoblasts, 2b is a cell-poor zone in the intermediate pulp layer, 2c is a cell-rich zone in the intermediate pulp layer, 2d is the central pulp layer).
Ultramicroscopic structure of odontoblast –
Above you can see what an odontoblast looks like with a branched process, which will be located in dentin and predentin (where 1 is dentin, 2 is predentin, 3 is an odontoblast process located in the dentinal tubule, 4 is the Golgi complex, 5 is the nucleus, 6 is mitochondria, 7 – endoplasmic reticulum.).
Differences between the coronal and root parts of the pulp -
The root part of the pulp has significantly weaker vascularization and innervation compared to the coronal part of the pulp. In addition, the cellular composition of the root part of the pulp is much poorer, and the odontoblast layer, even in the “young pulp,” has only 1-2 rows of cells. Apparently, such differences in structure depend on the characteristics (differences) in the supply of nutrients and calcium salts - in the crown and root parts of the tooth.
In the coronal part, dentin and enamel receive nutrients and calcium salts - almost exclusively from the dental pulp. As for the nutrition of the hard tissues of the tooth root, it occurs not only through the pulp, but also due to the process of diffusion of nutrients from the pericement. Therefore, evolutionarily, a decrease in the importance of root pulp in the nutrition of hard tissues of the tooth root has been formed, and its structure has changed.
| Coronal pulp: | Root pulp: |
|
|
Pulp histology: video
Below in video 1 you can see the histology of tooth tissue in stunning resolution. Video 2 is the best lecture on pulp histology you will ever hear. The video is in English, but if you wish, you can turn on subtitles and select translation from English into Russian in the settings.
Features of the structure of the pulp of temporary teeth -
The structure of the pulp in baby teeth differs little from permanent ones. For example, in baby teeth there are fewer differences in the structure of the coronal and root parts of the pulp, and in addition, the pulp in baby teeth is more abundantly supplied with blood. There are also slight differences in the composition of cellular elements and the number of collagen fibers (Fig. 3).
Blood supply to the dental pulp -
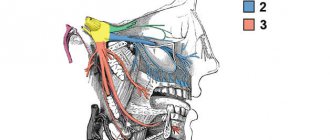
Blood circulation and innervation of the pulp are carried out thanks to dental arterioles, venules and nerve branches of the corresponding arteries and nerves of the jaws. For example, the pulp of the teeth of the upper jaw is supplied with blood from the superior alveolar artery, and the pulp of the teeth of the lower jaw - from the inferior alveolar artery. Branching off from the main vascular nerve trunk, the neurovascular bundles penetrate into the tooth cavity through the apical openings located at the apices of the roots and then break up into smaller branches.
However, vessels can enter not only through the apical openings at the root apices, but also through the openings of accessory canals on the lateral walls of the root. These holes may have clinical significance because... through them, infection can penetrate from the deep periodontal canals into the dental pulp (and vice versa). Thus, arterioles with a diameter of 50-150 microns penetrate through the openings of the tooth root and occupy the central part of the coronal and root pulp. In turn, smaller precapillary arterioles (10–12 µm in diameter) depart from the arterioles, which form an extensive capillary plexus in the Weil layer.
Pulp blood circulation diagram –
Capillaries with a diameter of 8-10 microns are usually divided into two groups. The first group is fenestrated capillaries (about 30%), which are located mainly near the odontoblast layer. Their presence facilitates the rapid transport of nutrients to odontoblasts, which is necessary especially during the period of active dentin formation (dentinogenesis). Upon completion of tooth eruption, the number of these capillaries decreases significantly.
The second group of capillaries are the so-called somatic capillaries (about 70% of them). Both types of capillaries provide nutrition to all structural components of the pulp. Moreover, the volume of the capillary bed can vary greatly, which is facilitated by the presence of a large number of collapsed capillaries (they begin to function only during inflammation), as well as arteriole-venular anastomoses. The latter provide the ability to discharge blood from the arterial into the venous (without the participation of capillaries).
From the capillary network in Weil's zone, blood flows into muscle-type venules (they contain smooth myocytes in the wall), which subsequently exit the pulp through the apical openings at the apexes of the roots. Moreover, venules are located more centrally in the pulp, while arterioles are located more peripherally. A unique feature of the blood circulation in the pulp is that the efferent venules have a smaller diameter than the arterioles entering the pulp. Therefore, even in the absence of inflammation in the pulp there are always phenomena of hyperemia and blood stasis.
Moreover, this same feature is very high intrapulpal pressure (about 20–30 mm Hg), which is much higher compared to interstitial pressure in other organs. All this ensures a fairly slow rate of blood flow through the pulp, and apparently is important for the nutrition of tooth tissue (trophic function of the pulp).
Lymphatic vessels of the dental pulp -
Lymphatic capillaries begin in the peripheral and middle layers of the pulp - in the form of sacs with a diameter of 15 to 50 microns.
They are distinguished by several features - first of all, a thin endothelial lining (with wide gaps between endothelial cells of more than 1 micron), as well as the absence of a basement membrane over a larger extent. Lymphatic capillaries are surrounded by a thin network of reticular fibers. With traumatic or inflammatory swelling of the pulp, lymphatic drainage increases. This is manifested by an increase in the diameter of the lymphatic capillaries, and a sharp widening of the gaps between endothelial cells also occurs (plus a sharp drop in the content of micropinocytotic vesicles in them). Further, through the lymphatic capillaries, the lymph flows into thin-walled collecting lymphatic vessels.
Innervation of the pulp -
The common sensory or afferent nerve for the maxillary and mandibular teeth are the II and III branches of the trigeminal nerve (i.e., the maxillary nerve and the mandibular nerve). In turn, nerves depart from them, which form plexuses - the superior dental plexus in the upper jaw and the inferior dental plexus in the lower jaw. In turn, bundles of myelinated nerve fibers branch off from these plexuses, which penetrate into the tooth cavity along with blood vessels - through the apical openings at the apexes of the roots. And, accordingly, forming a neurovascular bundle (tooth pulp) there.
The nerve fibers form a subodontoblastic nerve plexus, which is located under the layer of odontoblasts (also called Rashkov's plexus). Unmyelinated nerve fibers depart from this plexus, which are directed to the peripheral areas of the pulp, where they seem to entwine the odontoblasts, forming the so-called “nadodontoblastic plexus” between the odontoblasts and predentin. Some of the nerve fibers end in this plexus, but the rest of them penetrate into the dentinal tubules.
Removing the nerves of the front teeth: what to pay attention to
A beautiful snow-white smile always attracts attention and encourages communication. That is why during preventive examinations you should pay special attention to the health of the front teeth, which are located on the so-called. "smile lines"
Removing the nerves of the front teeth is not a technically difficult procedure; it is comparable in complexity to similar operations on other teeth. In this case, it should be taken into account that a pulpless tooth becomes a “dead” tooth - without receiving the necessary elements, it darkens and becomes fragile over time. Naturally, in this case it will be necessary to restore the beauty of the dentition over time.
Aesthetic dentistry at the Eurodent clinic offers several options for restoring the appearance of teeth:
- Teeth whitening (including pulpless teeth)
- Installation of veneers (lumineers, ultra-veneers);
- Artistic restoration of teeth;
- Installation of crowns (metal-ceramics, zirconium oxide).
In order to avoid the unpleasant consequences of removing the nerves of the front teeth, you should undergo regular preventive examinations by the dentist. The specialist will be able to notice “problems” before the appearance of alarming symptoms and eliminate them without any problems.
In order to find out how much it costs to remove a nerve in a tooth , you can come for a free consultation at the Eurodent clinic.
With us you can undergo high-quality diagnostics and receive qualified dental care. Based on: 19 votes
Functions of dental pulp –
The functions of the dental pulp stem from its morphology (structure). Below we list its main functions:
- Trophic function - we have already said that the pulp has a well-developed network of blood and lymphatic capillaries.
The main intercellular substance of the pulp serves as an intermediate medium through which metabolism occurs. Thus, oxygen and nutrients from the blood enter the cellular elements of the pulp precisely through the intercellular substance, and metabolic products are excreted through it into the venous or lymphatic systems. But the trophic function of the pulp is not only to nourish its own structures. The dentin and enamel of the crown part of the tooth receive nutrients and calcium salts - almost exclusively from the dental pulp (the processes of odontoblasts play a major role here). But as for the nutrition of the hard tissues of the tooth root, it occurs not only through the pulp, but also due to the process of diffusion of nutrients from the pericementum.
- Plastic function is realized thanks to odontoblasts, which throughout a person’s life participate in the formation of secondary and tertiary dentin. For example, in teeth there is a constant deposition of secondary dentin on the side of the pulp chamber, which leads to a gradual decrease in its volume. The deposition of denser tertiary dentin, as well as the obliteration of dentinal tubules, also occurs due to odontoblasts, and protects the pulp from external irritants and the penetration of bacteria into it.
- The protective function - the function of phagocytosis and disposal of dead cells is provided by neutrophil granulocytes and macrophages. Lymphocytes (plasma cells) - participate in the synthesis of antibodies. Fibroblasts participate in the formation of a fibrous capsule around the inflammatory focus. In addition, the pulp is also a biological barrier that prevents the penetration of pathogenic bacteria from the carious cavity into the periodontium. The protective function also includes the processes of formation of tertiary dentin and obliteration of dentinal tubules that we have voiced.
- Sensory function - carried out due to the presence of a large number of nerve endings.
Why does a dead tooth hurt?
It is logical that a dead tooth, that is, one from which the nerve has been removed, should not feel anything, much less hurt. However, patients often complain of toothache after tooth depulpation. With proper removal, a pulpless tooth cannot hurt; after removal of the nerve, pain can occur in the border structures: jaw bones, soft tissues, neighboring teeth, because the nerves remain there, and it is they that sometimes ache for several days, as they are “concerned” with the surgical intervention. However, if the pain does not stop, you need to consult a dentist; perhaps the nerve was not completely removed, or the pain is caused by some other reason - only a specialist can determine this.
A tooth is a very complex structure, and in this case the saying “Measure twice, cut once” fully reflects the essence of dental treatment!
Age-related changes in the pulp –
Even after the complete formation of a tooth, with age there is a gradual reduction in the size of the pulp chamber. This occurs as a result of continuous deposition of secondary dentin as well as intermittent deposition of tertiary dentin. Consequently, at a more mature age, the pulp will occupy a significantly smaller volume than at a young age. In addition, the shape of the pulp chamber itself changes (as a result, the pulp horns are smoothed out).
All this also has clinical significance, for example, deep preparation of dentin in the area of the pulp horns in old age will be less dangerous. In addition, with age there is a decrease in the number of cellular elements in all layers of the pulp (up to 50% of the initial level), but at the same time the content of collagen fibers increases 3 times. The blood supply to the pulp deteriorates due to the reduction of a large number of capillaries (especially those located in the capillary plexus in the Weil layer). Loss of nerve fibers also occurs, and in particular, this is associated with an age-related decrease in the sensitivity of the pulp to irritants.
With age, the frequency of formation of calcifications in the pulp also increases. Although, if calcification occurs not locally, but diffusely, then this process is called petrification. Petrifications most often form in the root part of the pulp (along the periphery of vessels, nerves, and also inside the vascular wall), sometimes causing disturbances in the blood supply to the pulp and pain. We hope that our article was useful to you!
Sources:
1. Higher professional education of the author in dentistry, 2. The European Academy of Paediatric Dentistry (EU), 3. “Anatomy of human teeth” (Gayvoronsky, Petrova). 4. “Periodontology” (Danilevsky N.F.), 5. “Pulpitis of temporary and permanent immature teeth” (Mamedova).
Pulpitis is enemy number 1!
Pulpitis is an inflammation of the dental nerve, which usually occurs as a result of advanced caries.
Pulpitis can be acute or chronic. The first is characterized by severe pain, especially at night. If you do not immediately go to the dentist, then after some time acute pulpitis will go into the chronic stage, the pain will dull somewhat, and the nerve will respond only to specific stimuli, especially changes in temperature. However, there is no need to calm down in this case, since if the patient does not go to the dentist at this stage, then complications may soon arise, and pulpitis will eventually develop into periodontitis, which can threaten tooth loss.