Necrosis is a serious pathology accompanied by the death of gum tissue. It is quite rare in dental practice. The danger of this process lies in its irreversibility, asymptomatic course in the early stages of development and serious complications that it can lead to if the necessary measures are not taken in time. Find out what can trigger necrosis of gingival tissue, what the dead areas look like, what symptoms should alert you and where to go if they are identified.
Necrosis of gum tissue: how dangerous it is, what causes it and how to treat the pathological process
Necrosis is the process of gradual death of cells and tissues, leading to the cessation of their functionality and cessation of vital activity. Such a pathological phenomenon can begin in almost any part of the human body. In dental practice, gum necrosis usually occurs when the mucosal tissue begins to die, which is due to the cessation of blood circulation in them. There are many potential causes for this pathological process. Today we’ll talk about what this phenomenon is, what its characteristic symptoms are and how to treat the problem.
Possible reasons
Gum necrosis can be associated with various negative factors. The process of cell death is triggered by:
- chemical burns - doctor’s mistakes when killing the dental nerve with arsenic, treating gum fibromatosis using liquid nitrogen;
- prolonged exposure to low temperatures - applying ice to the gum after implantation and other dental procedures;
- chronic periodontitis is an inflammatory disease that affects all periodontal structures; in severe cases, soft tissues die;
- mechanical injuries of the gums - rubbing of the mucous membrane with a prosthesis, cuts with subsequent infection, jaw fractures, serious bruises;
- hormonal imbalances - pregnancy, age-related changes in the body, taking certain groups of medications;
- bad habits - smoking, use of narcotic and psychotropic substances.
To establish the cause of gum necrosis, it is necessary to undergo a comprehensive diagnosis. If the pathological process is not stopped, dangerous complications can arise. The most common include osteomyelitis of the jaw, sepsis, and loss of chewing function.
What is gum necrosis?
Gum necrosis is a serious pathological process leading to irreversible death of mucosal cells and its destruction. Symptoms of the initial stage are usually poorly distinguishable and rather vague, which makes it very difficult to diagnose the problem in the early stages of its development. Experts in the field of periodontics distinguish two forms: wet and dry necrosis. The affected areas noticeably darken and lose sensitivity. At the same time, the treatment is quite complex and lengthy. If we are talking about the wet form, it is important to urgently transform it into a dry form, in which surgical intervention is possible to stop the further spread of the process. You can see what the affected gum looks like from the photo below.
At the initial stage of the pathology, the symptoms are quite difficult to distinguish
There are many factors that significantly increase the risk of developing pathology. This includes aggressive chemical exposure, sudden temperature changes, disturbances in blood composition, penetration of harmful microorganisms, and much more. Symptoms that may indicate a problem include bleeding, a putrid odor, loose teeth, ulcers, and pain. However, similar symptoms are typical for many other dental diseases, so it is important to see a doctor as soon as possible and undergo a thorough diagnosis. In addition, gum necrosis often develops against the background of advanced diseases, so this process can be considered as a complication of many pathological conditions.
Necrosis is not reversible, which means that dead cells are not regenerated. Timely seeking specialized help will help stop its further spread, but the resulting defects can only be filled with the help of gum grafting.
What is gum necrosis and should you be afraid of this phenomenon?
Necrosis is the cessation of vital activity, the death of certain tissues or organs in a living organism, caused by local cell death. For example, a heart attack is necrosis of the heart muscle. In dentistry, gingival necrosis is most often encountered - this is an irreversible process of death of gingival tissues caused by impaired blood circulation of their cells. Further in the article there is useful information about the causes of the disease, its symptoms, how gum necrosis is diagnosed and treated, what the prognosis is and how to protect yourself.
How can gum necrosis manifest itself?
For what reasons can the process of mucosal cell death begin?
There are quite a lot of potential prerequisites for the development of such a process. The most common causes of destruction of mucosal structures are the following phenomena and conditions:
- low level of hygiene and, as a consequence, the appearance of abundant dental plaque, the development of gingivitis, periodontitis, advanced stages of these diseases,
- constant injury to mucosal tissue due to malocclusion, poorly installed filling, crown or prosthesis - everything that disrupts local blood circulation and leads to its stop in certain segments of the gums,
- hormonal disruptions during adolescence, during pregnancy, and in diseases of the endocrine system and hematopoietic organs.
Untimely treatment of gingivitis can provoke necrosis.
Pathology can appear against the background of severe hypothermia or temperature changes, after using arsenic to kill the pulp. If a temporary filling with this substance is not sealed tightly enough, it can come into contact with the mucous membrane and provoke an irreversible process of its gradual death. Much less often, a similar problem occurs after tooth extraction due to severe tissue trauma, as well as after anesthesia. So, for example, if a powerful anesthetic is administered too quickly, a spasm of blood vessels and nerve endings may occur, which will lead to poor circulation. This situation is especially dangerous for patients with diabetes and infectious diseases.
How dangerous is this pathological phenomenon?
If you start the process, it will inevitably lead to irreversible consequences. The affected tissues do not have a chance to recover, and the further the necrosis goes, the higher the likelihood of losing teeth and losing chewing function. The addition of infections can provoke the development of osteomyelitis of the jaw - purulent-necrotic destruction of bone tissue structures. Less commonly, the pathological condition is complicated by general blood infection - sepsis.
You need to understand that necrotic areas in the oral cavity become a suitable environment for the proliferation of harmful microorganisms. The problem is that the initial stages of the pathology are quite difficult to diagnose. If the problem has already become pronounced, it will be much more difficult to treat.
Necrotic areas in the oral cavity become a suitable environment for the proliferation of harmful microorganisms
Causes of necrosis
- Radiological radiation (in cancer patients)
- Electromagnetic radiation (from computers and other gadgets)
- Disturbances in the functioning of the endocrine glands
- Malfunctions of the nervous system
- The patient has gastrointestinal diseases
- Hormonal imbalance
- Exposure to toxic substances
- Long-term use of medications that may contain substances harmful to teeth
- Radiation exposure
- Hereditary factor
- Abuse of products containing acids
The main symptoms of this disease are: chalky spots on the enamel in the neck of the tooth, increased sensitivity of the teeth and dilation of blood vessels, as well as changes in the color of the enamel. With necrosis, the tooth surface loses its shine and becomes dull. After exposure to toxic substances, a decrease in the acidity of saliva and a disruption of the microcirculation of the dental neurovascular bundle are also observed. Patients begin to complain of pain when brushing their teeth. If the problem is not treated in time, it can lead to a decrease in the efficiency of chewing function and impaired diction.
Types and symptoms of pathology
Necrosis develops gradually, moving from a mild stage to a more complex and advanced one. To choose the right treatment tactics, it is important to determine its form and degree of development:
- early stage – the symptoms are vague and weakly manifested. Dental tissues lose their shine, sensitivity to temperature changes in food occurs, and minor bleeding appears. The enamel becomes slightly rough, and the gums become pale, moving slightly away from the teeth,
- medium - the gingival papillae swell, destruction of their tips, bleeding, formation of a grayish coating, and pain when touched are observed. The affected area may become very pale or even darken, and an unpleasant odor may appear. Possible enlargement of the submandibular and other lymph nodes. At the same stage, ulcers may appear on the mucous membrane, the patient’s temperature rises to 38-39 ° C, headaches, appetite and sleep disturbances, nervous disorders occur,
- the latter – there is severe hyperemia, inflammation and swelling of the affected area. Tanya die off, decrease in volume and sometimes expose bone structures, and teeth begin to loosen. Abundant deposits of soft plaque appear, and the patient suffers from high fever, digestive disorders and general malaise.
At the initial stage, the gum turns white and moves away from the tooth
“I was diagnosed simply during a routine preventive examination. Can you imagine my shock? After the examination, the doctor said that I suspected necrosis of the mucous membrane near one upper tooth. After examination, the diagnosis was confirmed. I went through treatment and everything seems to be fine. Now I don’t miss a single scheduled examination. This is how nothing portends trouble, and therefore, like a bolt from the blue, your gums are dying...”
Natalya V., from correspondence on the forum www.32top.ru
As mentioned above, gum necrosis can be in one of two forms: wet or dry. In the first case, the dead areas dry out and significantly decrease in volume. In this case, signs of inflammation and intoxication are usually absent. The wet form is considered more complex and dangerous, accompanied by swelling and severe hyperemia. As part of treatment, they usually try to make it dry in order to surgically remove the affected areas and stop the spread of the pathology.
Pathogenesis
The reasons for the development of necrosis are most often the negative effects of chemical vapors saturated with acid solutions, improper diet or taking certain medications. In this case, decalcification is observed, that is, the loss of calcium salts by tissues, which reduces the strength of enamel and dental dentin, the formation of cracks, chips or destruction of a large area. Excessive sensitivity and increased abrasion appear. If treatment is not started, the lesion gradually affects the entire coronal part and pulp.
Symptoms:
- pigmentation, the appearance of dark spots on the surface;
- sticking of the lower and upper teeth when closing, which is caused by softening;
- the appearance of uneven contours, breaks and microcracks;
- the enamel surface becomes matte, slightly rough;
- the bite decreases, the gaps between individual units increase;
- dentin acquires a dark, pronounced shade;
- over time, increased sensitivity decreases and disappears;
- destruction gradually begins from the cutting edge to the neck;
- the root cavities are closed, the formation of a volume of replacement dentin is diagnosed.
Necrosis of the gums after the use of arsenic
Previously, such a pathological phenomenon was a fairly common complication from arsenic. Some time ago, this poison was quite widely used in dentistry to kill the pulp and subsequent depulpation - removal of the nerve.
Problem may arise when using arsenic for dental treatment
Until now, some budget clinics use arsenic-based substances, although today there are safer and less toxic devitalizing pastes. So, for example, necrosis from “Depulpin” (arsenic-free pulp killing agent) is an unlikely phenomenon. However, even when using it, it is important to act carefully, in no case exceeding the recommended dosage, otherwise an aggressive effect on surrounding tissues may provoke a similar problem.
Both arsenic pastes and more modern gentle agents have a strong toxic effect, directly related to the disruption of metabolic processes in the treated area - this is their direct purpose. But if excess composition gets on the mucous membrane and is in contact with it for too long, their effect will spread to healthy tissues, resulting in an irreversible process.
How is diagnostics carried out?
Often the problem is identified during a routine dental examination, without complaints from the patient. In other cases, symptoms appear: pain, hyperemia, bleeding. Other common signs of pathology are bad breath, inflammation and swelling of the mucous membrane, deterioration in general health, digestive problems, difficulty swallowing, etc. As part of the diagnostic examination, an X-ray is usually taken and an instrumental examination is performed. Radiography allows not only to identify the necrotic process, but also to assess its extent, as well as determine the stage and possible complications.
X-ray examination allows you to see hidden problems
On a note! Additionally, laboratory examination may be required, for example, microscopic examination of soft plaque. It allows you to study the microflora, identify the possible development of a fungal infection, determine the number of leukocytes, spindle-shaped rods and Vincent spirochetes1.
At the very initial stage, changes in gum tissue are still reversible, but making an accurate diagnosis requires the use of differential techniques to exclude other possible gum diseases. It is also important to identify associated pathological conditions and complications.
Symptoms of the disease
Signs of the disease differ depending on the stage.
Early.
The tissues are slightly affected, darkening of the enamel and pale gums may be observed.
Average
. Swelling of the interdental papillae, a gray coating forms on the mucous membrane, and bad breath appears.
Heavy.
Swelling of the gum tissue - it turns black and ulcers appear on it. Appetite disappears, body temperature rises to 39 C°.
Last
. The epithelium dies, severe pain is felt in the gums, the necks of the teeth are exposed, and the dental units become loose.
Features of treatment of the pathological process
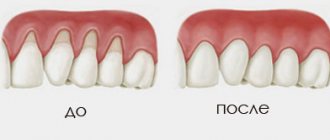
How to treat necrosis directly depends on its form and stage, the presence or absence of concomitant diseases. This is an irreversible process, so the main treatment is aimed at stopping it and stopping further spread. It is important to stop cell death and restore blood circulation. Necrotic areas will have to be removed surgically. Depending on the form of the pathology, there are two treatment tactics:
- dry necrosis - the affected area is treated with antiseptics, after which dead tissue is removed, normal blood flow is established in areas that have not lost their functionality,
- wet – the causative area is treated with a solution of hydrogen peroxide, abscesses and ulcers are opened and drained, and a thorough antiseptic treatment is carried out. All this is necessary to transfer the condition to a dry form. It also happens that 2-3 days after the procedures the patient’s condition worsens, and in this case the affected tissue is removed urgently.
As part of treatment, antibiotics are usually prescribed to prevent intoxication of the body. After the necrotic process has completely stopped, a transplantation - gum grafting - can be performed to restore aesthetics.
After treatment you may need gum surgery
Troubleshooting
Treatment of gum necrosis is selected depending on the stage of the pathology. Cell death is irreversible, so the periodontist directs efforts to restore blood flow to living tissues and stop the process of necrosis. Treatment of the problem area with antiseptics, surgical removal of dead areas, and restoration of normal blood circulation help stop it.
In case of wet necrosis, the necrosis is transferred to the dry stage, treated with antimicrobial drugs, and the abscesses are opened and drained.
Antiseptics and other drugs
The death of gum cells is harmful to the body. It leads to general intoxication, so the patient must be prescribed antibacterial and detox therapy. Treatment is not complete without the following drugs:
- Antibiotics. They fight the increased proliferation of pathogenic microorganisms, which is observed during necrosis.
- Immunocorrectors. Imudon, Ribomunil and other drugs support immune defense against gum necrosis.
- Vitamins. Strengthen the body, improve blood clotting.
- Antihistamines. Erius and other medications are prescribed in combination with antibiotics.
- Antiseptic ointments and gels. Miramistin, Chlorhexidine and others prevent the growth of bacteria in the oral cavity.
Folk remedies
Pathology cannot be defeated using traditional methods. However, it is possible to improve the condition of the gums and stop the spread of inflammation. There are the following recipes for this:
- take 20 grams of boiling water per glass. dry thyme, steam, leave for an hour, strain, rinse,
- make a mixture of dry herbs sage, celandine, St. John's wort (1 to 1), steam with a glass of boiling water, cool, rinse your mouth,
- crush a leaf of golden mustache, pour boiling water, leave, rinse your mouth in the morning.
Preventive measures - how to prevent the development of necrosis
Prevention is based on maintaining oral hygiene and preventing dental diseases. In this regard, experts suggest adhering to the basic rules:
- regularly brush your teeth with an individually selected brush and toothpaste - 2 times a day, rinse your mouth after each meal, use floss and irrigator,
An irrigator is an additional device for maintaining oral hygiene - correct the bite in a timely manner to avoid tissue injury and accumulation of bulky deposits,
- adhere to a healthy diet and a balanced diet, ensure a sufficient supply of vitamins, minerals and amino acids in the body,
- give up alcohol and smoking - these bad habits lead to severe irritation of the mucous membranes and dental tissues, provoke many pathological conditions,
- support the body's immune defense,
- promptly treat diseases of the teeth and gums, as well as systemic pathologies of the gastrointestinal tract and endocrine system, and control diabetes mellitus.
After treatment of necrosis, it is important to provide competent and regular oral care to prevent relapses. It is imperative to regularly visit the dentist’s office for routine preventive examinations - at least 2 times a year.
- Wolf G.F., Rateitskhak E.M. Periodontology, 2008.