From this article you will learn:
- what is periodontium and its functions,
- alternative classifications of periodontal fibers,
- What is the difference between periodontium and periodontitis?
The periodontium is the ligamentous apparatus of the tooth, located in the slit-like space between the bone wall of the alveolus and the root of the tooth (periodontal fissure). Some authors in their works also call periodontium – the term “pericementum”. The periodontium consists of bundles of type 1 collagen fibers that firmly connect the tooth root, covered with a layer of cement, to the compact plate of the alveoli. Destruction of periodontal fibers (for example, during periodontitis) leads to a decrease in the area of attachment of the tooth to the bone and, accordingly, to the appearance of mobility.
The average width of the periodontium (width of the periodontal fissure) is only 0.20-0.25 mm. Moreover, the greatest width is observed in the cervical and apical regions of the tooth root, and the narrowest section, about 0.1 mm, is located in the middle third of the tooth - about 0.1 mm. It turns out that the periodontium has an hourglass shape, which, according to many authors, is a sign of adaptation of the ligamentous apparatus of the tooth to functional loads.
Anatomy of periodontal and periodontal tissues –
Periodontal fibers distribute the pressure exerted on the tooth - in the form of traction on the alveolar bone. Its second main function is to hold the tooth in the alveolus. It should be noted that the rate of renewal of collagen fibers in the periodontium is approximately 2 times higher than in the gums (and 4 times higher than in the skin). The constant restructuring of the fibers helps to adapt the ligamentous apparatus of the tooth to changing loads, but this also explains the possibility of orthodontic movement of the tooth (without disturbing the periodontal attachment).
The formation of periodontium around the tooth root occurs in parallel with the formation of the root. Teeth eruption begins when the root is only 25-50% formed, and therefore the formation of periodontal fibers continues to occur even after the tooth crown begins to erupt through the mucous membrane. Moreover, the growth of periodontal fibers occurs simultaneously - both from the side of the bone wall of the alveoli and from the side of the cementum of the tooth root. The development of periodontal tissue ends only after the end of tooth eruption.
Differences between periodontium and periodontium (Fig. 1-2) –
The periodontium is the entire set of structures that ensure the attachment of the tooth to the bone wall of the alveolus (the surface of the tooth socket). Thus, the periodontal structure includes not only the periodontium, but also the cement of the tooth root, soft gum tissue, and the dental alveolus.
The structure of the periodontium –
As we said above, the periodontium is located between the cementum of the tooth root on one side and the compact lamina of the alveoli on the other side. It consists of loose fibrous connective tissue (FCT), the main component of which is mature type I collagen fibers. Moreover, in people under 25 years of age, in addition to mature collagen, fibers of immature collagen (procollagen) can also be found in the periodontium. Between the bundles of collagen fibers there is an intercellular substance with blood and lymphatic vessels, as well as nerve fibers.
There are no mature elastic fibers in the periodontium, and there are only a small number of immature elastic fibers (oxytalan), which are located along the walls of blood vessels. At the same time, the collagen fibers themselves are rigid and incapable of stretching - so how is the physiological mobility of the tooth formed? The fact is that collagen fibers in the periodontium have a shock-absorbing effect due to their spiral bends. These bends straighten during chewing load on the tooth, and when it stops, they curl again. Thanks to such bends, the tooth has physiological mobility.
Periodontal fibers (histological specimen) –
The cellular composition of the periodontium is represented primarily by fibroblasts, cementoblasts and osteoblasts, which are involved in the construction of collagen, cement and bone tissue, respectively. In addition, Malasse epithelial cells were found in the periodontium, which can be a source of the formation of cysts and tumors. We will talk about the full composition of cellular elements below.
Types of periodontal fibers:
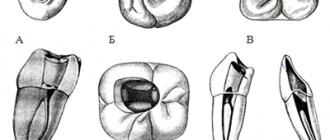
Collagen fibers passing nearby intertwine with each other, forming strong bundles with a diameter of 0.2 mm (such bundles are called periodontal ligaments or ligaments). There are several alternative classifications of periodontal fibers, and below we present two of them. According to the classification of I.P. Gayvoron periodontal fibers can be divided into 3 types (Fig. 2) –
- dental-gingival fibers,
- dentoalveolar fibers,
- interdental fibers.
1) Complex of dental-gingival fibers - bundles of these fibers begin from the cementum of the tooth root in the area of the bottom of the gingival pocket, and then they spread fan-shaped, weaving into the soft tissue of the gums around the neck of the tooth (marginal edge of the gums). This type of fiber ensures a tight fit of the gum to the neck of the tooth. Below you can see that the dentogingival fibers have a variety of directions and form a three-dimensional network in the gum tissue. The structure of these fibers is quite thin and not too powerful.
2) Dento-alveolar fibers (horizontal and oblique) - these fibers begin just below the fibers of the previous group. They are located in the periodontal gap between the cementum of the tooth root on one side and the compact lamina of the alveoli on the other side. Dento-alveolar fibers are usually divided into horizontal and oblique. Horizontal fibers are quite small in number, and they go in a horizontal direction from the surface of the tooth root - to the apices of the interalveolar septa (Fig. 5).
Almost the entire surface of the roots is covered with oblique dento-alveolar fibers, and it is predominantly this type of fiber that holds the tooth in the alveolus and also performs a support-shock-absorbing function. At one end these fibers are attached to the cementum of the root, and at the other to the wall of the alveoli. Due to the oblique direction of the fibers, the tooth is suspended inside the alveolus and, thus, chewing pressure is not directly transmitted from the tooth to the bone tissue of the alveolus. In general, the arrangement of bundles of dento-alveolar fibers in the lateral sections of the periodontal fissure looks like a hammock mesh (Fig. 5-6).
In the middle third of the periodontal fissure (in young people under 25 years of age) there is a dense intermediate plexus of immature collagen fibers - the so-called “Sikcher plexus”. The fibers of this plexus have a very high regenerative potential. They are of great importance for the regeneration of periodontal structures, for example, this can be important when planning orthodontic treatment. But it must be taken into account that the Sickher plexus disappears in people over 25 years of age. A number of researchers have put forward a logical explanation for the need for the presence of immature collagen in the periodontium.
The fact is that part of the periodontal fibers begins to form from the side of the cement of the tooth root, and the other part - from the side of the bone plate of the alveoli. According to a number of authors, periodontal fibers are not a single formation, and when both parts of the fibers reach the middle of the periodontal fissure, they are connected through immature collagen fibers. By the way, this theory is confirmed by the clinical observations of the author of the article, who has repeatedly carried out replantation of teeth completely removed from the socket. At the same time, fragments of periodontal fibers were preserved on the side of the socket and the root of the tooth, thanks to which the periodontium regenerated perfectly in young patients (24stoma.ru).
3) Transseptal (interdental) fibers - these fibers go from the neck of one tooth to the neck of another, and for this purpose the fibers pass over the tops of the interalveolar septa. Those. they form a “ligament” that goes from the cementum of the root of one tooth (on the side of the contact surface) to the cementum of the root on the contact surface of the adjacent tooth. These periodontal fibers perform the function of maintaining the continuity of the dentition, as well as redistributing the chewing load along the dentition.
Alternative classification of periodontal fibers –
There are several alternative classifications of periodontal fibers. These classifications may include the following division of fibers into groups:
- Circular (free) fibers - they start from the neck of the tooth, fan out, ending in the soft tissues of the gingival margin.
- Fibers of the alveolar ridge - they connect the neck of the tooth with the crest of the alveolar bone (in Fig. 4 they are called dentocomb fibers).
- Horizontal fibers are a small group of fibers that are located immediately under the fibers of the alveolar ridge (at the very entrance to the periodontal space). These fibers run horizontally, forming, together with the transseptal fibers, the circular ligament of the tooth.
- Oblique fibers are the most numerous group of fibers that connect the tooth root with the compact lamina of the alveoli (in the previous classification they were called dento-alveolar).
- Apical fibers - they diverge perpendicular to the dento-alveolar fibers from the apices of the roots to the bottom of the alveoli.
- Transseptal fibers - they run horizontally from the neck of one tooth to the neck of another, connecting adjacent teeth to each other.
Anatomy
The histological structure of the periodontium includes the periosteum, alveolar tissue, periodontal ligament, gum and gingival sulcus.
- The periosteum is a dense tissue that is attached to the outer surface of the alveolar process.
- The alveolar process is a spongy bone penetrated by blood vessels and bone marrow.
- The periodontal ligament secures the teeth in the alveoli.
- The gums and gingival sulcus prevent pathogenic bacteria from penetrating into the periodontal gap.
A healthy periodontium is about 0.2 millimeters thick. It consists of elastic collagen fibers, between which are loose connective tissues.
The periodontium is literally permeated with blood vessels, which form the internal, middle and external plexuses and play the role of a kind of shock-absorbing pillow.
- The blood supply is successfully carried out by several longitudinal blood vessels.
- The lymphatic system is located along the small vessels.
- Innervation is carried out by two types of nerve endings - bushy and glomerular nerve endings of pulpal nerve fibers.
The structure of the periodontium under a microscope –
In Figure 8 below you can see collagen fibers penetrating the root cementum. Please note that the terminal sections of the fibers (located in the cement of the root or in the bone wall of the alveoli) are called Sharpey's fibers. Next, Fig. 8 shows a histological preparation of the periodontium of a tooth, where 1 – bundles of collagen fibers, 2 – the main amorphous substance, 3 – periodontal vessels.
Electron microscopy data made it possible to find out that periodontal fibers penetrate into the cement of the tooth root to a depth of only 3 to 5 μ.t, and into the bone wall of the alveoli - no more than 20 μ.t. It also became known that although periodontal fibers consist predominantly of mature type 1 collagen, it also contains some immature elastic fibers (oxytalan). These fibers are only 2-3 mm long, and they are not located perpendicularly like all steel fibers, but parallel to the surface of the tooth root. Oxytalan fibers cross the dento-alveolar fibers at right angles, and their role is to redistribute blood flow in the periodontium under conditions of chewing load.
Collagen fibers occupy only 40% of the periodontal volume, and the remaining 60% is nothing more than the main amorphous substance (which, in turn, consists of as much as 70% water). In addition to water, there is also a large number of different cellular elements present here - first of all, we are interested in fibroblasts, which are located along the collagen fibers. Fibroblasts can also differentiate into fibrocytes or myofibroblasts during the cell cycle.
Another group of cellular elements includes cementocytes and cementoblasts. The latter are located on the surface of the cementum of the tooth root, and their function is to build replacement cement. There is also a small group of cellular elements, which include osteoblasts, osteoclasts, and odontoclasts. The following are also found in small quantities in the periodontium: lymphocytes, plasma cells, mast cells, eosinophils and neutrophilic leukocytes.
Periodontal histology: video
Below in video 1 you can see the histology of tooth tissue in stunning resolution. Video 2 is the best lecture on periodontal histology you can ever hear. The video is in English, but if you wish, you can turn on subtitles, and then select translation from English into Russian in the settings.
Blood supply to the periodontium –
The sources of blood supply to the periodontium are the superior and inferior alveolar arteries. In turn, smaller “dental arteries” branch off from them, which already penetrate the apical openings at the apexes of the roots of the teeth. Before penetrating the apical foramen, its alveolar and periodontal branches are separated from the dental artery. The bone wall of the alveoli throughout its entire length is penetrated by a system of perforated canaliculi, through which smaller arterioles penetrate from the alveolar branch of the dental artery to the periodontium.
Periodontal blood supply diagram –
The vascular network of periodontal tissues of adjacent teeth is combined into a single system, which allows for collateral blood flow. An important point is that periodontal vessels can be connected to intrapulpal vessels - through additional openings on the lateral surface of the tooth root. These may be ways for the infection to spread.
The lymphatic system is formed by capillaries that blindly begin in the intercellular substance of periodontal tissue, and is rather poorly developed. From the periodontium of the teeth of the upper jaw, the outflow of lymph occurs into the parotid lymph nodes, and from the teeth of the lower jaw - into the submandibular and sublingual lymph nodes. This is what explains the increase in certain groups of lymph nodes, for example, during exacerbations of chronic periodontitis.
Innervation of the periodontium –
It is carried out from the side of the trigeminal nerve, the afferent and efferent fibers of which form a plexus in the periodontal tissues. The endings of these fibers are pain receptors and mechanoreceptors. In most teeth, the maximum concentration of receptors is concentrated in the area of the root apices, but in the periodontium of the incisors, the receptors are evenly distributed throughout the periodontium. Sympathetic nerve fibers responsible for regulating blood flow are also found in the periodontium.
Classification of periodontal diseases.
As Carl Linnaeus said, knowledge begins with classification. And the most popular classification in the world is the International Classification of Diseases (ICD-10)
- By 05.3 chronic periodontitis;
- By 05.2 acute periodontitis:
- other.
- desquamative;
- ulcerative;
- hyperplastic;
- simple marginal;
- By 05.1 chronic gingivitis:
- K.05.0 acute gingivitis.
- simple;
- difficult;
- other.
- By 05.4 periodontal disease.
- By 05.5 others.
- By 05.6 unspecified.
- By 06.0 gum recession.
As you can see from the classification, the main periodontal diseases are gingivitis, periodontitis and gum recession. Now we will briefly tell you what kind of animals these are.
Functions of periodontium –
- Retaining function - it consists in holding the tooth in the alveolus, and the dento-alveolar fibers of the periodontium are primarily responsible for this.
- Shock absorption and distribution function - intercellular substance and periodontal fibers allow you to evenly distribute the chewing load from the tooth to the alveolar tissue.
- Protective function - the connective tissue and cellular components of the periodontium represent the so-called “histohematic barrier”, which ensures the structural and antigenic homeostasis of both the periodontium itself and the surrounding tissues. The implementation of the protective function is mediated by both specific and nonspecific protective factors.
- Plastic function - ensures the preservation of the structure of the periodontium, as well as the reparation of both the periodontium itself and adjacent tissues (for example, the bone plate of the alveolus, as well as the cement of the tooth root). The periodontium is very rich in cellular elements, including osteoblasts, which are responsible for the formation of bone tissue on the surface of the alveoli, as well as cementoblasts, on which the production of replacement cement for the tooth root will depend.
- Trophic and sensory functions are provided by a well-developed vascular and nervous network (a large number of receptors). These functions are closely related to those listed above.
Functions
- supporting and holding. Perception and redistribution of pressure during chewing.
- reflexogenic. Regulation of chewing loads due to the fact that the periodontium contains many nerve endings.
- plastic. Promotes the restoration of ligaments and the formation of alveolar walls. Performed by osteoblasts, cementoblasts and fibroblasts.
- trophic. It is carried out with the help of nerves and capillaries and is associated with chewing pressure.
- barrier It is performed with the help of histiocytes, which do not allow pathogenic bacteria to penetrate into the tooth root area.
- sensory.
Additionally, we note that without periodontium, teething in infants is impossible; it regulates the adaptation of the tooth to the stresses that arise during chewing and biting food, performs a reparative function in the event of a tooth root fracture, and also provides root protection with the help of leukocytes and macrophages.