Dental clinic No. 2
In order to always anticipate surprises, the doctor must be prepared to expand access to the dental cavity to facilitate the preparation of complex root canals and carefully examine the floor of the tooth cavity to look for such anatomical variations.
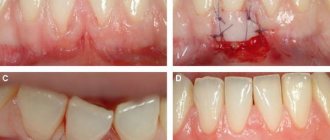
Endodontic dogma is that careful cavity and root canal preparation and obturation is the key to successful canal therapy. Endodontic preparation can be divided into cavity preparation (coronal preparation) and root canal preparation (radicular preparation). Transferring the principles of preparation of carious cavities according to Black in relation to endodontics, the following endodontic principles of preparation can be distinguished: creation of external, comfortable, retention (holding) and resistant forms. A complete preparation along the entire length of the tooth is the external form. In turn, the external shape can be modified for a comfortable shape to accommodate anatomy, canal curves and instrumentation. In some endodontic techniques, the canal can be prepared with slight retention of the first gutta-percha point (retention form). But the most important is the resistant form, in which the so-called “apical stop” is prepared in the apical section, a barrier that protects the tissues of the apical periodontium from the removal of the filling material and irrigating solution beyond the apex and creates a limit for the compaction of gutta-percha in the canal (Fig. 1).
| pic 1 |
Basic tools for preparing a tooth cavity. For trephination of an intact tooth crown, Ingle JI suggests using a cone-shaped fissure bur with a working rounded top for a turbine tip (Fig. 2 B). It is first directed at a right angle in the long axis of the tooth to remove only the enamel. Then it should be located parallel to the longitudinal axis of the tooth (Fig. 2 C, D). The roof of the tooth is removed using a low-speed tip with a round bur (Fig. 2 E, F) No. 2, 4 less often No. 6 of regular length (9 mm) for molars and premolars or surgical length (14 mm) for incisors and canines. The protrusion (“shoulder”) inside the cavity of the anterior teeth, which prevents the direct passage of the endodontic instrument into the root canal, is eliminated using a long, conical diamond bur on a turbine drill (Fig. 2 G). The remaining pulp from the pulp chamber is removed using a spherical bur No. 1 or 2 (Fig. 2 H).
| pic 2 |
It is necessary to remember the following axioms of the structure of the coronal cavity of the tooth and root canals when searching for root canal orifices (Ingle JI). 1. The two root canal orifices of the first maxillary premolars are located further buccal and lingually than is usually realized (Fig. 3 A). 2. The orifices of the mesiobuccal canals of the upper and lower molars are located under the mesiobuccal cusps, and the external shape should often be more expanded due to these cusps (Fig. 3 B, C). 3. The mouth of the palatal canal in the upper molars is located not so far to the palatal wall of the tooth cavity, but in the center of the medial half of the tooth (Fig. 3 B). 4. The orifice of the distal-buccal canal of the upper molars is not located so distally-buccally, but almost directly to the buccal side of the palatal canal (Fig. 3 B). 5. The orifice of the distal canal in mandibular molars is not so distally located, but in fact almost exactly in the center of the tooth (Fig. 3 C, E). 6. The orifice of the mesial-lingual canal of the lower molars is not so far mesial-lingual, but in fact directly buccally from the orifice of the distal canal (Fig. 3 B). 7. Certain anatomical variations that occur quite often: The mesial buccal root of the maxillary first molar often (up to 95% [4]) has an additional mesiopalatal canal located exactly oral to the orifice of the main canal. The mouth of the additional channel is located in the groove, which forms the mouth of the main channel like a “comma tail”. This entire groove should be examined to locate the mouth of the accessory canal (Fig. 3 B). The lower second molar often has a common mesial orifice, which divides approximately 1 mm below the floor of the dental cavity into mesial buccal and mesial lingual canals (Fig. 3 D). The lower first and second molars may have two distal canals with separate orifices or a common one. orifice, like the previously described medial canals (Fig. 3 E). The mandibular first premolar often has a second canal that branches off from the main canal buccally or lingually a few millimeters below the floor of the dental cavity (Fig. 3 E). The lower incisors and canines often have two canals. The medial lingual canal is hidden under the internal protrusion (“shoulder”), which corresponds to the lingual girdle. This protrusion should be removed with a #2 long shank round bur or finishing diamond cone bur to allow proper exploration of the root canals (Figure 3 G).
| pic 3 |
Table 1. Degree of deviation of teeth from the central axis
When preparing a tooth cavity, it is necessary to take into account the degree of deviation of the tooth from the central axis in the vestibulo-oral and medio-distal projections (Table 1). The upper incisors and canines are inclined palatally by 29°, the lower incisors are inclined lingually by 20°. The lateral lower and upper incisors are deviated medially at 17 and 16? respectively. If the doctor does not know about these deviations or ignores them, then he can make a perforation and a ledge on the walls of the tooth cavity (Fig. 4. A, B, C)
| pic 4 |
Table 2. Incidence (%) of root canals.
For successful endodontic treatment, it is also extremely important to know the variations in the number of root canals in order to avoid the error of missing a canal. Although back in 1921, Hess W., studying 513 teeth, indicated that four canals were found in 54% of the first molar, this fact was ignored. F. Pineda, J. Cutler (1972), studying the medial buccal roots of the first molars, found that in 39% of cases this root has one canal, in 61% - 2 canals. Later studies (J.K. Kalild and D.D. Peter, 1990) showed that in a study of 51 medial buccal roots of the upper first molars, a two-canal variant of the structure was identified in 95% of cases. Table 2 summarizes information from various authors about the frequency of occurrence of additional channels. As follows from this table, in the lower incisors, canines and premolars it is always necessary to look for the second canal, and the first upper molar should be considered a four-canal. Lower premolars can be extremely difficult teeth to treat endodontically. Two narrow canals are usually located vestibulo-orally; division into two roots can occur in the apical third. At higher magnifications, it is often possible to view more complex anatomy. The dentist’s knowledge of the anatomy of the tooth cavity and root canals is an important part of endodontic treatment, guaranteeing the success of the treatment and avoiding errors and complications.
Author: Trigolos N.N.
Apical periodontitis of the tooth - what is it?
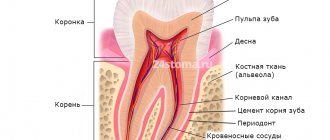
The diagnosis of periodontitis is made when the patient's periodontal tissues near the apex of the tooth root become inflamed, which is why it is called apical. It affects deep gingival and bone structures, so it is not easy to treat - unlike, for example, caries. Nevertheless, this disease requires immediate intervention, because if the patient is not in a hurry to treat apical periodontitis, then he risks encountering unpleasant consequences of the disease: the appearance of granulomas and cysts, destruction of the alveolar bone, and in the most severe cases, even sepsis.
Diagnosis of apical periodontitis
It should be remembered that the symptoms of apical periodontitis are similar to the symptoms of some other oral diseases: pulpitis, sinusitis, hilar cyst and others. To make an accurate diagnosis, the following studies are necessary:
- electroodontometry
- helps to assess the degree of pulp necrosis; - radiography
- allows you to see tissue changes in the apical region; for chronic apical periodontitis, x-ray is the best diagnostic method, but it may not detect acute inflammation at an early stage; - A blood test
is an additional diagnostic method. With apical periodontitis, an increase in the level of leukocytes and ESR is observed.
Types and symptoms of apical periodontitis
Depending on how the inflammatory process proceeds, two types of disease are distinguished: acute apical periodontitis and chronic apical periodontitis. The second is always a consequence of the first: if acute inflammation is not cured in time, then it has every chance of becoming chronic.
The symptoms of acute apical periodontitis of pulpal origin are difficult to miss - they can cause the patient many unpleasant moments. The acute period is usually accompanied by the following conditions:
- nagging pain in the area of the affected tooth, which intensifies over time, becomes pulsating, and can radiate to other parts of the face;
- swelling of soft tissues, enlarged lymph nodes;
- rise in temperature;
- headache.
The duration of acute apical periodontitis ranges from 2 days to 2 weeks. In the absence of appropriate treatment, two options are possible: either the disease will progress, involving more and more tissue, or it will enter a chronic stage. The clinic of chronic apical periodontitis looks like this:
- pain in the affected area is mild or absent altogether, and can also occur when pressing or biting;
- slight tissue swelling may be observed;
- Possible bad breath;
- the diseased tooth is sensitive to temperature influences.
The chronic course of the disease may be accompanied by acute periods. With exacerbation of chronic apical periodontitis, the same symptoms are observed as in the acute form.
Apical periodontitis: pathogenesis
Why does inflammation appear in the peri-root zone? Pathogenic bacteria in tissues are the most likely cause of apical periodontitis. It is called an infectious form of periodontitis, it is a logical continuation of untreated caries, which subsequently develops into pulpitis. If the patient continues to ignore the symptoms and does not seek treatment, the pulp dies, allowing pathogenic bacteria to enter the periodontium through the apical foramen.
Another cause of the disease can be mechanical damage - a blow, bruise, displacement or fracture of a tooth. Then the patient is diagnosed with traumatic periodontitis.
The third reason is the penetration of caustic, potent substances into the peri-root tissue, for example, medications. Almost always this is a consequence of a medical error, most often - inaccurate treatment of pulpitis. Such cases are called drug-induced apical periodontitis.
Possible complications after cyst removal
Removing a cyst is a necessary procedure; the longer the treatment of a cyst is delayed, the more likely complications are to develop. There is no need to be afraid of removing a cyst; according to statistics, the percentage of possible adverse consequences is immeasurably less than complications from an unoperated cyst (abscess, phlegmon, sepsis).
After cystectomy, the service life of the tooth is not reduced. Both after therapeutic and surgical treatment of cysts, dynamic monitoring of the condition of the bone tissue is required.
To avoid complications, it is important to maintain oral hygiene, follow your dentist's recommendations, as well as eat a healthy diet and avoid alcohol, smoking, carbonated drinks and solid foods in the first days after surgery.
Treatment methods for apical periodontitis of the tooth
How to treat chronic apical periodontitis and how does the treatment method for acute apical periodontitis differ? In both cases, the patient will need several visits to the doctor, since the therapy is carried out in several stages.
- The first stage:
opening the tooth, thoroughly cleaning the dental canals from the remains of necrotic pulp and areas affected by caries. Expansion of channels. - Second stage:
relief of inflammation. It is produced by filling the channels with antiseptic and anti-inflammatory materials. Additionally, the doctor may prescribe medicinal rinses, and in advanced cases, a course of antibiotics. - Third stage:
filling the canals and monitoring the results of treatment using radiography.
In particularly difficult cases, surgical intervention may be required to gain access to the affected root through an opening in the alveolar bone. If none of the treatment methods brings results, the tooth is removed.
Classification of pulpitis
In dentistry, pulpitis is divided into varieties, each with its own characteristics. Each one can be identified with the help of serious diagnostics. Types of pulpitis:
- Spicy:
- focal;
- diffuse.
- Chronic:
- fibrous;
- gangrenous;
- hypertrophic or proliferative;
- chronic with exacerbation.
Exacerbations of chronic pulpitis are difficult to diagnose. They are often mistakenly interpreted as one of the forms of acute pulpitis. In such cases, the history of the disease (history) plays an important role.