Mandibular anesthesia by palpation
The target point is the mandibular foramen, through which the inferior alveolar nerve enters the canal, located on the inner surface of the ramus of the mandible. Location of the mandibular foramen .
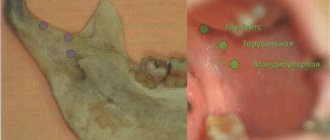
The distance from the edges of the lower jaw: from the anterior edge of the lower jaw - 15 mm, from the posterior - 13 mm, from the semilunar notch - 22 mm and from the lower edge of the lower jaw - 27 mm (Fig. 93, A). Rice. 93. Lower jaw. A - lower jaw from the outside, slightly in front and above (V.P. Vorobyov, 1946): - articular process; 2— coronoid process; 3 - anterior edge of the lower jaw branch; 4 - mandibular eminence (torus); 5—temporal scallop; 6— retromolar fossa; 7 - mandibular foramen; 8 - tongue of the lower jaw; 9 - mental foramen. B - branch of the lower jaw: 1 - inferior alveolar nerve, 2 - internal pterygoid muscle.
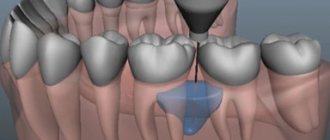
The height of the hole in adults corresponds to the level of the chewing surface of the lower molars, in children and the elderly it is slightly lower. From below and in front, the mandibular foramen is covered by a bony protrusion (tongue of the lower jaw). In this regard, the anesthetic solution must be injected 7-10 mm above the level of the hole, where the nerve, before entering the mandibular canal, passes through a bone groove filled with loose fiber and in which the anesthetic spreads well. CONCLUSION : to approach the target point, the needle must be inserted 7-10 mm above the level of the chewing surface of the lower molars (Fig. 94, A).
Rice. 94. Needle position for mandibular anesthesia . (G.P. Ruzin, M.P. Burykh, 2000) A - on the mandibular bone. The needle passes 7-10 mm above the chewing surface of the lower molars, the end of the needle is located in the pterygo-maxillary space in the bone groove (sulcus n. mandibularis). 1 — level of the chewing surface of the lower molars; 2—tongue of the lower jaw; 3 - pterygomaxillary space. B - on a vertical section. B - on a horizontal section of the preparation.
Injection equipment (for all types of intraoral mandibular and torusal anesthesia): carpule or disposable plastic syringe 2 ml, needle 41.5-50 mm long.
Technique for mandibular anesthesia using palpation
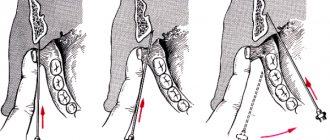
1. The patient opens his mouth as wide as possible. 2. The finger is fixed in the retromolar fossa (see Fig. 95A, B, C): for right-sided mandibular anesthesia - the index finger of the left hand, for left-sided - the thumb. The injection to the right and left is performed with the right hand. First, the retromolar fossa is found. A bone cord descends from the coronoid process to the lingual side of the alveolar process of the lower jaw - the temporal crest; between the anterior edge of the lower jaw and the temporal crest there is a small triangular depression - the retromolar fossa. With the patient's mouth wide open, use your finger to find the anterior edge of the mandibular ramus at the level of the distal edge of the crown of the third lower molar (if it is absent, immediately behind the second molar). Moving the finger a little in the middle, they fall into the retromolar fossa. The finger is fixed in the retromolar fossa so that the tip of the nail probes its inner edge (the pedicle of the temporal ridge) (Fig. 95, A). 3. The syringe is located at the level of the premolars of the opposite side. 4. The needle is inserted near the edge of the nail, to the middle of the stem of the temporal ridge, 7-10 mm above the chewing surface of the third lower molar. 5. The needle is advanced posteriorly, at a depth of 5-7 mm it reaches the bone, 0.3-0.5 ml of anesthetic is injected, turning off the lingual nerve. 6. Without losing contact with the bone, advance the needle another 20-25 mm posteriorly, perform an aspiration test, and inject 1.5-2 ml of anesthetic. Pain relief occurs within 5-10 minutes (Fig. 95 D).
Rice. 95. Intraoral mandibular anesthesia using palpation . The finger descends from the outer edge of the mandibular ramus into the retromolar fossa. A, B, C - palpation of the anterior edge of the lower jaw branch; G—syringe is located at the level of the premolars of the opposite side. The injection site is 10 mm above the chewing surface of the third lower molar
Note : If, due to the anatomical features of the lower jaw, contact with the bone is lost when advancing the needle, the syringe is moved to the incisors. A prerequisite for success is that the needle, having reached the bone, when advancing at a distance of 20-25 mm, should not lose contact with it. At the moment of administering the anesthetic, the tip of the needle must touch the bone. Anatomical features of the lower jaw .
The branch of the lower jaw is not located strictly in the sagittal plane, but somewhat at an angle to it, with its anterior edge being closer and its posterior edge further from the midline. The level of inclination of the jaw branch is different for each patient, therefore, by injecting a needle into the bone 5-7 mm, it is not always possible to advance it to the target point - the bone groove above the mandibular foramen. In this case, the syringe is moved to the incisors, the needle is advanced to a depth of 20-25 mm without losing contact with the bone, and the target point is reached.
Complications
Carrying out any local anesthesia technique can result in complications of varying severity. This depends on two factors:
- doctor's qualifications;
- patient's health.
A qualified dentist will be able to carry out the manipulation as accurately as possible and in compliance with all safety measures for the patient. Also, a qualified dentist is well aware of the anatomical features of the structure of the skull of people of various age categories.
Types of complications:
- needle fracture due to non-compliance with the technique of introducing the solution by the dentist;
- paresis of the facial muscle;
- contracture of the pterygoid muscle;
- damage to vascular walls;
- numbness of the molars of the lower jaw;
- oral infection;
- ischemia of soft tissues due to deformation of the vessel with a needle;
- temporary blindness;
- post-injection abscesses and phlegmons.
A needle fracture occurs due to a gross violation of the instillation technique by the dentist. This can happen either due to inattention or due to little experience as a doctor. The remaining needle is removed from the tissue surgically in the operating room.
For patients suffering from neurological and mental diseases, local anesthesia using intraoral and extraoral injections is prohibited. Other types of pain relief are intended for them.
Paresis of the facial muscle occurs due to the entry of the anesthetic solution into the trunk of the facial nerve. This occurs due to the needle being immersed unreasonably deep into the tissue. Half of the patient’s face turns stiff literally a couple of minutes after the solution is administered. However, this pathological picture is not always dangerous to health: paresis can go away on its own after a few hours.
Contracture of the pterygoid muscle leads to a pathology in which it loses its ability to contract. To restore lost muscle functionality, physiotherapy and therapeutic massage are prescribed. The muscle recovers quickly if you conscientiously visit the office of a physiotherapist and massage therapist.
Temporary blindness occurs immediately after the administration of the anesthetic. The patient complains that he sees nothing. This condition may last more than an hour, but subsequently vision is completely restored.
Abscesses and cellulitis are common complications after injections. This is due to a violation of the sterility of the instillation process or the patient’s failure to comply with sanitary standards after surgery in the maxillofacial area. An abscess requires professional treatment: opening, removing purulent contents and suturing (if necessary). You should not treat any purulent infections yourself: this risks spreading the infection to healthy tissue.
To prevent possible complications, which often include an allergic reaction to drugs, you need to warn your dentist in advance about your illnesses and special sensitivity to novocaine or other drugs.
Complications associated with the patient's neurotic condition
Some patients experience so much pain that the condition causes dangerous post-operative complications. These include:
- syncope - anemia of the brain;
- collapse - temporary acute heart failure.
Syncope
Syncope occurs reflexively as a response to fear associated with upcoming pain at the sight of tools, etc. d. It can occur both during treatment and after it.
Symptoms of brain anemia:
- darkening of the eyes:
- pale skin;
- sticky sweat;
- loss of consciousness.
In this case, you need to urgently unfasten the top buttons to ensure full breathing, and let them smell ammonia on a cotton swab. If the patient has lost consciousness indoors, it is necessary to ensure a flow of fresh air: open a window or vent in winter. After 2-3 minutes the patient regains consciousness. If this does not happen, you need to perform artificial respiration and administer cardiotonic drugs.
How to prevent syncope (anemia of the brain):
- conduct psychological preparation before visiting the dentist’s office;
- qualitatively anesthetize all facial tissues before dental procedures;
- eliminate negative emotions that provoke nervousness.
Apodactyl mandibular anesthesia (well-known method)
When performing anesthesia using the apodactylic method, the main landmark is the pterygomaxillary fold. It is located in the middle of the temporal ridge and can be wide, narrow, or have a normal (medium) transverse size. 1. The patient opens his mouth as wide as possible. Using a dental mirror, held in the left hand, move the corner of the mouth and the cheek in the middle. Injection site : behind the lower molars the pterygomaxillary fold is visible, laterally (behind this fold) there is a groove, which is divided into three equal parts and an injection is made in front of it between the upper and middle thirds of its length 10 mm above the chewing surface of the lower molars (Fig. 96) . 2. The syringe is placed on the premolars or on the first lower molar, the needle is directed perpendicular to the plane of the lower jaw branch; for this, the syringe barrel must be used to move the corner of the mouth posteriorly. 3. The needle is deepened into the soft tissue by 20-25 mm until it touches the bone. An aspiration test is performed and 1.5-2 ml of anesthetic is injected. Pain relief occurs within 5-10 minutes.
Rice. 96. Apodactyl mandibular anesthesia (N. Evers, G. Haegerstam, 1990): - the cheek is moved to the side with a dental mirror; — the syringe cylinder pulls the corner of the mouth posteriorly, the syringe is located at the level of the lower molars of the opposite side; — there is a mark on the cannula from the side of the needle tip (the cut of the needle is directed towards the bone). DISADVANTAGES: anesthesia is performed with a short needle 25 mm long. If the needle is fractured in the cannula area, the fragment is difficult to remove from the soft tissue (surgery may have to be used)
Apodactyl mandibular anesthesia according to A. E. Verlotsky
It is performed similarly to the previous anesthesia. Injection site : the outer part of the pterygomaxillary fold in the middle of the distance between the chewing surfaces of the upper and lower molars (in the absence of molars - in the middle of the distance between the posterior ends of the alveolar processes of the lower and upper jaws). If the width of the pterygomaxillary fold is significant, the needle is inserted in its middle. If this fold is narrow and located near the mucous membrane of the cheek, the needle is inserted into its inner edge (Fig. 97).
Rice. 97. Apodactyl mandibular anesthesia according to A.E. Verlotsky (V.I. Zausaev et al., 1981)
Note : apodactylic methods of mandibular anesthesia are not very common in the USA and Europe, since dentists consider this technique to be inaccurate. Anesthesia zone for mandibular anesthesia : all teeth of the corresponding side of the jaw, alveolar process, gums on the vestibular and lingual sides, mucous membrane of the floor of the mouth, anterior 2/3 of the tongue, half of the lower lip, skin of the chin on the side of anesthesia. On the vestibular side, the gums from the middle of the second premolar to the middle of the second molar are innervated by the buccal nerve. To anesthetize them, you need to turn off the buccal nerve or additionally inject 0.3-0.5 ml of anesthetic into the transitional fold near the corresponding tooth. Anesthesia of the incisors and canines is incomplete due to the anastomoses of the opposite side (Fig. 98 A).
Rice. 98. A - zone of anesthesia during mandibular anesthesia . B - zone of anesthesia during torusal anesthesia (explanation in the text)
Duration of anesthesia : from 1.2-2 to 4-6 hours (when using a medium-acting anesthetic (lidocaine), anesthesia lasts an average of 2 hours, when using a strong anesthetic (articaine) - 4-6 hours. Application : for long-term, traumatic interventions (operations) on the teeth and in the area of the alveolar process of the lower jaw, during inflammatory processes (periostitis, osteomyelitis), during interventions on the lower molars. COMPLICATIONS :
1. Contracture of the lower jaw. Occurs when a low-quality anesthetic solution is administered, when the pterygomaxillary muscle is injured (insertion of a needle medial to the pterygomaxillary fold, repeated, 2-5 times, repetition of anesthesia with subsequent injury to the muscle, periosteum and bone). 2. Damage to blood vessels with the formation of a hematoma, entry of anesthetic into the bloodstream, injury to the inferior alveolar nerve. 3. Fracture of the needle in the cannula area. Prevention of complications Mandatory aspiration test. Do not use low-quality (little-known companies) and short needles, use needles 41.5-50 mm long, then the needle fragment can be easily grabbed with a tool (tweezers, clamp) and immediately removed from the soft tissues.
Scope of application in dentistry
Mandibular anesthesia is used before any manipulation that is accompanied by pain:
- elimination of carious cavities;
- root canal treatment;
- extraction of teeth, including impacted ones;
- opening of abscess foci to extract pus;
- removal of sequesters;
- excision of the mucosal hood during teething;
- removal of cystic formations and tumors in the mobile jaw area;
- splinting for jaw fractures.