Tooth extraction is a process that traumatizes the gums. After healing a diseased tooth, nerves, ligaments and small blood vessels are torn, which causes bleeding. This is a natural process - the blood does not allow pathogenic organisms to enter the circulatory system, washing them out. And then, curled up, it forms a barrier between unprotected tissues and bacteria. After tooth extraction, white plaque on the gum is not pus, but another stage of protection and restoration of the body.
When removing a tooth, the patient must be prepared:
➢
to moderate bleeding that may last for some time;
➢
the appearance of a dense blood clot in the gum;
➢
unpleasant odor 10-12 hours after surgery;
➢
the formation of a white coating on the blood clot;
➢
pain after surgery;
➢
temperature rise.
The listed symptoms are not a sign of an unsuccessful operation or infection in the body - this is the body’s natural response to tooth extraction.
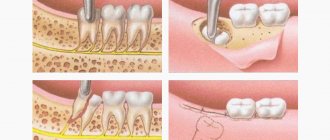
What is white plaque on the wound after tooth extraction?
A few hours after the tooth is removed, a dark clot appears in the socket - bluish, black, red or brown. This clot is blood, and it is the primary protection of the socket from bacteria or pieces of food entering it. On the 2nd - 4th day, the patient may see that a coating appears on the clot - yellowish, gray or white. The deposit looks like pus and, together with the resulting bad breath, can alert the patient. However, there is no need to be alarmed - this plaque is not a sign of wound decay and indicates a normal healing process. This special protein compound is fibrin.
A milky plaque (fibrinous) can be very dense, hard or soft. This is no cause for concern. If you come to the dentist with this question for an unscheduled appointment, the specialist will tell you that everything is in order and there is no need to remove the film.
If the film is not removed and the wound is not disturbed, active processes will occur underneath it:
- the blood clot will begin to dissolve;
- the hole will begin to decrease in size;
- young cells, osteoblasts, will begin to move from the edge of the wound to the center;
- The gums will begin to close the wound.
Fibrinous plaque after tooth extraction is a natural stage of gradual recovery of the body, in which it is better not to interfere.
Stages of alveolitis
All these symptoms of alveolitis cannot appear at the same time. Signs of the disease accumulate, alternate, or overlap as inflammation progresses. Symptoms help determine the stage of the disease.
Serous alveolitis
It develops 72 hours after tooth extraction. The main symptom is aching pain that intensifies while eating. Body temperature is not elevated, regional lymph nodes are not enlarged. Upon examination, pieces of food and saliva are found in the hole, but there may not be a blood clot there, or it may be partially destroyed. Serous alveolitis continues for a week, and if left untreated, it turns into a purulent form.
Purulent alveolitis
Occurs 10 days after tooth extraction. By this time, the pain from alveolitis has already become so intense and constant that it is impossible to eat. In this case, unpleasant sensations spread along the branches of the trigeminal nerve. The soft tissues of the affected area swell, and mouth opening is limited. The patient feels weak and unwell, his temperature rises (up to 38 degrees) and a putrid taste and smell appears in the mouth. Upon examination, you can see redness, swelling, a dirty gray coating, and the alveolar process is thickened on both sides of the socket.
Chronic purulent (hypertrophic) alveolitis
As the disease becomes chronic, the pain begins to gradually subside, body temperature normalizes, and the patient’s general condition noticeably improves. The soft tissue in the area of the inflamed hole grows, and pus is released from it. The gums at the site of inflammation are swollen and have a bluish tint.
Alveolitis can occur not only in adults, but also in children. If a child has had a permanent tooth removed, parents need to carefully monitor compliance with the doctor’s recommendations.
Why you don’t need to remove white plaque after tooth extraction
In some cases, patients intentionally or accidentally remove a blood clot or fibrinous film from the socket. This is not necessary, since removing a clot or film can provoke negative processes.
First of all, an open wound provides access for bacteria to the circulatory system and tissues of the maxillofacial apparatus. Infection can cause serious consequences and require long-term treatment with antibiotics. Also, removing the clot and white plaque increases the pain, since an open wound is more sensitive to any irritants, including drinking drinks and food, during a conversation.
Finally, plaque on the gums after tooth extraction does not need to be cleaned off because this can cause re-bleeding and prolong the wound healing stage.
In any case, there is no need to intentionally remove plaque; this can cause:
- serious complications;
- severe pain;
- improper gum formation;
- long recovery process after tooth extraction.
To avoid accidentally damaging the socket, blood clot or fibrinous film, you must follow the recommendations given by the doctor after the operation.
Alveolitis of the tooth: treatment
The treatment of alveolitis after tooth extraction must be taken seriously, since the disease will not go away on its own, and its consequences can be very serious:
- blood poisoning
- abscess
- osteomyelitis
- phlegmon
- periostitis
Only an experienced dental surgeon will create an effective treatment plan. It is better to start it when the first signs of the disease appear. The treatment process may include:
- numbing the affected area using anesthesia
- washing the hole with warm antiseptic solutions
- removing particles of tissue decay that remain after washing using a sharp surgical spoon
- treatment with a sterile cotton swab
- applying a gauze bandage with iodoform impregnation or an anesthetic and antiseptic bandage
- impregnation of soft tissues at the site of inflammation with anesthetic and lidocaine
- application of antiseptic tampons, hemostatic sponge with kanamycin
- removal of dead tissue
- microwave therapy, fluctuarization, infrared laser beams, ultraviolet irradiation
- prescribing vitamins, analgesics and sulfa drugs
- antibiotic therapy
With proper treatment of serous alveolitis, the inflammatory process subsides after 3–4 days.
A week after the pain disappears, the walls of the socket begin to heal and become covered with new mucous tissue. After 14 days, the swelling subsides and the mucous membrane takes on a normal pink color. After treatment of purulent alveolitis, the wound heals within 1–2 months, and tissue restoration takes about six months.
How not to damage white plaque after wisdom tooth removal
To eliminate the risk of complications and speed up the recovery process, you need to follow the rules of behavior after tooth extraction:
- do not eat or drink for 3 hours after surgery;
- stop smoking and drinking alcohol for a while;
- do not heat the cheek and gums, avoid overheating;
- for the first 24 hours, do not rinse your mouth or brush your teeth;
- Do not go to the bathhouse for a week, do not play sports.
Smoking is contraindicated, as it provokes vasospasm: the bleeding stops too quickly, the blood clot is not formed enough. Hot drinks, warming the cheek, sports training and visiting a bathhouse cause overheating of the body and dilation of blood vessels, which can cause re-bleeding, opening and infection of the wound.
Rinsing and brushing the mouth are acceptable 24 hours after tooth extraction, but they should not be overly vigorous. Hygienic procedures must be moderate so that the blood clot remains in the cavity and the subsequently formed fibrinous protective layer is not damaged. During the recovery period, food should be chewed only on the non-operated side of the jaw.
If you have a fever and severe pain in the first few days after tooth extraction, you can take Paracetamol - this will help reduce discomfort and improve your well-being.
Tooth extraction itself is an unpleasant procedure. And if complications arise, such as alveolitis, then the patient’s mood deteriorates even more. In order to prevent its occurrence, you need to know everything about this unpleasant disease. We will tell you what you need to know about the causes of alveolitis, its types, first symptoms and treatment methods.
What it is
Alveolitis of the tooth socket is an inflammatory disease that occurs after tooth extraction as a result of infection of the wound. If the operation was difficult, with injury to the gums and the tooth socket itself, then the risk of complications increases significantly. Normally, the hole after tooth extraction heals within one to two weeks, but with alveolitis this process takes a long time.
Since the disease occurs when an infection enters the wound, in order to prevent complications from occurring, it is necessary to carefully monitor oral hygiene after the tooth extraction procedure.
Alveolitis can occur before the tooth extraction procedure as a result of infection.
Causes
Alveolitis of the socket most often occurs after tooth extraction and is considered its main complication. However, it does not always occur. In order for this complication to arise, a confluence of certain circumstances is necessary.
The main causes of alveolitis are:
- destruction of the blood clot that forms after tooth extraction and prevents infection from entering the wound;
- getting plaque, stone, or bone fragments into the hole during removal;
- unscrupulous cleansing of the hole by a doctor from granulomas and granulations;
- violation of sterility during surgery;
- too traumatic removal;
- failure on the part of the patient to comply with all the doctor’s instructions;
- reduced immunity and exhaustion of the patient’s body.
After tooth extraction, you should not rinse your mouth too vigorously, as you can wash out the formed blood clot from the hole; this threatens the entry of pathogenic microbes into the wound, which cause inflammation.
Symptoms
The first signs of alveolitis usually appear 2-3 days after the procedure. The symptoms of the disease cannot be confused with anything. This is, first of all:
- severe pain in the area of the extracted tooth;
- constant intensification and spread of pain to adjacent areas of the oral cavity;
- fever up to 38.5° C, chills and general deterioration of health;
- the appearance of bad breath;
- inflammation, swelling and redness of the gums;
- absence of blood clot;
- the presence of a specific gray plaque;
- enlargement of the submandibular lymph nodes;
- presence of purulent exudate.
If one or more symptoms of the disease appear, you must immediately consult a dentist, since alveolitis does not go away on its own, it must be treated as soon as possible. Otherwise, complications are possible.
Diagnostics
The diagnosis of “alveolitis” can only be made by a doctor after a thorough examination of the patient’s oral cavity. Do not self-diagnose under any circumstances! This is a serious disease that, without proper treatment, can cause more dangerous complications, including blood poisoning. The absence of a blood clot in the socket at the site of the extracted tooth in the presence of other symptoms of the disease is decisive when making a diagnosis.
Treatment
If treatment for alveolitis is started in time, the disease usually goes away within a few days. Treatment usually consists of the following:
- thorough removal under local anesthesia of the remaining blood clot at the site of the extracted tooth;
- treating the walls of the socket with a dental instrument until slight bleeding appears;
- further treatment with a special antiseptic raster to prevent the spread of infection;
- the use of antibiotics (usually in the form of a powder that is sprinkled on the hole);
- prescription of painkillers;
- rinsing the mouth with antiseptic solutions;
- physiotherapeutic procedures aimed at speedy healing of the wound.
One of the most common complications of alveolitis, if not treated promptly, is osteomyelitis of the jaw bone. To prevent its occurrence, you should immediately consult a doctor as soon as you suspect some signs of alveolitis.
If you do not have the opportunity to see a dentist immediately, before visiting a doctor you should rinse your mouth with a warm (but not hot!) 3% solution of hydrogen peroxide or baking soda (half a teaspoon of soda per glass of boiled water).
Medicines
After thoroughly treating the hole, the doctor usually prescribes special medications to the patient for the treatment of alveolitis. In addition to antibiotics and painkillers, antiseptic solutions for oral baths and mouth rinses are necessarily prescribed, because maintaining the cleanliness of the mouth and socket is an indispensable condition for successful treatment.
The following drugs are most effective:
- Hexicon . A modern antiseptic drug that is successfully used in dentistry. Particularly effective for stomatitis, gingivitis, periodontitis, alveolitis. Intended for topical use. Hexicon solution is used both in the form of applications and in the form of oral baths or for rinsing the mouth.
- Corsodil . The active substance of the drug is chlorhexidine. This is an effective antiseptic that has a bactericidal effect. Used in dentistry to disinfect the oral cavity. Used externally, as a solution for rinsing, irrigation and applications. After cleaning the socket of an extracted tooth, systematically rinsing the mouth with Corsodil solution has a good effect.
- Stomatidin . An effective antiseptic with antifungal and antibacterial spectrum, which is used not only in dentistry, but also in ENT practice. It prevents the development of infections and is indicated for stomatitis, gingivitis, alveolitis, periodontal disease, tonsillitis and pharyngitis. It is used both for rinsing the mouth and for applications.
- Chlorhexidine . A proven broad-spectrum antiseptic drug that is used for disinfection not only in dentistry. Effective for treating purulent wounds, in the treatment of diseases of the oral mucosa. It is an excellent preventative against most dental diseases.
- Eludril . Created on the basis of chlorhexidine. It has analgesic, anti-inflammatory and antiseptic effects. Indicated for stomatitis, gingivitis, alveolitis, periodontitis, as well as for treating the oral cavity before and after tooth extraction.
Prevention
The best prevention is the patient's strict compliance with all doctor's instructions. After tooth extraction, you should not rinse your mouth too aggressively to avoid damaging the blood clot. After all, its presence in the socket is a guarantee that pathogenic bacteria that provoke inflammation of the socket or alveolitis will not get into the wound.
When white plaque on a wound after tooth extraction requires examination by a doctor
Despite the fact that white plaque after wisdom tooth removal is a natural reaction, the patient needs to conduct a daily self-examination of the oral cavity and consult a doctor for help if alarming symptoms appear.
You should consult a doctor if:
➢
on the 3rd - 4th day the pain does not decrease, it becomes throbbing and intense;
➢
a white, reddish or yellow mass or liquid is released from the wound;
➢
swelling of the gums has intensified or spread to the face;
➢
body temperature rose above 38 degrees.
These signs indicate possible infection or complications. After examining the oral cavity, the dentist, if necessary, may prescribe a course of antibiotics or surgical cleaning of the socket cavity.
Preparing for tooth extraction
To avoid complications after dental procedures, simple preparation for tooth extraction is recommended.
- Do not delay going to the dentist: an inflammatory process quickly develops in the gum tissue, which stimulates increased blood supply to the sore spot, which is undesirable for surgery.
- Tooth extraction is not recommended for women during their menstrual period. On critical days, blood clotting is reduced, which leads to additional blood loss.
- It is better to contact the surgeon in the first half of the day, so that if unforeseen circumstances arise, you do not have to look for 24-hour dentistry.
- If an adult patient is going to the dentist, and the manipulation does not involve general anesthesia, then you need to eat first. The operation implies a mandatory reduction in the level of glucose in the body, which is already low in a hungry person. Lack of glucose causes a decrease in the rate of blood clotting, and after eating, the reverse process occurs.
- If general anesthesia is likely, contact your doctor in advance for an examination and consultation with an anesthesiologist. During general anesthesia, you cannot eat too much; the last meal should be taken no later than four hours before the operation. If this rule is not followed, the patient may vomit during anesthesia, and the vomit will enter the respiratory system, which will greatly complicate the work of doctors.
- Be sure to tell your dentist if you are allergic to certain medications.
- If you have heart disease, tell your doctor; this point is especially important if you are taking blood thinners. It is better to discuss this issue in advance with a cardiologist; sometimes taking medications that reduce blood clotting is temporarily discontinued.
The rules are simple, but this does not mean that you can ignore them. Tooth extraction is also an operation that sometimes leads to serious complications, especially if the patient and the surgeon are careless.
Gum healing
After tooth extraction, you need to be prepared for the fact that pain and swelling may intensify on the second day after surgery. But already on the 3rd - 4th day after the operation, the discomfort will begin to decrease. By this time, the wound healing processes are more active, and by touching the tip of the tongue to the hole, you can feel that a compaction has formed.
During this period, the following are actively developing:
- bone formation in the area of the removed tooth root;
- narrowing of the socket due to the “growth” of the gums;
- formation of the mucous membrane in the socket area.
Fibrinous plaque after tooth extraction persists for a week. It disappears on its own, without mechanical cleaning. Little by little, the mucous membrane begins to turn pink, gradually acquiring a healthy, natural color. Around the 10th day, wound healing is completed: healthy tissue is formed that covers the mouth of the hole. A small depression remains in the area of the removed tooth. The formation of bone tissue at the site of tooth extraction takes much longer - up to 6 months. Changes will be visible on an x-ray.
Why does alveolitis begin?
A slight inflammation in the socket is an inevitable process, since during tooth extraction tissue is injured and an open wound appears, and the environment in the mouth is unsterile. But alveolitis does not occur in everyone. So why does an infection get into the hole that the human body cannot cope with on its own?
Causes of infectious inflammation in the socket
The natural protective barrier is destroyed
A blood clot forms at the site of the extracted tooth; it closes the wound and protects it from infection. If this natural barrier is destroyed, for example by rinsing the mouth after tooth extraction, then the infection can penetrate into the tissue of the hole and provoke inflammation.
Poor oral hygiene
Bacteria live in the oral cavity. During the doctor’s manipulations, as well as after them, particles of tartar or soft plaque can get into the wound. This is a very good environment for bacteria, so they multiply quickly. Severe inflammation begins.
Poor sterilization of surgical instruments
Paradoxically, an infection in the socket can also be caused by a dental surgeon who uses poorly sterilized instruments.
Violation of the rules for processing the tooth socket
After surgery, especially if the extracted tooth had a granuloma, the doctor must carefully treat the wound so that it fills with blood to form a clot, and apply sterile cotton wool. Neglecting these rules can provoke alveolitis.
Violation of doctor's recommendations after removal
Even if you did not make a mistake in choosing a dental surgeon and the removal went well, an infection can get into the wound. This happens if you violated the doctor’s recommendations for caring for the hole. For example, they disturbed the wound with a tongue or some object and introduced an infection into it.
Decreased immunity
The cause of alveolitis may be decreased immunity or exhaustion of the body. This happens after a serious illness.
Caries
If there are teeth in the oral cavity affected by caries, then there is always a possibility that after removal you will encounter alveolitis.
To avoid the occurrence of alveolitis after tooth extraction, choose a dental surgeon responsibly and follow all his recommendations. A good doctor will definitely advise you to undergo professional oral hygiene before removal. This will reduce the risk of infection getting into the socket.
Prevention of alveolitis
Successful prevention of alveolitis depends on:
- Doctor. Tooth extraction should be as gentle and atraumatic as possible. A prerequisite is the use of sterile instruments and postoperative monitoring of wound healing.
- A patient who, for a period of time (up to 10 days), must refrain from smoking, hot and spicy foods, touching the site of tooth extraction or any other impact on it (cleaning it with a napkin or a cotton swab) so as not to damage the formed blood clot that performs protective functions. functions.
Classification of alveolitis
There are acute and chronic alveolitis. It can be spicy:
- Serous. Occurs 2–3 days after tooth extraction. The patient reports continuous pain that worsens after eating. If you do not seek help, the inflammation progresses and suppuration occurs.
- Purulent-necrotic. It appears after another 3–4 days. The pain grows and radiates to the temple and ear. An increase in the submandibular lymph nodes is visible to the naked eye. It becomes difficult to open your mouth, it becomes painful and uncomfortable to eat. A medical examination of an inflamed alveolus causes severe discomfort in the patient. The specialist diagnoses the presence of a dirty gray coating inside it and significant swelling around it.
Lack of medical care is fraught with the evolution of acute alveolitis into one of the forms of chronic:
- Hypertrophic, in which the periodontium grows abnormally.
- Purulent. The symptoms disappear, but pus is discharged abundantly from the hole.
Treatment methods for alveolitis
Treatment of alveolitis is aimed at eliminating the source of infection, preventing complications and preserving the health of the remaining teeth in the row. To do this, mechanical cleansing of the hole is performed, washing out the remaining pus with a solution of furatsilin or hydrogen peroxide.
Applications with anti-inflammatory and analgesic substances help relieve socket pain. The lotions are applied for half an hour, then removed to prevent the growth of microbes in them. This procedure can be repeated several times. If the patient has concomitant diseases and a malfunction of the immune system, the dentist may prescribe a course of antibiotics.
With timely treatment of alveolitis, acute inflammation goes away within a few days, but minor residual pain can persist for another 2-3 weeks. If the symptoms of the disease do not disappear, this may be a sign of the development of limited osteomyelitis (inflammation of bone tissue).
Causes
Disruption or flushing out of a blood clot occurs when rinsing the mouth after tooth extraction. The opinion of patients that if you rinse with antiseptics, the wound will heal faster is wrong. They are much more likely to lead to a “dry socket” and problems with it than to speed up rehabilitation after tooth extraction. Only oral baths are acceptable.
In addition to improper rinsing, the causes of alveolitis consist of the following factors:
- Weak immunity;
- poor blood clotting;
- failure to comply with the surgeon's requirements after surgery;
- ingress of bone remains or particles of crumbled teeth into the wound;
- insufficient treatment of the hole (if pieces of the root, cystic tissue, areas of granulation remain).
You can quickly cope with the disease if you make a diagnosis at the earliest stages of development. That's why it's so important to pay attention to its signs.