Reasons for appearance
If a black dot has formed in the mouth on the cheek, this may be due to injury. It can occur in case of accidental biting of delicate tissue. A small hematoma remains at the site of injury, which resembles a black dot or lump. This is a normal bruise or bruise located inside the mouth. Damage can be caused in other ways, namely:
- when chewing a hard object;
- while eating;
- with bruxism.
Often, a blackhead inside the cheek occurs as a result of constant friction and pressure on the mucous membrane. The problem is quite relevant after installing braces. Sometimes the orthodontist violates the technology or does not tighten the structure well enough. When talking or chewing, it scratches the gums, leaving behind black bruises. In this case, you need to remove all the pads and repeat the procedure.
If a black dot regularly appears in your mouth on your cheek, your dentist should check the integrity of your teeth. A destroyed crown can scratch and injure the mucous membrane with its sharp edge. With the traumatic formation of dark hematomas, no special treatment is required. After eliminating the cause, they resolve on their own without a trace. If the injury is repeated, there may be an open wound that becomes infected with bacteria. Therefore, large hematomas inside the cheek must be treated with special ointments.
Mole on the inside of the cheek. Causes of blackheads in the mouth and associated symptoms
The tongue in the human body not only performs an important function, but is also considered a diagnostic point.
His external condition can tell the doctor a lot. You probably noticed that during the examination the therapist asks you to show your tongue. This is no coincidence, because from it he can read not only information about microflora disorders, but also detect malfunctions in the gastrointestinal tract and genitourinary system, assess the state of the immune system and tell you about your food preferences. Any kind of neoplasm is a reason to visit the clinic. What can blackheads mean and what causes their formation on the oral mucosa? If they are formed on the tongue or the inside of the cheek, then this may indicate banal biting while chewing food. Sometimes this is a symptom of a serious illness that requires immediate specialist intervention. Normally, the dark spot after biting disappears after a few days. When this does not happen, and it begins to increase in size, or new spots have formed around it, then you should not delay a visit to the dentist. After examining the oral cavity, he will determine the nature of the neoplasm and, if necessary, recommend a consultation with a therapist, gastroenterologist or oncologist. Often, the stimulating factor for the formation of black spots on the surface of the tongue or on the cheek can be an allergic reaction to the dental material that the doctor uses during treatment.
Infectious diseases of the oral cavity
Stomatitis is an infectious disease, and most often the provoking factor for its development is non-compliance with hygiene rules and improper dental care. In some cases, the disease can cause sore throat or disruption of the gastrointestinal tract. In medicine, there are two main types of disease: acute herpetic and aphthous stomatitis. As a rule, the disease disappears without the intervention of specialists, but in some cases its course is quite severe. Aphthous stomatitis is cured after 1-2 weeks, leaving no scars on the mucous membrane. Infectious diseases of the oral cavity are considered:
- Gingivitis is an inflammatory process of the gums caused by changes in the blood formula, vitamin deficiency or diabetes mellitus. The provoking factor for gingitis is the use of oral contraceptives. Redness of the gums, bleeding and inflammation of the periodontal pockets are observed.
- Periodontitis is the main cause of tooth loss in older people. Such an infectious disease may be associated with diabetes mellitus, vitamin deficiency, changes in the blood formula and the use of oral contraceptives. There is painful swelling of the gums, loosening of healthy teeth, fever and chills.
- Vincent's ulcerative stomatitis is the formation of ulcers or erosions in the gum area. The impetus for its development can be a stressful condition, an unbalanced diet and bad habits, in particular smoking. The disease manifests itself as bleeding ulcers. The patient experiences difficulty breathing, submandibular lymph nodes become enlarged, body temperature rises, and the process of swallowing becomes difficult.
- Glossitis is caused by a streptococcal infection. Its development is stimulated by injuries or irritation of the tongue as a result of a poorly fitting prosthesis, abuse of alcoholic beverages and tobacco products, sharp tooth edges, biting, as well as a lack of vitamin B in the body, and skin diseases.
Signs and symptoms
The reasons for the appearance of a black dot in the mouth on the cheek can be different. What they all have in common is that they eventually form a hematoma filled with bloody contents.
When an infection occurs, additional symptoms may occur such as:
- general malaise;
- temperature increase;
- weakness;
- swelling;
- blistering;
- the appearance of ulcers at the site of the vesicles;
- itching or soreness;
- decreased appetite;
- bad breath.
Sometimes general malaise is accompanied by enlarged lymph nodes. If these symptoms appear, you should contact your dentist for diagnosis and treatment.
Black dots on the sky. Why do gums darken?
Dark spots can appear on any part of the gums. They can be large and small, point and extended.
Causes of black spots on gums:
- Smoking (most common cause).
- Carious tooth damage.
- Tartar.
- Gingivitis, periodontitis with bleeding.
- Inflammation of the oral mucosa (stomatitis).
- Physical trauma to the jaw, gums.
- Tooth filling with amalgam.
- Peutz-Jeghers syndrome.
- Addison's disease.
Peutz-Jeghers syndrome and Addison's disease are very rare diseases. Their presence in humans has been known since early childhood. One of the symptoms of pathologies is the appearance of black dots or spots on the palate, gums, tongue, and lips.
A disease such as stomatitis can appear for a number of reasons, including disruption of the functioning of internal organs. A specialist should understand the causes of darkening of the gums.
Smoking and dark gums
The constant effect of nicotine and tar has a detrimental effect on the entire body, and especially on the oral cavity. Almost all smokers have the following symptoms:
- black spots on the gums;
- change in the shade of tooth enamel (change to yellow or gray);
- unpleasant odor from the mouth;
- bitter taste in the mouth.
To get rid of dark spots on your gums, you need to stop smoking, preferably forever. Breaking a bad habit is always difficult. Today you can quit smoking with the help of special patches and sprays.
Smoker's gums are always dark and with various diseases
When the cause of the violation has been eliminated, you can begin to remove black spots. Typically, gums are treated with laser correction. Small areas of darkening can be removed using folk remedies.
If you remove dark spots without eliminating the cause (without quitting smoking), you will not be able to achieve a reliable result. Over time, the blackening will reappear.
Stomatitis as a cause of gum blackening
Stomatitis is an inflammation of the oral mucosa. The occurrence of stomatitis is associated with the reaction of the immune system to unidentified molecules. The cause of inflammation can be:
- Gastritis (inflammation of the stomach).
- Duodenitis (inflammation of the duodenum).
- Colitis (inflammation of the colon).
- Worm infestation.
- Ulcers and redness of the mucous membrane appear when the rules of oral hygiene are not observed.
Ulcers and spots on the mucous membrane due to stomatitis are whitish or yellowish in color. But if there is bleeding or deep inflammation, they can turn brown or black. Stomatitis is treated with local remedies. No additional measures are needed to remove dark spots.
Gum fungus causes gums to turn black
Tooth decay and dark gums
Every inhabitant of planet Earth is familiar with caries. This is a sluggish destruction of hard tooth tissues, which is caused by unfavorable external and internal factors.
Caries demineralizes the enamel, gradually forming a hole in the dentin. If the disease is not cured in a timely manner, the pathological process will reach the pulp and periodontium. This is a dangerous condition that threatens tooth loss. Caries can also occur hidden. Destruction occurs deep in the tooth; changes are difficult to notice externally.
Advanced caries affects the condition of the gums. It turns black at the base of the tooth and a slight swelling may appear.
Necrosis of the tooth and its root in the gum - black spot
Trauma to the jaws and gums
A black spot on the gum may turn out to be a hematoma, a consequence of strong physical action:
- blow to the face, jaw;
- knocked out tooth;
- excessive pressure on the gums from orthopedic structures, too hard food;
- tooth extraction with complications.
Physical trauma leads to rupture of small vessels, blood flows into the tissue space. A purple or black bruise or sometimes a lump forms on the gum. Gradually the released hemoglobin decomposes, the stain changes color to brown and yellowish. A person should be aware of the injury, in order to avoid undesirable consequences, one should seek advice from a specialist.
Gum cyst after filling - dark spot
The consequences of serious gum trauma can be infection, inflammation and even tissue necrosis. Therefore, the problem cannot be started.
Stains from amalgam fillings
Amalgam is an alloy of silver and mercury, used as a filling material. Today, amalgam is used very rarely for tooth filling; more advanced materials have been developed.
If a tooth has been filled with amalgam, the gums around it may darken. With prolonged contact with the mucous membrane, the material stains it. The intensity and size of the dark spot depends on the characteristics of the tooth treatment. Hot drinks and food increase darkening.
Amalgam stains should not be a concern; they are only an aesthetic concern. If they appear, you need to seek dental help.
Carrying out treatment
If you bite your cheek and an ulcer forms, only a dentist can determine how to treat it after an examination. If a blood clot interferes, then such a bladder can be punctured. The doctor also prescribes rinsing with antiseptics, in particular, such as Furacilin or Chlorhexidine. You can also perform oral baths with decoctions of chamomile herbs or oak bark. These solutions help eliminate signs of inflammation.
In addition, wounds in the mouth appear due to weak blood vessels. To strengthen their walls, you can use vitamin A, C, E, K, and B vitamins. You can also stimulate and maintain immunity. To do this, it is recommended to take multivitamin preparations that contain all the required substances.
When you bite your cheek from the inside, what to treat will be determined by the doctor after diagnosis, since there is no universal method. It all depends on the identified disease. During therapy, it is important to eliminate the provoking factor.
For aphthous ulcers, the use of anti-inflammatory gels and mouth rinsing with Chlorphyllipt and Cholisal is indicated. The doctor prescribes antiviral, healing drugs and antiseptics for topical use. Acute disease requires the use of antibiotics.
Treatment of pemphigus involves the use of hormonal corticosteroids. In this case, therapy is carried out in a hospital setting. When new rashes appear, maintenance dosages of drugs are prescribed. For a speedy recovery, you need to rinse your mouth with Miramistin, as well as use pain-relieving gels and ointments. To normalize the functioning of the immune system, multivitamin complexes are prescribed.
Treatment of a hematoma on the buccal mucosa must be carried out under the supervision of a doctor. Self-medication is not recommended, as this can only worsen the problem.
Benign neoplasms of the oral cavity
“Something” that appears in the mouth does not grow, does not appear in a new place and, in principle, does not hurt. This means that the tumor is benign in nature. They, in turn, are divided into several subspecies.
Epithelial growths: papillomas, nevi, Serre glands. Papilloma is a small protrusion with “papillary” growths; when left in the mouth for a long time, it becomes rough and whitish. A nevus that varies in color, ranging from pale pink to brown. If you notice a yellowish semicircle above the upper or lower gums, it is most likely a Serra gland.
There are many more types of connective tissue tumors. Fibroids of identical color form on the lower lip, tongue or palate. After inflammation of the gums, compactions can form - fibromatosis. Lumps on the muscle tissue on the underside of the tongue and underneath it are called fibroids.
In addition to connective tumors, neoplasms of the oral mucosa are vascular. More often they develop in children and appear after diseases of the nasopharynx.
Mouth rinses
Proper oral hygiene includes the use of mouth rinses. If a person follows all the rules, then he visits the dentist, only for preventive purposes. There are many different rinses, so it is important to choose the right product correctly. According to reviews and recommendations from dentists, the most popular products are:
- "Listerine";
- "Splat";
- "Lakalut";
- "Asepta";
- "Paradontax";
- Colgate.
Listerine mouthwash is very popular. The price and instructions for this product are affordable, so everyone can easily use it. The mouthwash contains anti-inflammatory substances. It is used for periodontitis, helps eliminate gum disease and bad breath.
It has a reasonable price. The instructions for the Listerine mouthwash say that it protects the mucous membranes and teeth, is easy to use, and also creates a slight whitening effect. The disadvantages include a not very pleasant sharp aftertaste, as well as a burning sensation in the mouth.
The well-known antibacterial agent “Splat” has a whitening effect, has an anti-inflammatory and hemostatic effect. It prevents the formation of stone and plaque, and therefore prevents the development of periodontitis. Does not contain alcohol or fluoride.
Mouthwash can be used to prevent many diseases. It has a pleasant aroma and is also affordable. The disadvantages include a specific taste and high concentration.
Elmex mouthwash does not contain antiseptics or alcohol and is used to protect enamel. It can be used daily. Approved for use by children over 6 years of age. It freshens breath well and cleanses the oral cavity. The disadvantages include the high cost of the product.
The Italian drug President is made on the basis of medicinal herbs. It does not contain alcohol and has anti-inflammatory and antibacterial effects. This product reduces the risk of tartar formation and reduces enamel sensitivity. It has a pleasant aroma and taste, but its cost is quite high.
The unique formula of Colgate Total Pro mouth rinse helps combat harmful bacteria in the mouth, helps reduce bleeding and inflammation of the gums, and also freshens breath. It has a pleasant taste and is suitable for daily use.
Lacalut Active mouthwash has an astringent effect and is used for bleeding gums. This product protects teeth well. Used in courses of 21 days. Does not contain alcohol. It has a pleasant taste and aroma.
The drug "Asepta" contains two antiseptic substances, thanks to which it has an analgesic and antibacterial effect. Used for gum inflammation. The course of therapy is no more than 2 weeks. Otherwise, dysbiosis may develop.
According to the instructions for use, chlorhexidine digluconate 0.05% is used to combat pathogenic microorganisms of the oral cavity. That is why it is widely used in dentistry. The drug has no age restrictions, but for children 3 years old, special care must be taken when using it.
You can also use chamomile as a mouth rinse. This is a natural remedy that has a pronounced anti-inflammatory effect and has virtually no contraindications.
Mole in the mouth on the cheek.
Part 1
Examining your mouth for signs of cancer
- 1
Look for sores and inflammation on the lips, tongue, cheeks and lower mouth. Mouth sores are common and are not a sure sign of cancer. Although, when oral ulcers are combined with other symptoms and their development occurs in a certain part, this may indicate the presence of cancer.
- Look for mouth ulcers that take more than two or three weeks to heal.
- Look for mouth sores that appear in the same place over and over again.
- Look for mouth sores that have jagged borders and bleed when touched lightly.
2
Check for oral discoloration or spots in the mouth. Watch for discoloration on the surface/sides of the tongue, lips, inner cheeks that does not go away for more than two weeks.
- This color can be red, white, gray or dark.
- You may also notice velvety white and red patches in your mouth.
3
Check for numbness or pain in different parts of the mouth. You may experience numbness in parts of your mouth, face, and neck as a symptom of cancer.
- You may also experience persistent pain/sensitivity in a certain part of your mouth.
- If you experience any of these two symptoms with or without a lump/swelling, visit your doctor immediately.
4
Look for rough, crusty patches around the mouth and lips. These crusty patches may be hard to the touch, have irregular borders, and bleed for no reason.
5
Examine your teeth to see changes in their alignment. Examine your teeth carefully to see changes in their alignment. Also, if teeth are loose, this may also indicate oral cancer.
- If the position of the teeth has changed, then a good way is to wear dentures (if you use them). Difficulty in fitting dentures is a good sign that your teeth have shifted.
What is it used for?
Quite a lot of discomfort comes from biting your cheek from the inside. Many people who face this problem are interested in how to treat it. To prevent the development of an infectious process, rinses are used. In addition, they are indicated for comprehensive oral care and for:
- fight bacteria;
- preventing the formation of tartar;
- protection against caries;
- strengthening tooth enamel;
- eliminate bleeding gums.
Even with the most thorough brushing, it is impossible to completely eliminate all bacteria because most people do not pay the required attention to cleaning the inside of their cheeks and tongue. It is on the mucous membrane that a significant part of the bacteria accumulates. The use of rinses helps reduce the number of bacteria, as well as reduce the likelihood of their growth and reproduction. Pathogenic microorganisms provoke the appearance of bad breath and also contribute to the development of dental diseases.
Tartar is a hard formation on the enamel. You can get rid of them only with professional teeth cleaning. To prevent this problem, you need to use a rinse aid that slows down the plaque formation process. It also reduces the acidity of the oral cavity and reduces the risk of caries to a minimum.
The composition of the rinses includes fluoride, which has a mineralizing effect on the enamel. This product also reduces tooth sensitivity, as it normalizes the level of acidity and reduces the effect of irritants on the enamel. The active components that make up the product destroy pathogenic microorganisms.
Adenoid cystic carcinoma of the buccal mucosa
Adenoid cystic carcinoma (AC) is a malignant neoplasm of the salivary glands. The pathology was first described as Billroth cylindroma in 1856. The term adenoid cystic carcinoma was established in 1928 and is still used today. Adenoid cystic carcinomas account for less than 1% of all malignant tumors of the head and neck, and 50% of AKs arise in the oral cavity, mainly on the hard palate. Other slightly less common sites include the lower lip, retromolar/tonsillar region, sublingual gland, buccal mucosa, and floor of the mouth. Adenoid cystic carcinoma is clinically characterized by small size and slow growth. However, AKs spread invasively into surrounding tissues and form distant metastases. Pain is an important symptom for determining perineural extension. Thus, AKs have a long clinical course and a questionable prognosis, and the prognosis is somewhat worse when the minor salivary glands are affected than the large ones. We provide a description of the features of adenoid cystic carcinoma of the buccal mucosa in parallel with a review of the available literature.
Clinical case
A 45-year-old woman came to the clinic with complaints of a painful swelling on the mucous membrane of the left cheek. The formation was first noticed 3 months ago, after which it gradually increased in size. The appearance of the pathology was accompanied by pain, unexpressed and prolonged. An intraoral examination revealed a swelling with unclear boundaries on the mucous membrane of the left cheek in the area of the molars (photo 1). Palpation revealed a soft, well-defined, mobile swelling measuring 1x1 cm. The mucous covering the formation was not changed.
Figure 1: Intraoral photograph showing swelling in the left posterior buccal mucosa (black stripe).
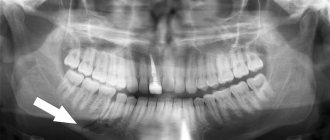
OPG did not reveal any violations of the bone structure of the upper and lower jaws (photo 2). Ultrasound showed a hypoechoic mass with a homogeneous internal structure and defined edges. No calcification zones were found, the formation is not fused with the surrounding structures (photo 3). These features indicated well-defined, benign tissue masses. The formation was surgically excised. Histopathological examination revealed a violation of cellular architecture and a lattice structure of tumor cells with many small cystic cavities. Perineural invasion was detected (Figure 4). Based on the above symptoms, a diagnosis of adenoid cystic carcinoma was made. Since the edges of the wound were not affected, it was decided not to use auxiliary therapy. The patient remained under observation for 3 years without signs of relapse.
Photo 2: OPG without bone tissue pathology
Figure 3: Ultrasound image showing a clearly visible hypoechoic mass with a homogeneous structure (lesion marked with x)
Photo 4: X10 micrograph showing the lattice structure of tumor cells
Discussion
Adenoid cystic carcinoma is a rare epithelial tumor that is characterized by painlessness and constant growth. WHO defines adenocarcinoma as a basaloid tumor containing epithelial and myoepithelial cells in various morphological configurations, including tubular, cribriform and solid structures. This disease has a more severe clinical course and is usually fatal.
AK usually occurs in the 4th-6th decade of life with a predominance of women in the ratio of 3:2. In our clinical case, a 45-year-old woman suffered from the disease. Among all salivary gland neoplasms, 9–23% arise intraorally, 50% of which are malignant.
Most articles in the literature describe cases of adenocarcinomas of both minor and major salivary glands. However, there is practically no mention of damage to the buccal mucosa alone. This article is the first in this aspect of all 41 published works. After the overall analysis, 2280 cases of adenoid cystic carcinoma were found in 41 articles. Of this number, 1382 describe intraoral localization and 178 involve the oral mucosa. Based on the data presented, we can conclude that among the minor salivary glands, the buccal mucosa is affected in 12.9%. The overall percentage of adenoid cystic carcinoma in the cheek area is 7.8%. According to a review of all articles, 60.6% of all adenocarcinomas occur in the oral cavity.
The clinical manifestation of the tumor is slow growth and the formation of a dense mass. Pain is a common and important symptom, sometimes appearing before clinical manifestation. The pain syndrome is usually dull and prolonged. The described case presents a slowly growing painful swelling. Local lymph nodes are rarely involved. Hematogenous spread occurs in late stages of the disease. Distant metastasis usually occurs to the lungs, bones and soft tissues.
Histologically, adenoid cystic carcinoma occurs in three types: cribriform, tubular and solid. The tubular form is the most favorable, and the solid form is the most malignant. AKs are divided according to their histological nature into levels: I, II, III. Level I: combination of cribriform and tubular, level II: combination of cribriform, tubular and solid and level III: solid type only. The reported clinical case was of the cribriform type and classified as level I. The tendency for perineural spread is quite typical for AK. Common pain syndrome may to some extent be associated with this factor. However, it cannot be considered pathognomic. Such distribution cannot be considered prognostically significant, while some authors indicate that this parameter may be a sign of distant metastasis.
Various treatment options for AK have been proposed, including surgery, radiotherapy, chemotherapy and combination therapy. Surgical wide excision is the treatment of choice. In this case, this particular method was used. The prognosis of the disease can be influenced by a variety of factors. Tumor stage, excision margin, location, perineural invasion, solid histologic type, and presence of cervical lymph node metastases are also taken into account. AK usually has a long clinical course with the formation of distant metastases in the later stages of the disease. According to one study, the average time between diagnosis of the primary lesion and detection of distant metastases is 60 months, ranging from 18 to 120 months. Unlike other malignant tumors, adenocarcinomas usually do not lead to death in the short term, but at the same time have low long-term survival.
Conclusion
Adenoid cystic carcinomas are seemingly harmless lesions that are characterized by very slow growth. However, due to the tendency for perineural spread and distant metastasis, this pathology requires careful and long-term observation.
Authors: Vidya Ajila , Department of Dentistry and Radiology, AB Shetty Memorial Institute of Dental Sciences, Nitte University, Deralakatte, Mangalore Shruthi Hegde , Department of Dentistry and Radiology, AB Shetty Memorial Institute of Dental Sciences, Nitte University, Deralakatte, Mangalore Gopakumar R Nair , MAHE Institute of Dental Sciences and Hospital, Chalakkara, Pallor, Mahe, India Subhas G Babu , Department of Dentistry and Radiology, AB Shetty Memorial Institute of Dental Sciences, Nitte University, Deralakatte, Mangalore
How to choose the right one
Each type of mouthwash is designed to solve a specific problem, as it contains a specific set of active ingredients. When choosing a remedy, you need to focus on the existing problem. If you bite your cheek, then the following types of drugs are suitable:
- elixirs for gums;
- antifungal agents;
- dry;
- against caries.
Elixirs have an anti-inflammatory effect and improve the microflora of the oral cavity. In addition, they eliminate swelling, increase blood circulation, and heal wounds. These products should be used before brushing your teeth.
Antifungals contain iodine. They are indicated for people with thyroid diseases. This product is rubbed into the gums up to 4 times daily. Dry ones are used for purulent inflammations. They are produced in powder form. They need to be diluted with water before use. Not suitable for daily use.
For regular use, it is better to buy products made from plant extracts. You need to pay attention to the composition of the product. If it contains ethyl alcohol, then it should not be used by drivers and children.
Anti-inflammatory ointments and mouth gels
If you have bitten your cheek and an ulcer has formed, many people are interested in how to treat it, since it causes significant discomfort. Treatment in this case should be timely and comprehensive. An integral part are dental gels that help eliminate inflammation and pain. They can be used on the recommendation of the treating doctor after examination.
Before deciding on the choice of medicine, you need to study the chemical composition so as not to harm the oral mucosa and human health. Such drugs as “Solcoseryl”, “Cholisal”, “Apident Active” have an analgesic effect.
The drug "Cholisal" helps eliminate swelling, suppresses pain and eliminates increased bleeding of the gums. The medicine must be injected into the gum pockets and after that do not eat for 30-40 minutes. The course of treatment is 10-14 days.
The drug "Solcoseryl" accelerates the restoration of damaged tissues. After the first use, inflammation goes away, the gums are restored, and an acute attack of pain is eliminated.
The drug "Apident Active" is made on the basis of propolis. Active components eliminate pain and inflammation. Anti-inflammatory drugs include Kamistad, Metrogyl Denta, Asepta.
When purchasing the drug, you need to study the instructions for use and reviews of Metrogyl Dent. The price of the product is affordable, and the result is noticeable almost immediately after use. This is a combination product made in the form of a gel. It contains an antibiotic and an antiseptic. This combination helps to quickly get rid of pathogenic microflora.
The drug "Kamistad" is a gel that contains components of plant origin. It helps quickly eliminate inflammation and provides pain relief.
How it works
Gels and ointments are an auxiliary means of antibacterial therapy. They have an anti-inflammatory and restorative effect, accelerating the healing process.
Such products are highly effective, are tightly fixed to the gums and do not have an unpleasant odor, providing fairly good access of the active components to hard tissues. They contain an antiseptic and an antibiotic. The result of its use is noticeable after the first procedure.
How to use correctly
Before using the gel, you need to consult a doctor and study the instructions for the drug. It is intended only as applications and compresses. It is recommended to carry out procedures between meals and at the same time reduce salivation. In order for the action to be purposeful and soft, you need to follow the following rules:
- check for allergies to the components of the product;
- apply the product in a thin layer;
- do not consume food or drinks for 30 minutes;
- the number of sessions per day is 4-5;
- It is forbidden to exceed the daily dosage.
If irritation and itching occurs in the oral cavity, you should immediately change the medication.
Black dot on the inside of the cheek. Black spot in the mouth on the cheek, like a mole
- Look for sores and inflammation on the lips, tongue, cheeks and lower mouth. Mouth sores are common and are not a sure sign of cancer. Although, when oral ulcers are combined with other symptoms and their development occurs in a certain part, this may indicate the presence of cancer.
- Look for mouth ulcers that take more than two or three weeks to heal.
- Look for mouth sores that appear in the same place over and over again.
- Look for mouth sores that have jagged borders and bleed when touched lightly.
- Check for oral discoloration or spots in the mouth. Watch for discoloration on the surface/sides of the tongue, lips, inner cheeks that does not go away for more than two weeks.
- This color can be red, white, gray or dark.
- You may also notice velvety white and red patches in your mouth.
- Check for numbness or pain in different parts of the mouth. You may experience numbness in parts of your mouth, face, and neck as a symptom of cancer.
- You may also experience persistent pain/sensitivity in a certain part of your mouth.
- If you experience any of these two symptoms with or without a lump/swelling, visit your doctor immediately.
- Look for rough, crusty patches around the mouth and lips. These crusty patches may be hard to the touch, have irregular borders, and bleed for no reason.
- Examine your teeth to see changes in their alignment. Examine your teeth carefully to see changes in their alignment. Also, if teeth are loose, this may also indicate oral cancer.
- If the position of the teeth has changed, then a good way is to wear dentures (if you use them). Difficulty in fitting dentures is a good sign that your teeth have shifted.
- Feel for bumps or swelling on the side of your face and neck. Look for abnormal bumps, swelling, or bulges on the side of the face or neck. Apply gentle pressure to the neck to detect any pain, tenderness or lumps. Visually inspect the skin for abnormal growths or birthmarks. Pull back your lower lip with your thumb and index finger and check for lumps or uneven growths. Do the same with the upper lip. Place your index finger on the inside of your cheek and your thumb on the outside, then check for pain, changes in texture, swelling, or bumps on your cheeks by gently rolling and pressing your fingers into the skin.