Anatomy
The fibers emerging from the nucleus first go dorsally to the bottom of the IV ventricle, without reaching it, bend around the nucleus of the abducens nerve, forming the internal knee of the facial nerve, then stretch in the ventral direction until they exit the pons at its posterior edge above and laterally from the olive medulla oblongata. Here in the so-called At the cerebellopontine angle, the facial nerve is located medial to the vestibulocochlear nerve in the form of a more powerful root of the facial nerve itself and a thin root of the intermediate nerve (n. intermedius). Then, together with the vestibulocochlear nerve, it enters the internal auditory foramen of the temporal bone. Here L. n. together with the intermediate nerve it enters the L. n. canal, which is embedded in the pyramid of the temporal bone. In this canal, the facial nerve runs forward and to the side, then bends posteriorly at almost a right angle, forming the external genu. Then it goes first in a lateral direction back, and then down and exits the skull through the stylomastoid foramen (foramen stylomastoideum). In the canal, the stapedius nerve (n. stapedius) departs from it, going into the tympanic cavity to the muscle of the same name. After leaving the skull, the posterior auricular nerve (n. auricularis post.), innervating the muscles of the auricle and the occipital muscle, and the digastric branch (r. digastricus), going to the posterior belly of the digastric muscle and to the stylohyoid muscle, are separated from the facial nerve. Having given these branches, L. n. penetrates the parotid gland, passes through it and forms a plexus (plexus parotideus) in front of the external auditory canal, from which branches extend to the facial muscles. The largest branches of L. and. on the face - temporal (rr. temporales), zygomatic (rr. zygomatici), buccal (rr. buccales), marginal branch of the lower jaw (r. marginalis mandibulae), cervical branch of the L. n. (r. colli), innervating the subcutaneous muscle of the neck (platysma).
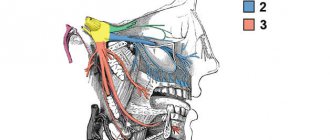
Rice. 1. Schematic representation of the topography of the fibers of the facial nerve: 1 - greater petrosal nerve: 2 - genu ganglion; 3 - stapedius nerve; 4 — tympanic string (connecting branch with the tympanic plexus); 5 - temporal branches; 6 - zygomatic branches; 7 - buccal branches; 8 - marginal branch of the lower jaw; 9 - cervical branch; 10 - parotid plexus; 11 - stylohyoid branch; 12 - digastric branch; 13 - stylomastoid foramen; 14 - posterior auricular nerve.
The bulk of the facial nerve consists of motor fibers. The intermediate nerve is directly connected to it, which anatomically represents a part of the L. n. The intermediate nerve is mixed, it contains sensory (gustatory) and parasympathetic (secretory) fibers. At the outer knee of the L. n. in the facial canal, the sensitive part of the intermediate nerve forms the nerve ganglion (gangl, geniculi). The peripheral processes of the pseudounipolar cells of this nerve ganglion are part of the chorda tympani (chorda tympani), the edges extend from the L. n. in the canal and through the canaliculus of the chorda tympanum it penetrates into the tympanic cavity, where it lies on its lateral wall and leaves it through the petrotympanic fissure (fissura petrotympanica). From here, the tympanic string goes down and joins the lingual nerve (n. lingualis), providing taste innervation to the anterior 2/3 of the tongue. The central processes of the nerve ganglion cells as part of the intermediate nerve are directed to the nucleus of the solitary tract (nucleus tractus solitarii) in the brain stem. The chorda tympani also carries secretory fibers to the sublingual and submandibular salivary glands. These fibers begin in the superior salivary nucleus, located in the pons dorsomedial to the nucleus of the left n. In the channel from L. n. The great petrosal nerve also departs (p. petrosus major), which exits the pyramid of the temporal bone through the cleft of the canal of the great petrosal nerve (hiatus canalis n. petrosi majoris) and from the cranial cavity through the lacerated foramen. It passes through the pterygoid canal (canalis pterygoideus) into the pterygopalatine fossa to the node of the same name, where the parasympathetic fibers switch to the postganglionic neuron. Postganglionic fibers are directed to the lacrimal gland and the glands of the mucous membrane of the oral and nasal cavities as part of the branches of the trigeminal nerve (Fig. 1).
Core of L. n. (nucleus n. facialis) is represented by cells located in the tegmentum of the bridge near the nucleus of the abducens nerve (n. abducens). The cells that have split off from the main nucleus are located dorsally from it and are united under the name of the accessory nucleus (nuci, accessorius n. facialis). Core of L. n. in the process of phylogenesis it moves: in lower vertebrates it lies dorsally, and in higher ones it shifts ventrally. Cortical center of L. n. located in the lower quarter of the precentral gyrus. The cell groups for the frontal branches lie higher than the cell groups for the oral branches. The axons of the cells of the cortical center of innervation of facial muscles are located in the knee of the internal capsule, being part of the corticonuclear tract (tractus corticonuclearis). Partially not reaching the nuclei of L. n. in the bridge, partly already at their level, the corticonuclear fibers intersect at the suture of the bridge and approach the cells of the nucleus of the L. n. the opposite side. Some of the uncrossed fibers end in the core of their side. Spine L. n. is formed from the axial processes of the cells of the nucleus of its side; a very small part of the fibers enters it from the nucleus of the opposite side. Through L.n. Most facial reflexes are realized both from the mucous membranes and from the skin - sucking, blinking, corneal, conjunctival, sneezing, nasolabial, etc.
Electromyography of the facial and trigeminal nerve
Electromyography of the facial nerve helps determine the cause of weakness or increased excitability of the masticatory and facial muscles. Electromyography of the trigeminal nerve is necessary to establish the cause of pain, disturbances in facial sensitivity and function of the masticatory muscles. Neuroscientists record the electrical activity of facial muscles and the nerves that control these muscles using various types of electrodes.
When conducting electromyography of the facial and trigeminal nerve, neurophysiologists at the Yusupov Hospital conduct a study of the blink reflex. The trigeminal nerve primarily consists of sensory fibers. Through them, excitation is transmitted from sensitive receptors of the face to brain cells. The facial nerve consists of motor fibers. It sends commands from the brain to the facial muscles. In the brain, both nerves form a reflex arc: in response to an impulse from the trigeminal nerve system, the facial nerve sends an exciting signal to the facial muscles. This reflex arc is examined using electromyography.
The neurophysiologist places electrodes on certain points of the face to stimulate excitation in the trigeminal nerve system and record the response in the facial nerve system. It then administers a series of stimuli and records the responses to them. The information is subject to computer processing. A neurologist-neurophysiologist receives measurement results, draws up a conclusion and gives recommendations for treating the disease.
In order to undergo EMG of the facial and trigeminal nerve, masticatory muscles of the face, call the Yusupov Hospital. The contact center operates 24 hours a day, seven days a week, including lunch breaks. You will be scheduled for a consultation with a neurologist-neurophysiologist at a time convenient for you. The price of EMG of the facial and trigeminal nerves and facial muscles at the Yusupov Hospital is lower than in other Moscow clinics, despite the high quality of the research.
Pathology
Primary and secondary lesions of the facial nerve
Defeat of L. n. is caused by various reasons and is usually referred to as “neuritis”. There are primary, or idiopathic, and secondary, or symptomatic, neuritis.
The most common neuritis is L. n., called colds or Bell's disease. In etiology, its main role is played by cooling the body, especially the head. Acute development of the disease over several hours or one day is typical. Its pathogenesis is explained by the fact that cooling, which is an allergic factor, causes vascular disorders in the nerve trunk (spasm, ischemia, edema) that disrupt its nutrition and function (ischemic paralysis). The developmental anomaly is also important - the congenital narrowness of the L. n. canal.
Symptomatic neuritis is observed in various inf., toxic diseases, in inflammatory, tumor processes at the base of the brain, in the cerebellopontine angle, in brain stem encephalitis, poliomyelitis, vascular lesions of the brain stem, in fractures of the base of the skull, the pyramid of the temporal bone, in damage to the parotid gland, in acute and more often chronic otitis, during hypertensive crises, etc.
There are cases of congenital paralysis of the muscles innervated by the L. n. (Mobius syndrome), and also describes hereditary and family cases, apparently associated with a genetically determined anomaly of the L. and. channel.
Topical diagnosis of lesions of L. n. is based on its different structure at different levels, therefore, damage to the nerve proximal to the origin of a certain branch causes loss of the corresponding function, and with distal damage, the function is preserved. This is the basis for diagnosing the level of damage along the L. n. canal, where three branches depart from the nerve: the greater petrosal nerve, which supplies fibers to the lacrimal gland, the stapedius nerve, which innervates the stapedius muscle, and the chorda tympani, which provides taste innervation of the anterior 2/3 tongue . Determining the degree of nerve damage is based on identifying the complete or partial loss of its functions and the dynamics of the development of symptoms.
Disturbances in the motor function of the nerve, even with minor damage, can be determined visually by the asymmetry of the face; with complete damage to the nerve, a picture of peripheral paralysis develops: the face is mask-like, the corner of the mouth is lowered, the palpebral fissure is open, the eyebrow is lowered, motionless.
To determine the vegetative function of L. n. examine the functions of tear and salivation. Tear production is examined using the Schirmer test (ribbons of filter or litmus paper are inserted into the lower fornix of the conjunctiva of the eye of the subject, resulting in lacrimation; the intensity of tear production is determined by the length of the paper wetting in millimeters). Salivation is examined by radiometric determination of the concentration ability of the salivary glands and determination of the intensity of salivation by the amount of saliva received (while the subject is sucking a slice of lemon, saliva is collected separately from the pre-catheterized right and left parotid ducts for 1 minute). The study of taste sensitivity on the anterior 2/3 of the tongue is carried out using a chemical method. gustometry, in which the thresholds of the main taste sensations are determined - sweet, salty, sour and bitter by applying the appropriate solutions to the tongue, or electrogustometry, when the threshold values of the strength of the electric current are determined, causing a specific sensation of sour when it irritates the taste buds of the tongue (see Taste).
Rice. 2. A patient with symptoms of neuritis of the left facial nerve: 1 - facial asymmetry; 2 - smoothness of the nasolabial fold and increased asymmetry when teeth are bared; 3 - lagophthalmos, the eyeball is raised upward and retracted outwards (Bell's symptom); 4 - asymmetry of the frontal folds when raising the eyebrows.
The main symptoms of neuritis L. n. (Fig. 2) are caused by peripheral paresis, paralysis of the facial muscles of the upper and lower half of the face (prosopoplegia) on the side of the affected nerve. Already at rest, the mask-like appearance of the corresponding half of the face (the face of the sphinx) attracts attention - the eye is wide open, almost does not blink, the forehead is without wrinkles, the nasolabial fold is smoothed, the eyebrow and corner of the mouth are lowered. The patient cannot frown, raise his eyebrows, when closing his eyes the eyelids do not close completely, the palpebral fissure gapes (lagophthalmos), when trying to close the eye, the eyeball rises upward and deviates outward (Bell's phenomenon), while the sclera is not completely covered. When smiling or laughing, half of the face is motionless; when teeth are shown, the mouth deviates to the healthy side; when the cheeks are puffed out, the diseased side “sails.” While eating, food gets stuck between the cheek and teeth, saliva and liquid food are poorly retained in the mouth, the patient cannot spit or whistle. During the acute period, the patient clearly pronounces labial sounds (b, m). Due to the slight displacement of the mouth, the protruding tongue may deviate slightly in the healthy direction. Often, motor disturbances appear simultaneously with movement disorders, and sometimes they are preceded by usually mild and short-lived pain in the area of the mastoid process and the auricle. Other disorders may also be observed due to damage to the sweat-salivary and taste fibers of the nerve trunk, extending in the L. n. canal. at its different levels. When L. is affected and. in the canal above the origin of the greater petrosal nerve, in addition to paralysis of the facial muscles, there is a lack of lacrimation (dry eye), sweating (dry skin of half the face), unilateral loss of taste in the anterior 2/3 of the tongue, strong, unpleasant perception of ordinary sounds (hyperacusis). With damage below the origin of the petrosal nerve, increased lacrimation is observed, because due to the weakness of the lower eyelid, tears do not enter the lacrimal canal, but flow out; taste disorder and hyperacusis. With a lesion below the stapedial nerve, hyperacusis does not occur; with a lesion below the origin of the chorda tympani, the disorders noted above are absent, but lacrimation persists. When L. is affected. at the level of the geniculate node, Hunt's syndrome is observed - a combination of peripheral paralysis with herpetic rashes and excruciating pain in the area of the auricle, tympanum, back of the palate and the anterior half of the tongue (see Hunt's syndrome). Colds neuritis L. and. sometimes it can be bilateral (diplegia facialis).
An important diagnostic and prognostic value is the study of electrical excitability of the nerve, in which a partial or complete reaction of degeneration is detected, and complete is a prognostically unfavorable sign. An electromyographic study makes it possible to judge the speed of impulse conduction in the left leg. and its branches and the presence of nuclear destruction.
Peripheral muscle paralysis when L. is affected and. should be distinguished from central paralysis associated with damage to the supranuclear tracts, in which the electrical excitability of L. n. not qualitatively changed.
In diagnosis, purely wedge and signs are also important. With L.'s disease. the upper and lower groups of facial muscles are involved to the same extent. With central paralysis, the muscles of the lower half of the face suffer significantly more; paralysis of the muscles of the upper facial group is almost absent. The muscles of the upper parts of the face are innervated from that part of the nucleus of the facial nerve, which receives bilateral supranuclear (corticonuclear) pathways.
In most cases, the course and prognosis of primary neuritis L. and. favorable. Mild cases are observed with complete restoration of facial movements within 2-3 weeks, moderate cases last approx. 2 months, sometimes recovery occurs only after 5-6 months. First, the function of the muscles of the upper half of the face is restored, then the lower half. Complete restoration of facial muscles is observed in approximately 70% of cases. Some patients develop contractures of paretic muscles. On the diseased side, the palpebral fissure narrows, the corner of the mouth is pulled up, and on the healthy side, the nasolabial fold is smoothed out. During the study, it is established that the affected side is the one on which differentiated movements are difficult. Patol and synkinesis are observed. When smiling, laughing, or showing teeth, an even greater narrowing of the palpebral fissure occurs at the same time, the eye may close, and when closing the eyes, the corner of the mouth tightens. Tic twitching of the corners of the mouth, orbicularis oculi muscle, and cheeks appears. Mild synkinesis and isolated tic-like twitches may persist after complete restoration of the function of the facial muscles. Recurrences of catarrhal neuritis L. are possible. both on the same and on the other side. They are rare and in some cases they are more severe, in others they are milder than the initial disease.
Paralysis of the facial muscles is not difficult to establish; it is more difficult to differentiate primary neuritis of L. n. from secondary. Combined lesion of L. n. and other cranial nerves, pyramidal and other conduction disorders indicates the secondary nature of the disease. In all cases of neuritis L. n. An otological examination should be performed. Otitis, especially chronic ones, may be accompanied by damage to L. n. in the channel. Primary neuritis may be indicated by the acute development of the disease, its occurrence in connection with cooling, in some cases after a sore throat or flu. To identify early signs of contractures, a study of the state of electrical excitability of the affected nerve is carried out (see Electrodiagnostics).
Facial nerve damage
There are damages to L. n. for fractures of the base of the skull, wounds of the parotid region, surgical interventions on the ear, salivary gland and total removal of acoustic neuromas. In case of fractures of the base of the skull, the nerve is damaged at the junction of the horizontal section of the LN canal. to vertical. The degree of nerve damage varies. When a nerve ruptures, early paralysis of the facial muscles develops; when the nerve swells or the blood circulation in it is disrupted, late paralysis develops, appearing 10-14 days after the injury.
During ear surgeries, nerve damage can be primary or secondary, when the nerve is compressed by bone fragments or hematoma; open - when the integrity of the L. n. channel is violated. and closed. During operations on the parotid gland or injuries to this area, the extracranial part of the nerve distal to the stylomastoid process is damaged. With total removal of acoustic neuromas of the L. n. is damaged along the path from the brain stem to the internal auditory canal.
Diagnostics
An experienced neurologist will be able to diagnose the problem with the naked eye. But to determine the cause of the disease, a number of instrumental studies will be needed.
CBC (complete blood count)
The development of the disease is indicated by the following indicators:
- increased erythrocyte sedimentation rate;
- increased number of leukocytes;
- decrease in lymphocytes as a percentage.
Analysis data may indicate chronic meningitis or otitis media, which caused compression of the facial nerve.
MRI
Thanks to the procedure, some causes of the disease can be identified:
- tumors in the brain;
- progressive heart attack;
- abnormal arrangement of blood vessels;
- damage to the meninges .
MRI allows the neurologist to prescribe an appropriate treatment regimen for the patient.
CT
The procedure, like MRI, allows you to identify the anomalies that caused facial neuralgia:
- tumors;
- stroke;
- brain injuries
Depending on the CT results, a tactic will be chosen to combat the problem - removal of the tumor or restoration of blood supply.
Electroneuromyography
The procedure allows you to determine the speed of propagation of impulses along the nerve. The following data indicate the signs of the disease:
- reduced speed of electrical signals;
- impulse transmission to one of the nerve branches;
- insufficient number of muscles excited by electrical signals;
- weak reaction of the facial muscles to conducted impulses.
Electromyography
The technique detects impulses in muscles without exposure to electric current. The study is often prescribed in combination with electroneurography. In case of illness, the procedure reveals some deviations:
- slow passage of the signal along the nerve;
- reducing the number of fibers .
These data indicate damage to the nerve endings. The technique does not reveal the inflammatory process itself, but diagnoses its complications - muscle atrophy. A repeated procedure, carried out several weeks after the first, makes it possible to judge the effectiveness of the prescribed treatment regimen.