Seal
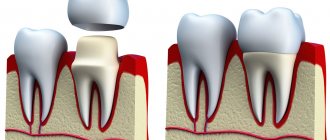
One of the most popular procedures in modern dentistry is the installation of crowns. The method allows you to save a damaged tooth, restore its function, and restore the attractiveness of your smile. But sometimes after orthopedic treatment, discomfort, sharp or dull pain, and sensitivity to temperature occur under the crown. In this case, discomfort may appear both in the coming days after prosthetics and several years later. What should be done in this case?
First of all, you need to understand what is causing the pain. If very little time has passed after treatment and the discomfort is not too great, do not worry. Such pain is residual in nature. As a rule, specialist intervention is not required - 3-5 days after treatment, the discomfort goes away on its own. It’s worse when the tooth starts to hurt months or even years after prosthetics. In this case, you cannot do without a visit to the clinic.
Khashchenko Stanislav Sergeevich is a dental surgeon with extensive experience.
Causes of pain
Unpleasant sensations can arise for various reasons. Sometimes this is a common reaction after the procedure, because the tissues need time to heal and adapt to the new structure.
Usually the pain is aching in nature and lasts no more than 3 days. If the pain is acute, does not go away and even intensifies, or at first it was not there, but some time after installing the crown it appeared, you should consult a doctor. Perhaps inflammatory processes have begun, and it is no longer possible to do without medical help. Causes of toothache under a crown.
The process of installing a crown on a tooth is a team effort of three specialists: a dentist-therapist, an orthopedic dentist, and a dental technician. A mistake in one of them can lead to unpleasant sensations.
What to do if your tooth hurts after having a crown installed?
- home
- For patients
- Interesting
- What to do if your tooth hurts after having a crown installed?
- What to do if your tooth hurts after having a crown installed?
- Interesting
- home
For patients
Installation of temporary or permanent crowns is a necessary step after the loss of one or more teeth. Any dental surgery has a risk of complications, and the installation of dentures is no exception. Pain after crown installation can occur either immediately or after a certain period of time. Regardless of the reason, you must promptly make an appointment with a doctor.
Why does my tooth hurt after having a crown installed?
Only a dentist can make a correct diagnosis after examining the tooth and taking an x-ray. Pain in the first days after installation of the prosthesis indicates improper preparation for the operation, and in a later period – an exacerbation of chronic processes. Often patients are also concerned about tooth loosening, redness, bleeding and sensitivity of the gums. Let's consider the main reasons for repeated treatment after prosthetics:
- inflammation of the nerve bundle (tooth pulp), if the tooth has not been depulped;
- if a tooth hurts after pulp removal, this may be a sign of caries or an allergic reaction;
- rubbing the gum crown;
- the occurrence of periodontitis – inflammation of the tooth root;
- infection during medical intervention;
- excessive filling of the canals with filling material;
- poor oral hygiene after prosthetics;
- wear or damage to the crown of the tooth.
Tooth hurts after crown installation: first aid
Only a dental specialist can provide competent assistance, but you should not endure pain and spend a sleepless night. For quick help with acute symptoms, you can use medicines and folk remedies:
- Take classic painkillers from your home medicine cabinet. It may be an analgesic or an anti-inflammatory agent. It is recommended to use the tablets in minimal quantities, as this may affect the effect of the anesthesia in the doctor's office.
- Rinse your mouth with a warm herbal decoction. For the best effect, it is recommended to rinse several times using chamomile, sage, and oak bark.
- Relieve pain with cold - press a towel with an ice cube inside to your cheek.
Solving a problem in dentistry
It is a mistake to believe that there is a norm for how much a tooth hurts after a crown is installed. If you feel unwell, schedule an examination and x-ray with your doctor. If the crown fits poorly, a sharp reaction to eating hot and cold food occurs. In this case, it must be replaced. Another common symptom is pain when pressing on a tooth or the appearance of blood when brushing. The doctor will draw up an anti-inflammatory therapy plan and, if necessary, correct the tooth stump. Pay attention to the period of wearing the crown. When a denture wears out, it can become a problem for your oral health.
Methods for treating a tooth that hurts after a crown:
- replacing a crown that is installed incorrectly,
- carrying out drug treatment: prescribing anti-inflammatory, antibacterial and antihistamine procedures and drugs,
- treatment of the oral cavity, professional cleaning of teeth and dentures,
- cleaning the tooth canals during inflammation, if this has not been done before,
- re-processing the roots.
If there is massive destruction of the tooth under the crown, it will need to be removed. ROMDENT dentists try to find a way out of any difficult situation and save the tooth. If this is not possible, we will offer you alternative methods of prosthetics and implantation. After installing any denture, follow your doctor's recommendations about dental hygiene and regularly check the condition of your teeth at a preventive examination.
Habits that ruin your teeth every day
| Poor canal filling. If necessary, before installing a crown, the doctor removes the neurovascular bundle (pulp) and then fills the dental canals. If the canals are severely curved or the doctor does not have enough experience, then mistakes may be made during the procedure, which can cause pain in the tooth. These include:
It is important that before and after canal treatment the dentist takes targeted photographs - this is the only way to identify all the shortcomings | |
| Poor quality materials. Poor filling material begins to settle and does not adhere so tightly to the walls of the tooth, thereby eliminating the tightness. Sometimes the filling cracks, and through these micro-cracks an infection enters the tooth, which causes the development of caries under the crown. | |
| Perforation of the root wall. If the roots are severely bent, the doctor may not calculate the force of pressure on the drill. As a result, the channel is drilled through. If the error is not corrected, the infection can penetrate into the tooth from below and lead to caries. Perforation can also occur if the pin is not installed correctly. | |
| Fracture of the instrument in the canal. The disposable root canal drill is very thin and fragile. If the channels are strongly curved, then with strong rotation and awkward movement of the doctor, the tip of the instrument may break off. There are other reasons why a foreign body remains in the canal:
| |
| We recommend taking a panoramic photo of the jaw (OPTG) before installing a crown. It will allow you to timely detect deformation of the canals, the presence of inflammation and particles of instruments in the canal. | |
| Incorrect crown size. There are several reasons for this: an error during taking impressions; deformation of the material from which the impression is made; the crown was installed without fitting;; The dental technician did not correct the defects after trying on the crown. | |
| Error in crown installation. The crown does not fit tightly to the tooth, or it is installed without taking into account the bite - it can be too high or low - this injures the antagonist teeth. | |
Indications for tooth extraction
Tooth extraction along with a crown is done urgently or routinely in the following situations:
- purulent inflammatory process on the roots of the tooth, which cannot be controlled with medication and does not go away after drainage;
- acute osteomyelitis, periostitis or phlegmon of the jaw, which do not respond to conservative measures and serve as a source of odontogenic infection;
- tooth fracture, in which it is impossible to restore its integrity with filling materials or a stump inlay;
- the presence of a focus of chronic infection in the periodontium and the inability to complete endodontic treatment (obstruction, curved root canals, perforation of the tooth cavity or root wall);
- severe tooth mobility (grade 3 periodontitis), tooth protrusion by more than 2/3.
Pain under the crown due to the patient's fault
Unpleasant sensations are not always associated with the work of dentists. They often arise against the background of the patient’s negligent attitude towards his health.
- Poor oral hygiene.
Plaque and food particles accumulate around the gums. Soft plaque gradually transforms into tartar, which contains a lot of bacteria. They provoke inflammation of the gums and gradually penetrate inside the tooth. - Ignoring preventive examinations
. Every six months it is necessary to visit the dentist to prevent various complications. This will help maintain dental health and extend the life of the structure. If dental problems are detected, the doctor will offer treatment options. Remember, timely treatment is always cheaper and does not take much time. - Heavy load on the tooth.
Excessive consumption of nuts and other solid foods can damage the seal of the crown, which can then lead to caries.
What is periodontitis?
We can easily notice changes in the appearance of teeth and the appearance of carious lesions on the enamel at home, limiting ourselves to one visual examination of the oral cavity. But things are completely different when you need to know the condition of the pulp. The pulp is the heart of the tooth, which is hidden from prying eyes. To see it, you need to undergo an x-ray examination by a dentist. The same applies to the root and basal tissue of the tooth; their diagnosis is carried out only using an x-ray. Inflammation of the periodontal tissues can be fraught with dangerous consequences; if the infection penetrates deep into the tooth and goes beyond the root canals, a person may lose the tooth.
How is the treatment carried out?
Of course, the simplest option is this: the doctor removes the crown, treats the tooth, and then installs the crown again. But the disadvantage of this method is that the patient will have to pay again for all orthopedic work, including the crown.
However, today you can go a different route, which is offered by some dentists. In this case, the tooth is treated without removing the structure. The doctor makes a hole through which he performs the necessary manipulations, and then seals it.
Before treating a tooth, a photograph is always taken under the crown. If the problem is not detected on the diagnostic image, then the crown will need to be removed to determine the cause of the pain.
Treatment of a living tooth
If the cause is caries, then treatment; most often performed through the crown. Main signs: pain is sharp and severe, the tooth reacts to hot and cold.
If the reason is a violation of the fixation of the crown, then the crown is removed, medicine is applied to the ground tooth, and then the crown is put back.
Treatment of a pulpless tooth
Signs: aching pain, accompanied by pulsation in the temple and ear. Treatment is carried out both with and without crown removal - it depends on the presence of a pin and the cause of pain (periodontitis, a fragment of an instrument in the root, etc.).
How to remove a tooth with a crown
Before the start of surgery, an X-ray examination is performed, which allows the doctor to understand the scale of the operation and outline the sequence of actions. When removing a tooth covered with a single crown, and there are suitable conditions in the bone for this, the doctor may suggest immediate implantation, i.e. implantation of a titanium root in place of an extracted tooth.
Extraction is always performed under local anesthesia. If a patient has dental phobia, then at the Refformat clinic he can be offered sleep treatment (the cost of 1 hour of sedation is 13,900 rubles).
Removing a tooth with a crown and inlay is a more complex operation due to the fact that the inlay along with the crown may separate from the tooth and then the doctor will have to remove it in parts.
After extraction, an anti-inflammatory and wound-healing material is inserted into the hole, which is absorbed as the wound heals. If, after removal, it was decided to undergo implantation, then the tooth is removed from the alveolar socket as carefully as possible, so that all its walls remain intact. The success of implantation and the degree of stabilization of the titanium pin depend on this. For the same purpose, the implant is “lined” with osteoplastic material. The doctor’s further actions depend on the area on which the operation was performed. If this is the front, the defect is closed with a temporary prosthesis, but if the removal was performed in the area of the chewing teeth, temporary structures are not necessary.
How to relieve pain
The tooth under the crown can get sick at any time. How to relieve symptoms if it is not possible to see a doctor soon?
- Painkillers (Ketanov, Nise, Ibuprofen, etc.)
- Rinse your mouth with a solution of baking soda and salt.
- Rinse your mouth with a decoction of chamomile or sage
Remember that pain is the body's signal for help. Constantly ignoring and drowning out the pain with improvised means can worsen the problem, and then the only solution will be tooth extraction.
Symptoms and signs of periodontitis.
As mentioned earlier, periodontitis may not manifest itself for a long time; the patient runs the risk of finding out about the disease too late, when it has entered the acute stage. In this case, the signs of inflammation of periodontal tissues will be felt much more clearly. Periodontitis is characterized by the following symptoms:
Deterioration of general condition.
There is an increase in temperature, worsening sleep, weakness, etc.
- Pain when chewing food and when closing the jaws.
- Change in gum color (become darker).
Based on this symptom, periodontitis can be identified in its initial stages of development. Also, the periodontal tissues may swell, and the swelling may spread to the cheek and neck.
Painful sensations.
In the acute course of the disease, the patient begins to be bothered by a sharp, aching pain that radiates to neighboring teeth.
- Slight tooth mobility.
- The appearance of bad breath.
- Increased sensitivity due to mechanical impact on the tooth.
Types of periodontitis.
There are several classifications of periodontitis; it is usually distinguished by the place of formation: apical (infection affects the base or apex of the root) and marginal (occurs in the area of the gum edge due to injury).
According to the nature of the course of the disease, the following stages are distinguished:
Acute periodontitis.
It is further divided into several forms: serous acute periodontitis is the initial stage of the development of inflammation; it occurs after the infection penetrates through the apex of the tooth root into the periodontal area. Then it develops into purulent acute periodontitis. This form of the disease is very dangerous because The pus penetrates the bone structures and can spread throughout the body. It is characterized by: severe increasing pain, painful sensations when pressing on the tooth and when biting, headache, swelling of the mucous membrane, etc.
Chronic.
It has three stages of development: fibrous, granulating and granulomatous. Chronic periodontitis is characterized by a calm and even imperceptible course of the inflammatory process; only sometimes the patient may experience slight pain when tapping a painful tooth. But at the same time, this stage is considered the most dangerous, because may lead to tooth loss. With the development of the granulating form, the unit and the tissues around it are destroyed. A fistula forms on the gum, from which pus flows. Granulomatous periodontitis is characterized by the formation of a granuloma, a sac filled with purulent fluid, which subsequently develops into a cyst if not removed. Tooth mobility increases, gums bleed, and abscesses develop.