From this article you will learn:
- what is acute and chronic sinusitis,
- how to recognize the symptoms of sinusitis,
- causes of the disease,
- how to treat sinusitis in adults.
Sinusitis (from the Latin sinusitis) is an inflammation of the mucous membrane that lines the paranasal sinuses from the inside. Inflammation can be localized in only one of the sinuses, or in several at once. Most often, the maxillary sinuses (maxillary sinuses), which are located in the projection of the apices of the roots of 5-6-7 teeth on each side of the upper jaw, are susceptible to inflammation. This disease is usually called the terms maxillary sinusitis or sinusitis (Fig. 2).
Sinusitis (in addition to the maxillary sinuses) can also be localized in the frontal sinuses, sphenoid sinuses, and also in the cells of the ethmoid bone. To designate it in these cases, the terms frontal sinusitis, sphenoiditis and ethmoiditis are used, respectively. However, most often patients have to deal with maxillary sinusitis, which is primarily due to some anatomical features of the maxillary sinuses.
Diagram of the paranasal sinuses -
In this article, we will first look at maxillary sinusitis - symptoms and treatment in adults, talk about modern methods of diagnosis and therapy (computed tomography, endoscopic endonasal maxillary sinusitis, as well as modern radical treatment methods, for example, endoscopic maxillary sinusotomy and others).
What are the maxillary sinuses?
There are two such sinuses (one on each side of the upper jaw). The average size of the maxillary sinuses in an adult: from 2.5 to 3.5 cm in width, from 3.6 to 4.5 cm in height, from 3.8 to 4.5 cm in depth. The sinuses are filled with air, and their inner surface is lined with mucous membrane. In Fig. 3 you can see that the upper bony wall of the sinus is also the lower wall of the orbit, and the bottom of each sinus is separated from the apices of the roots of 5-6-7 teeth by only a thin layer of bone tissue (on average from 1 to 3 mm).
It is important that the maxillary sinuses communicate with the nasal passages (using special anastomoses, i.e. openings). Thanks to these holes, there is a constant physiological cleansing of the sinuses from mucus and desquamated epithelial cells. However, it is the presence of such anastomoses and the proximity of the sinus to the apexes of the roots of the teeth of the upper jaw that determine the main reasons for the development of maxillary sinusitis in adults and children.
Causes of maxillary sinusitis –
The main causes of the development of maxillary sinusitis can be divided into 3 groups (in descending order):
- acute and chronic inflammatory diseases of the nose,
- foci of inflammation at the roots of the upper teeth,
- fractures of the upper jaw and zygomatic bone.
Most often, the development of maxillary sinusitis occurs against the background of a runny nose during acute infectious diseases (for example, ARVI and influenza), as well as against the background of chronic rhinitis.
These causes account for about 62% of all cases of the disease. In this case, most often inflammation occurs in the presence of predisposing factors, for example, a deviated nasal septum, obstruction of the nasal passages, or against the background of allergic rhinitis or polypous growths in the nasal passages. An equally important role is played by the patency of the anastomosis connecting the maxillary sinuses with the nasal cavity, through which the process of physiological cleansing of the sinuses occurs. The second large group of causes are causes of odontogenic origin (i.e., related to teeth). In approximately 32% of cases, the development of maxillary sinusitis is associated with inflammatory foci at the apexes of the roots of the 5-6-7 teeth of the upper jaw. The fact is that the bottom of the maxillary sinuses is located only 1-3 mm from the apexes of the roots of these teeth, and therefore, if a focus of inflammation occurs at the apex of the root, the inflammation can also affect the mucous membrane of the sinuses (Fig. 5).
Odontogenic maxillary sinusitis can also develop - 1) due to errors in filling root canals, when the filling material is removed beyond the apex of the root, 2) as a result of pushing the infected pulp beyond the apex of the root during the treatment of pulpitis and periodontitis, 3) when perforation of the maxillary sinus occurs, caused by time of removal of the lateral teeth of the upper jaw, 4) as a complication during implantation of teeth in the lateral parts of the upper jaw.
Important: a large group of patients may simultaneously have both rhinogenic and odontogenic causes of sinusitis.
For example, in the area of the apex of the roots of the 5-6-7 upper teeth, the patient may have foci of chronic inflammation, which in themselves did not cause inflammation of the mucous membrane of the maxillary sinuses. But in the case of the development of ARVI, not only an acute runny nose develops (which makes it difficult for the mucous secretion to drain from the maxillary sinuses), but also the activation of inflammatory foci in the area of the apexes of the roots of the teeth. The combination of these factors greatly increases the risk of developing sinusitis in a patient.
What are the sinuses and the ethmoidal labyrinth?
The sinuses are fairly large cavities located in the upper jaw area that lighten the weight of the bone. The area of these sinuses is located directly under the eyes. When examining x-rays, you can see a darkening in this area, indicating the absence of any abnormalities.
Experts today have not been able to establish the significance of the paranasal sinuses in human evolution, but they suggest that the cavities are necessary to increase the volume of the maxillary bone and reduce the overall mass of the skull bones. Air enters the paranasal sinuses through the ethmoid labyrinth, which has the appearance of a bone with many small round holes.
The ethmoid labyrinth is located on the bone of the same name, which is localized in the area of the bridge of the nose and stands slightly higher than the maxillary.
It is worth noting that the bone really has the appearance of a labyrinth with several curls, and there are holes on them.
Both the maxillary sinuses and the ethmoidal labyrinth are paired bones that play a critical role in the breathing cycle, as well as in the formation of the timbre of the human voice.
Acute sinusitis -
As we said above, acute sinusitis can be rhinogenic or odontogenic. In the first case, it will develop against the background of acute respiratory viral infections and influenza, chronic nasal diseases, and allergic rhinitis. And in this case, the development of sinus inflammation occurs against the background of a runny nose, nasal congestion, and the development of swelling of the mucous membrane of the nasal passages. The fact is that swelling of the mucous membrane leads to a narrowing or complete closure of the openings between the maxillary sinuses and the nasal cavity, which leads to disruption of the outflow of mucous secretion from the sinus and serous exudate formed during inflammation.
If the development of sinusitis is associated with teeth, very often patients complain of pain in one of the lateral teeth of the upper jaw, which preceded the onset of sinusitis. In some patients, the pain may be sharp and throbbing, while in others it appears only when biting on the causative tooth. Some patients may experience only slight discomfort in one tooth, but in some cases there may be no toothache at all (in which case the causative tooth can only be identified through an x-ray). In such patients, sinusitis does not develop against the background of a runny nose and nasal congestion, and nasal discharge appears only later.
At the first stage of the development of sinusitis - in addition to a runny nose and nasal congestion with rhinogenic sinusitis, or pain in one of the teeth with odontogenic sinusitis - the patient is usually initially only bothered by malaise. In the initial period, the inflammation is serous in nature and the formation of pus in the sinus does not yet occur. Mucous discharge from the nose during this period still has a transparent color, without an unpleasant odor. In general, the patient does not present any active complaints at the initial stage, but everything changes when serous sinusitis gradually turns into purulent sinusitis.
Symptoms during the transition of serous sinusitis to purulent:
- Purulent exudate may be released from the nasal passage on the side of the inflamed maxillary sinus, the discharge of which may intensify when the head is tilted forward (Fig. 7). In the morning, you can often notice traces of pus leaking from the nose on the pillow. But if the outflow of purulent exudate from the sinus into the nasal cavity is completely disrupted, then such a symptom may be absent.
- A feeling of heaviness may appear in the corresponding half of the face, which is typical if only one maxillary sinus is inflamed.
- When pressing on the skin in the projection of the anterior wall of the sinus, pain may be felt. In addition, pain or discomfort may be felt when tapping on the teeth located in the projection of the inflamed sinus (usually the 5-6-7 teeth of the upper jaw).
- Common symptoms include lethargy, weakened sense of smell, chills, loss of appetite, and weakness.
- Body temperature can rise to 37.5 - 39.0 degrees (sometimes higher).
- Increasing pain, which is initially localized in the projection of the inflamed sinus, but then can spread to the frontal, temporal, occipital regions, and to the area of the upper jaw teeth.
- With severe sinusitis, swelling of the soft tissues of the face may also be observed due to their edema, redness, as well as the development of purulent purulent periostitis from the oral cavity.
Computed tomography and radiography –
The final diagnosis is made based on the symptoms of maxillary sinusitis and data from computed tomography or radiography. It is optimal to do a computed tomography (CT) scan, because Such photographs will allow not only to examine the sinuses in different projections, but also to simultaneously inspect all the teeth of the upper jaw - for the presence of inflammatory foci and poorly filled root canals. The latter is very important for establishing the cause of sinusitis and choosing the right treatment tactics (24stoma.ru).
At the end of the article, we will present a specific clinical case in which the patient was mistakenly diagnosed with maxillary sinusitis of rhinogenic origin. As a result, she was tormented for several years with punctures, rinses, and antibiotics, while she had classic odontogenic sinusitis (the cause of which was a focus of inflammation at the apex of the root of one of the teeth in the upper jaw). Therefore, it is very important to conduct a full diagnosis and establish the correct cause of the disease.
CT scan of the paranasal sinuses (normal and pathological) –
An important feature of CT is that it allows you to visualize not only the filling of the sinus with pus. For example, with chronic maxillary sinusitis, there may be no pus in the sinus at all, and the process develops like catarrhal inflammation (hyperplastic thickening of the sinus mucosa). In this case, CT allows us to consider in which areas of the mucous membrane in the sinus changes occur. For example, if we see changes in the area of the bottom of the sinus, we immediately assume that the inflammation is associated with the teeth.
If the mucous membrane is thickened primarily in the area of the anastomosis with the nasal passages, then first of all we assume that the inflammation is of a rhinogenic nature (i.e., the infection has spread from the nasal cavity). As for traditional radiography, it is much less informative and only allows one to judge the presence of inflammation in it by the degree of darkening of the sinus, as well as see the level of pus in the sinus.
Acute purulent sinusitis on x-ray –
Chronic sinusitis: symptoms
Acute maxillary sinusitis in adults, in the absence or improper treatment, can very quickly become chronic. If you have developed chronic sinusitis, the symptoms in adults depend on the form of chronic inflammation, which can be either catarrhal, or purulent, or polyposis, or purulent-polyposis.
- Catarrhal form - this form is usually practically asymptomatic, but with periodic, not pronounced exacerbation of the inflammatory process.
During exacerbations, patients may complain of a feeling of heaviness in a certain half of the face (due to the inflammatory process), periodic disruption of nasal breathing, as well as some malaise at the end of the day. During an instrumental examination of the nasal passages, the ENT doctor can detect swelling and cyanosis of their mucous membrane. X-rays for this form of sinusitis usually do not give results at all, but a CT scan may show thickening of certain areas of the mucous membrane in the sinus (in areas of inflammation). You can see the catarrhal form of sinusitis in the CT image in Fig. 9 - in the sinus (on the left in the image) you can see a thickening of the mucous membrane in the area of the bottom of the sinus, as well as the wall adjacent to the nasal passages.
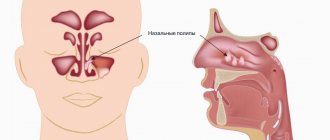
- Purulent and polypous forms - the diagnosis of chronic sinusitis is made based on symptoms and X-ray or CT data, as well as endoscopic sinusoscopy. In the purulent form, the sinus will be partially filled with purulent exudate, and in the polypous form, there will be growths of polyps on the surface of the mucous membrane (a combined purulent-polypous form of sinusitis may also occur). Polyps in the maxillary sinus are no different from polyps that often grow in the nasal passages, and they look the same (Fig. 12).
Patients with purulent and polypous forms of chronic sinusitis usually present the following complaints:
→ fatigue, → putrid odor, → periodic discharge of pus from the corresponding half of the nose, → temperature 37.5 – 37.8.
Chronic sinusitis in the acute phase -
If the source of inflammation of the sinus mucosa has not been eliminated, or improper treatment or self-medication has been carried out, the acute inflammatory process becomes chronic, which in turn is characterized by a wave-like course. The latter means that periods of remission will periodically be replaced by exacerbations (a wave-like course of inflammation). Exacerbations of chronic sinusitis can occur for various reasons, for example, against the background of hypothermia or decreased immunity, against the background of acute respiratory viral infections, exacerbation of chronic inflammation in the area of the apexes of the roots of 5-6-7 teeth, etc.
Chronic sinusitis in the acute phase is characterized by symptoms similar to acute maxillary sinusitis, which we described above. Very often, the development of chronic sinusitis is a complication of incorrect actions by the doctor, or when the patient is addicted to self-medication. Below I will demonstrate an example from my own clinical practice.
Vasomotor sinusitis
It develops in people with disorders of the autonomic nervous system and nasal breathing against a background of negative emotions and stress.
Clinical manifestations
Allergic and vasomotor symptoms are manifested by sneezing, difficulty in nasal breathing, and discharge of large amounts of contents from the nose. Most often this is pansinitis.
Diagnostics
In this case, ACMD-Medox can use both SCT and MRI with equal benefit. With classical radiography, there may be options for under- and over-diagnosis associated with the nature of the visualization of pansinuit in the images.
Maxillary sinusitis: treatment
Treatment of maxillary sinusitis begins with establishing the cause of its occurrence, and this is the most important stage in treatment. You probably already realized that if sinusitis is associated with teeth (odontogenic origin), the treatment should be completely different than if the cause was an infection in the nasal cavity (rhinogenic origin). Plus, you should know that there are also combined causes that aggravate each other.
With the causes of rhinogenic origin, everything is basically clear here - these are acute and chronic inflammatory processes in the nasal passages, occurring with acute runny nose and/or nasal congestion, etc. But the dental causes of maxillary sinusitis are more interesting. Firstly, there are poorly filled root canals in the area of 5-6-7 teeth and foci of inflammation at the apexes of the roots of these teeth. Secondly, the cause of sinusitis can be filling material that is abundantly removed beyond the apexes of the roots (when filling root canals).
Thirdly, sinusitis can occur as a result of traumatic removal of 5-6-7-8 teeth. For example, the doctor may push a fragment of tooth or bone tissue into the sinus. Or he can simply make a perforation (a hole through the sinus) with an instrument. According to the rules, after this the doctor must perform gum surgery to tightly sutured the extraction site, but in fact, 95% of dental surgeons simply do not do this. As a result, a fistula is formed between the oral cavity and the sinus, and infection from the oral cavity penetrates into the sinus, causing inflammation in it. Next we will talk about how to treat sinusitis.
Establishing diagnosis
Several examination methods are used to make a correct diagnosis. The initial stage is a general examination and interview of the patient, listening to complaints and identifying the conditions for the appearance of symptoms of the disease. After this, the doctor prescribes a general and biochemical blood test.
These studies are mandatory because they help identify common signs of inflammation. After this, the patient is sent for fluoroscopy of the maxillary sinuses. In the image, the specialist can see deviations from the bones, especially the nasal septum.
The next stage of the examination is rhinoscopy. This method is a study of the nasal passages with a special device. At the same time, the doctor notes the degree of damage to the mucous membranes and detects possible complications.
If necessary, magnetic resonance imaging is prescribed, which allows you to see polyps and other neoplasms, as well as complications. Based on diagnostic data, treatment is prescribed.
Treatment of acute sinusitis –
Acute maxillary sinusitis of rhinogenic origin can be cured without the use of antibiotics, but only if you consult a doctor at the very beginning of the development of inflammation (until serous inflammation turns into purulent). The most important thing at this stage is to relieve swelling of the nasal mucosa, because the edematous mucous membrane increases in volume and blocks the anastomosis between the maxillary sinus and the nasal cavity. Removing edema will normalize the outflow of serous inflammatory exudate from the sinus.
Traditional sprays for the common cold can be used for no more than 2-3 days, because their longer use leads to the opposite effect - persistent swelling of the mucous membrane. Therefore, in order to quickly relieve swelling of the nasal mucosa, it is better to use such remedies only during the first 2 days. An exception may be the spray for runny nose “Rinofluimucil”, which can be used for up to 7 days. This drug not only relieves swelling of the nasal mucosa, but also reduces the viscosity of mucopurulent discharge (i.e., it will improve the outflow from the sinuses).
After eliminating acute symptoms, it is better to switch to the drug “Nasonex” (spray), which contains low dosages of glucocorticoids that do not have a systemic effect. This drug has a pronounced anti-inflammatory, anti-allergic and anti-edematous effect, and is used for up to 3 weeks. In addition, the doctor may additionally prescribe you herbal preparations “Sinupret”, “Sinuforte”, “GeloMyrtol Forte” (they stimulate the removal of inflammatory exudate from the sinuses). However, they can only be used when the outflow of exudate from the sinus is not impaired.
Drugs for the treatment of sinusitis in adults -
If the serous process has turned purulent, then there are all indications for antibiotic therapy, as well as for rinsing the sinuses through the nose. For lavage, it is better to use the YAMIK sinus catheter - today this is the best and most effective option. And if the clinic doesn’t use it, but does traditional punctures, then this is not a serious clinic at all and it’s better to run away from there. How to choose a good clinic: serious ENT clinics always perform endoscopic maxillary sinusotomy using a shaver, and sinus lavage is carried out only using a Yamik sinus catheter.
Antibiotic therapy for sinusitis -
Antibiotics of choice for the treatment of sinusitis:
- β-lactam lactamase-protected synthetic penicillins (amoxicillin + clavulanic acid, or ampicillin + sulbactam, or piperacillin + tazobactam, or cefoperazone + sulbactam, or ticarcillin + clavulanic acid), or carbapenems (imipenem or meropenem).
- Macrolides (azithromycin, clarithromycin).
- Modern fluoroquinolones (levofloxacin or moxifloxacin).
- III-IV generation cephalosporins (ceftriaxone or cefepime).
- Oxazolidones (linezolid) – only when multi-resistant microflora are isolated.
When treating mild to moderate forms of sinusitis, it is better to start treatment with β-lactam lactamase-protected synthetic penicillins. The best option would be a combination of amoxicillin with clavulanic acid, for example, tablet preparations such as Augmentin, Amoxiclav and others. But in severe cases, it is worth choosing either from modern fluoroquinolones, or one of the III-IV generation cephalosporins (but all these drugs in severe cases should already be administered parenterally).
If the patient is intolerant to penicillins - in mild and moderate forms of the disease, we prescribe, for example, macrolide antibiotics or fluoroquinolones (in tablets), and in severe forms - some of the fluoroquinolones (parenterally). And we remember that if you are intolerant to penicillins, you cannot prescribe antibiotics from the cephalosporin group. It is also worth considering that with long-term chronic sinusitis, fungal flora can often join the bacterial infection and, therefore, such patients should be additionally prescribed antifungal drugs (after culture for microflora).
The total duration of antibiotic use usually ranges from 7 to 10 days, but in some cases up to 14 days. We sincerely advise you never, under any circumstances, use Russian-made antibiotics (unless you want to find out what pseudomembranous colitis is). It is also worth considering that the effectiveness of antibacterial therapy increases significantly when, in parallel with the patient, procedures for washing the sinuses with antiseptics are carried out (for example, using the Yamik sinus catheter).
→ Antibiotic treatment regimens for sinusitis (sinusitis)
Important: do not forget that if acute sinusitis is associated with the formation of inflammatory foci at the apexes of the roots of 5-6-7 teeth, then at the same time you urgently need to contact a dentist-therapist to open the causative tooth and disinfect the root canals in it using drugs for based on calcium hydroxide (the drug is placed in the root canals for about 1 month). Keep in mind that if sinusitis is odontogenic in nature, then antibiotic therapy without sanitizing the source of infection in the root canals will be ineffective.
And I would also like to say a few words to patients who are planning to cure their sinusitis at home, using available means, for example, regular nasal rinses and taking antibiotics. In essence, this is useless, although it can lead to short-term improvement, plus it will cause the process to become chronic and require surgical treatment in the future.
How to treat chronic sinusitis –
If you have chronic maxillary sinusitis, treatment should also begin with determining the cause and source of infection. Patients who are treated for purulent and polypous sinusitis are usually always severe. These are patients with a long history of self-medication and antibiotic use. Many of them then have to be sent for radical maxillary sinusotomy in a hospital setting, but in some cases more gentle techniques can be used.
Modern methods for diagnosing chronic sinusitis are CT or endoscopic endonasal maxillary sinusoscopy. As for treatment methods, this is still lavage of the sinuses using the YAMIK sinus catheter and antibiotic therapy, which in most cases are supplemented by surgical techniques - such as endoscopic endonasal maxillary sinusotomy or radical maxillary sinusotomy.
Computed tomography (CT) - at the diagnostic stage, it is important to do a CT scan and evaluate the condition of the sinus mucosa, whether there are inflammatory foci at the apexes of the roots of the 5-6-7 upper teeth on this side, how well the root canals in these teeth are sealed. Sometimes it happens that the apices of the roots are located immediately under the mucous membrane of the maxillary sinus. In these cases, infection from poorly filled root canals directly affects the mucous membrane of the sinus, without the formation of a traditional inflammatory focus in the area of the apex of the tooth root.
But in some cases, this can lead to the development of an inflammatory focus in the form of a cyst, which penetrates the maxillary sinus and is filled with pus. As we said above, such cysts can only be diagnosed outside the period of exacerbation (when the sinus is not filled with pus), using CT or endoscopic sinusoscopy.
Endoscopic endonasal maxillary sinusoscopy - in some cases it is important to do a diagnostic endoscopic maxillary sinusoscopy - it is done through the nose using a thin flexible probe with a video camera. This allows you to look at the sinus from the inside (determine the presence of polyps and the degree of damage to the sinus, etc.), and also decide whether it is necessary to expand the anastomosis between the sinus and the nasal cavity. In the price list, this service may also be called “Diagnostic endoscopy of the maxillary sinuses,” and its cost on average will be about 2,000 rubles for 1 sinus.
Carrying out endoscopic maxillary sinusoscopy:
Commentary on the video - in the sinus, the tops of the three roots of the 7th tooth are clearly visible, which are visible through the mucous membrane, as well as a cyst up to 1 cm in size (having a round shape and yellow color), filled with pus. Endoscopic sinusoscopy is performed under local anesthesia.
Surgical treatment methods (sinusrotomy) –
1) Endoscopic endonasal maxillary sinusotomy - based on the results of diagnostic maxillary sinusoscopy (if there are polyps, foreign bodies in the sinus, etc.) - endoscopic gentle maxillary sinusotomy is prescribed using the “shaver” apparatus. This device allows you to scrape out polypous growths from the sinus, preventing the need for a full-fledged maxillary sinusotomy in a hospital setting. During this operation, the anastomosis is also widened, which will improve the outflow from the sinus (this will significantly reduce the risk of new exacerbations of chronic sinusitis). The operation is performed under general anesthesia.
2) Radical maxillary sinus - radical maxillary sinus is indicated when most of the mucous membrane of the maxillary sinus is affected (with irreversible changes). If endoscopic maxillary sinusotomy is done through the nose and is a fairly mild procedure, then radical maxillary sinusotomy requires making an incision in the oral cavity and creating a “window” in the bone tissue in the projection of the roots of the 5-6-7 teeth. Through this window, the irreversibly altered mucous membrane is removed, polyps are scraped out, and foreign bodies (tooth fragments or filling material) are removed.
At the same time, reversible edematous-infiltrative changes in the sinus mucosa are not an indication for its radical removal. Those. in case of chronic catarrhal sinusitis, of course, there is no need to perform a radical maxillary sinusitis. In general, nowadays, with the advent of the possibility of performing endoscopic operations using a shaver, the need for radical maxillary sinusotomy has become significantly lower. But this radical technique is really necessary in difficult situations, for example, when chronic sinusitis is observed against the background of an oroantral communication (fistula between the sinus and the oral cavity).
Operation stages
Complex treatment is carried out in 1 day, we strive to combine all activities in one visit
- Preparation The operation is performed only after professional hygiene and sanitation of the oral cavity, and re-treatment of compromised dental roots. Sterility ensures there is no risk of infection.
- Removal Surgery according to the selected protocol for accessing the sinus with putting the patient to sleep with the simultaneous administration of an analgesic. Performed in a sterile operating room.
- Control X-ray examination CT after surgery is mandatory - to assess the quality of the operation performed and the condition of the maxillary sinus.
If a tooth with an inflamed root was removed, which provoked the growth of a polyp, after the operation the orthopedist will install a temporary orthopedic structure. You will never leave our Center without teeth.
On days 10-14, the sutures are removed and a control CT scan is performed. The patient is invited for a preventive examination and a convenient date for the visit is agreed upon.
Treatment of sinusitis (case study) –
A 28-year-old patient came to the medical center with symptoms of unilateral acute purulent maxillary sinusitis (Fig. 15-16). A CT scan revealed that the sinus was half filled with pus. The treatment that was prescribed was punctures and rinsing of the sinuses with antiseptics and massive antibiotic therapy. As a result, for the next 3 years the patient regularly visited this clinic with symptoms of exacerbation of chronic sinusitis, and she was given the same therapy.
During this time, the attending physician never referred the patient to a dentist to determine how well the root canals in teeth 5-6-7 on this side were filled. Moreover, during this time the patient had CT images taken outside the exacerbation period. When the patient comes to me for a consultation, the image taken outside the exacerbation period shows a rounded formation up to 1 cm in size in the area of the bottom of the maxillary sinus, which is not typical for the topography of the sinus (Fig. 17). The preliminary diagnosis is a cyst of the maxillary sinus on the right (in the picture the right sinus is shown on the left).
Own cysts of the sinus mucosa are extremely rare, and practically the only reason for their formation is inflammation in the area of the apex of the roots of one of the 5-6-7 upper teeth. In addition, the CT scan clearly showed that the apices of the roots are located directly under the mucous membrane of the sinus, i.e. There is no layer of bone between the tips of the roots and the bottom of the sinus. As a result, I refer the patient for a “diagnostic maxillary sinusoscopy,” which involves the use of a thin flexible probe with a video camera and light. As a result, we see a cyst filled with pus (Fig. 18). The cyst was located in the projection of 5-6 teeth and we were unable to accurately determine the causative tooth (including because the root canals of all 5-6-7 teeth on this side were poorly sealed).
As a result, the patient was initially referred for an endoscopic maxillary sinusotomy using a shaver (through the nose), a technique used to curettage and remove polyps and cysts in the sinus. During the operation, the patient also had the anastomosis between the maxillary sinus and the nasal cavity widened. 1 month after the operation and repeated diagnostic maxillary sinusoscopy, the patient was sent for retreatment of 5-6-7 teeth (including sanitation of the root canals using preparations based on calcium hydroxide). As a result, the patient is happy and satisfied.
Important: as an oral and maxillofacial surgeon, I sincerely recommend that (if the ENT doctor himself does not consider it necessary to refer you for a CT scan of your teeth, as well as for a consultation with a dentist), you independently consult a dentist-therapist for a consultation. So that a thorough examination of each root canal in the area of 5-6-7-8 teeth is carried out. Unfortunately, ENT doctors make a lot of mistakes in diagnosing the odontogenic nature of the origin of sinusitis, i.e. when it is related to teeth.
Factors predisposing to the development of sinusitis –
We have already said that each maxillary sinus communicates with the nasal passages through a special anastomosis (opening). This hole is necessary for the outflow of mucous secretions accumulating in the sinus, as well as for ventilation of the sinus. Moreover, it should be noted that infection of the maxillary sinuses by pathogenic bacteria of the nasal cavity occurs precisely through these anastomosis (and regularly), but in most people this does not end with the development of sinusitis. And there are reasons for this.
Normally, bacteria that enter the sinuses are removed from the sinuses (along with mucus) through the same anastomosis, which occurs due to the movement of the cilia of the ciliated epithelium - the uppermost layer of the mucous membrane of the sinuses. Thanks to this cleansing mechanism, the number of pathogenic bacteria is almost always below a critical level, which would necessarily lead to the development of sinusitis. But in some cases, there is a disruption in the evacuation of mucus and bacteria from the sinuses. And let's look at what this is connected with
Sharp swelling of the nasal mucosa due to influenza, ARVI, chronic rhinitis leads to narrowing or complete closure of the anastomosis between the maxillary sinus and the nasal cavity. As a result, mucus and bacteria accumulate in the sinus lumen, and sinus ventilation (aeration) is also disrupted, which very quickly leads to rapid growth of bacteria. In some patients, these anastomosis may initially be too small in size, which, if even slight swelling occurs, immediately leads to disruption of the outflow of secretions from the sinus. And this is the first moment predisposing to the development of sinusitis.
In such patients, ENT doctors can expand the size of the anastomosis, which will significantly reduce the risk of developing sinusitis in the future. The second predisposing point is the insufficiency of the function of the ciliated epithelium, which provides drainage function, clearing the sinus of mucus. All kinds of chronic rhinitis (including allergic), accompanied by prolonged swelling of the mucous membrane, often lead to disruption of the functioning of the cilia of the ciliated epithelium. Well, the third factor predisposing to the development of sinusitis is when there is a combined infection, i.e. both from the side of the nose and from the tops of the roots of the 5-6-7 upper teeth.
Complications of maxillary sinusitis –
Acute purulent sinusitis of the maxillary sinus (or with exacerbation of chronic sinusitis) can be complicated by the development of purulent periostitis of the upper jaw, the formation of an abscess or phlegmon of the orbit, as well as the transition of inflammation to other nasal sinuses, including the cells of the ethmoid labyrinth. In addition to these complications, phlebitis and thrombophlebitis of the veins of the face, as well as the sinuses of the dura mater, can occur, which, along with phlegmon of the orbit, can even lead to death.
As for long-term chronic forms of sinusitis (purulent and polypous forms), the prognosis for them is favorable only with surgical treatment, i.e. when performing endoscopic maxillary sinusotomy using a shaver or radical maxillary sinusotomy in a hospital setting. Long-term chronic sinusitis also leads to impaired immunological reactivity and immune deficiency.
Sources:
1. Higher medical education of the author, 2. Based on personal experience in maxillofacial surgery, 3. “Guide to maxillofacial surgery” (Timofeev A.A.), 4. “Complex treatment of odontogenic maxillary sinusitis” (Shulman F. ), 5. “Clinical recommendations for the diagnosis and treatment of acute rhinosinusitis” (Lopatin A.S., Svistushkin V.M.).
Contraindications
The operations for removing sinus cysts are quite simple. Patients recover quickly after the intervention, and complications are rare. Contraindications are only general for any surgical interventions:
- acute infection;
- diabetes mellitus (severe);
- increased bleeding (blood does not clot well);
- pregnancy;
- epilepsy;
- oncology.
Before surgery to remove a cyst from the sinus, you need to take tests (for HIV, syphilis, hepatitis B and C, general blood test).