An inflammatory formation affecting the upper part of the tooth root is called granuloma. It is formed during the development of periodontitis. Tooth granuloma is tightly attached to the root, being the initial stage of a granular cyst (cystogranuloma), from which it differs, in fact, only in its slightly smaller size. If the formation is ignored and not treated, it will begin to increase.
Tooth granuloma: symptoms of the disease
Only a doctor can make a diagnosis based on an x-ray, where a darkening will be visible in the root area. Any darkening in the image is a sign of the presence of a cavity, but if a granuloma occurs, it means that periodontitis, which is chronic in nature, begins to develop.
For a long time, the tooth may not bother a person at all. Sometimes pain may occur when biting or when eating hot food: these are the first signs of the development of chronic periodontitis. An exacerbation of the disease is observed during periods of weakening of the body's immunity: then the pain intensifies significantly, which is especially noticeable when biting. During such periods, as a rule, the gums become swollen, and in the area of inflammation it becomes painful to touch.
Symptoms
Even having an idea of what dental granuloma is, its symptoms are not so easy to determine. The fact is that the disease may not manifest itself for a long time. The tooth under which the formation is located may not outwardly stand out in the dentition. The gums may also look quite healthy.
In some cases, the disease is accompanied by the following symptoms:
- swelling of facial tissues;
- swelling of the gums;
- slight increase in temperature;
- the occurrence of flux;
- acute pain in the area where the granuloma has formed;
- slight discharge of pus between the tooth and gum;
- pain in the eyes, migraine, dizziness;
- On palpation there is acute pain.
Good to know. Granuloma often makes itself known if a person has had a cold, flu, pneumonia and other diseases that lead to a decrease in immunity.
Why does granuloma appear on the root of a tooth?
At the tops of the roots, such formations can appear for several reasons:
- Poorly performed treatment of pulpitis. If caries is started, the affected cavity gradually becomes quite deep. When microorganisms enter the pulp, its inflammation begins, accompanied by acute pain, which may stop over time, indicating the death of the nerve.
But the development of the disease does not end: bacteria through the root canals extend beyond the boundaries of the affected tooth, as a result of which a focus of inflammation appears near the upper parts of the roots, called periodontitis. The further course of the disease can occur according to several scenarios, one of which is the formation of granuloma.
It is necessary to understand that a tooth with a granuloma does not necessarily have to be affected by caries, since the root can become inflamed near a tooth that has already been treated. If the doctor has not completely removed the tissues affected by caries by placing a filling on top of them, then there is a high risk of developing pulpitis with the subsequent formation of granuloma.
- Filling of root canals performed with violations. A granuloma that appears on the root of a tooth whose canals were filled some time ago indicates the unsatisfactory quality of the procedure performed. Due to inattention, haste or inexperience, the doctor could not fill the canals to the very top. Dentists often refuse to admit their own mistake, because in this case they will have to treat the tooth for free. Such unfortunate specialists can evade until the last minute, pretending that they do not understand the causes of pain, recommending taking a course of antibiotics.
Causes
The main cause of dental granuloma is infection in the periodontal tissue. More often this happens in cases:
- pulpitis (acute or chronic);
- tooth trauma (cracks - entrance gates for infection);
- inflammation of the soft tissue surrounding the tooth (periodontitis);
- poor quality treatment of pulpitis, dental canals.
Other factors that can trigger the development of the chronic stage of granuloma and cause exacerbation: hypothermia, viral diseases, stress, failure of the immune system.
Diagnosis of granuloma on the tooth root
At the early stage of development of the disease, it will not be possible to notice any visual changes. The first signs of pathology become noticeable as the size of the infected area and the amount of pus increase.
To treat the disease with therapeutic methods, it is necessary to examine the affected area in detail: a complete picture of the granuloma must be obtained, which will allow one to detect key signs of the disease that differ from other diseases.
When suppuration occurs, the gums become very red and swollen, and pain appears, which can radiate to the head area in general and the ear in particular. This is the first symptom that should make you wary.
The following methods can be used to make an accurate diagnosis:
- use of classical x-rays;
- the use of radiovisiography or, in simpler terms, computer x-ray.
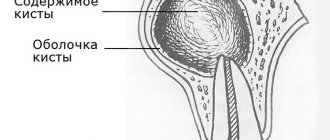
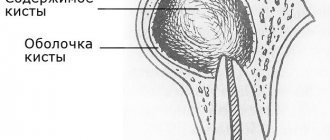
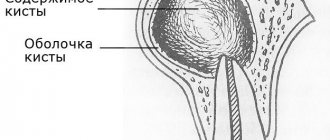
In the picture, the affected area looks like a dark spot with a clear border in the upper part of the tooth. The size of the spot indicates the following:
- 5-8 mm – the probability of having a dental granuloma is high;
- more than 8 mm – formation in the form of a cyst.
In rare cases, a large granuloma, up to 1.2 cm in size, may occur. Therefore, X-rays may not be enough for diagnosis: it is recommended to perform a biopsy of tissue cells from the area affected by the disease.
In most cases, granuloma is discovered during treatment of other dental diseases: the doctor may pay attention to increased swelling and swelling of the gums. In addition, the bone tissue near the top of the tooth may also bulge.
An increased risk of developing granuloma is observed in patients with crowns and pulpless teeth. Such people are advised to undergo regular examinations in order to promptly identify any changes affecting the gums and teeth.
Pyogenic granuloma as an interdisciplinary problem
Pyogenic granulomas can be considered as benign vascular tumors or as reactive vascular changes arising at sites of previous injury or inflammation [1].
Synonyms: botryomycomoma, telangiectatic granuloma, benign pedunculated granuloma, granuloma of pregnancy, lobular capillary hemangioma, eruptive angioma, etc.
The variety of listed synonyms indicates the absence of a common view on the etiopathogenesis of the disease and, as a result, causes significant difficulties in classification, diagnosis, treatment tactics and prognosis of this pathology.
The term “botryomycosis” was proposed by Boullinger, who in 1887 described lung lesions in horses, caused, according to the then assumption, by Botryomyces equina. Ten years later, in 1897, Poncet and Dor first presented patients with what they then believed to be equine botryomycosis. Further research proved the untenability of ideas about the mycotic nature of this disease, however, the term “botryomycoma” is still widely used today.
Different points of view are still expressed about the etiology of pyogenic granuloma. Previously, the disease was regarded as vegetative pyoderma; it is now considered a type of angiomas, developing as a reactive process at the site of microtrauma in the form of a vascular node with profiling capillaries, resembling granulation tissue. Since this formation is essentially neither infectious nor granulomatous, its most accurate name is “lobular capillary hemangioma” [2].
Most often, pyogenic granuloma is observed in young people and adolescents, as well as during pregnancy (in 5% of all pregnancies). Pyogenic granuloma has been reported in the gastrointestinal tract, larynx, nasal mucosa, conjunctiva and cornea [3].
Trauma (including microtrauma), pregnancy, infectious diseases or previous dermatosis are suggested as provoking factors. However, a history of trauma is noted in only 25% of cases.
Cases of the occurrence of multiple pyogenic granulomas on burn surfaces have been described after taking oral contraceptives, protease inhibitors and acne treatment with isotretinoin. It is known that pyogenic granulomas regress after pregnancy. In one study, an increased concentration of vascular endothelial growth factor was found in pyogenic granulomas during pregnancy; after childbirth, the content of this factor was practically not determined; apoptosis of endothelial cells and regression of the granuloma were noted [4].
Clinically, pyogenic granuloma is a soft or densely elastic, painless tumor-like formation on a stalk, 0.5–2.0 cm in diameter, dark red in color, with a smooth or lobulated surface. The stalk, surrounded by a “collar” of exfoliated epithelium, can be of varying length and sometimes gives the tumor a mushroom-like appearance. Appearing several weeks or months later at the site of injury (cut, burn, injection, abrasion, etc.), the granuloma quickly grows, darkens (may become cyanotic), and thickens. Its surface, initially moist, vascular (like a raspberry), erodes, becomes crusty, and bleeds easily with minimal trauma. Often a secondary infection occurs, ulcerations form (sometimes occupying the entire surface of the tumor), necrosis, and bloody-purulent discharge. Palpation is usually painless. More often it is presented by a solitary focus (multiple tumors are rare, but are sometimes observed after extensive burn injuries). Most often it is localized on the hands (especially on the fingers), feet, face, but can also be located on other areas of the skin - on the trunk, genitals, in the perianal area, along the edge of the eyelids and on the tongue. According to observations, in approximately half of cases, pyogenic granuloma is found at the site of an ingrown nail and is one of the most common complications of this pathology [5].
Giant granulomas, with a diameter of 3.0–5.0 cm or more, are traditionally considered a rare phenomenon, but in practice they are detected quite often. According to observations, they periodically occur in bedridden patients at the site of bedsores.
The course of pyogenic granuloma is characterized by rapid growth, the presence of a stabilization phase of the process, and complications in the form of a secondary infection with all the ensuing consequences. This tumor is not characterized by spontaneous regression, but it is not prone to dissemination and malignancy.
Differential diagnosis is usually not difficult. It is carried out with vegetative pyoderma, melanoma, Kaposi's sarcoma, angiosarcoma, glomus tumor, keratoacanthoma, spinous cell epithelioma.
To prevent bleeding and exclude malignancy, removal of the lesion is recommended [6].
Pyogenic granulomas are removed using tangential excision and electrodesiccation; in the latter case, the number of relapses is noticeably lower. During manipulation and excision, the lesions bleed heavily. Lidocaine with epinephrine must be used (with a ten-minute delay of manipulation - the effect of epinephrine), electrocoagulation is used for hemostasis. The focus of pyogenic granuloma, cut off with a scalpel blade, is sent for histological examination. Then curettage of the base of the lesion is performed, which helps stop bleeding and prevent relapse. Curettage and electrodesiccation of the base are carried out until bleeding stops.
There are reports of the effectiveness of cryo- and laser therapy.
We present a clinical case of a patient with pyogenic granuloma.
The patient, born in 1987, complained of a painless formation on the skin of the right hand, bleeding in the area of the rash. She was ill for about 2 weeks when the above complaints first appeared without a clear causal connection. Denies the fact of skin trauma. I did not contact a dermatovenerologist and did not treat myself. Education progressively increased in size.
Life history: tuberculosis, helminthic infestations, viral hepatitis, denies sexually transmitted diseases in the past. Current chronic diseases: denies. Operations, injuries: denies. Allergy history: not burdened. Currently, she is being seen by an obstetrician-gynecologist for pregnancy at 30 weeks.
Objectively: general condition is satisfactory. Position: active. Body temperature 36.7 °C. Upon examination, no pathology was found in the internal organs and systems.
Local status: the pathological skin process is limited in nature, localized on the skin of the palmar surface of the third finger of the right hand. It is represented by a bright red node up to 1.0 cm in diameter, along the periphery there is a rim of exfoliated epidermis, the phalanx of the finger is slightly swollen. On palpation, the formation is soft-elastic, heterogeneous, immobile, painless. Peripheral lymph nodes are not enlarged. Dermographism is mixed. There are no other pathological rashes on the skin or visible mucous membranes (Fig. 1).
During the examination: general blood test, general urinalysis, biochemical blood test - without pathology. Examination for hepatitis HBsAg - not detected. ELISA for antibodies to HIV - negative.
On dermoscopic examination, the formation was of a non-melanocytic nature; Large vascular lacunae of pink-red color and superficial ulceration are visualized.
Considering the bleeding of the formation, progressive increase in size, and state of pregnancy, the patient was referred to a surgeon for excision. Within a week, she was consulted by three surgeons from different health care facilities in Surgut, who doubted the correctness of the diagnosis. There were suggestions of “cancer”, “wart”, etc. A 2-week observation was recommended. During the observation period, the formation slightly increased in size. At the next visit, the surgeon performed outpatient excision of the pyogenic granuloma and treatment with antiseptic solutions (Fig. 2). When examined after 10 days, active epithelization was noted in the lesion and the absence of new rashes (Fig. 3).
Conclusion. Pyogenic granuloma, due to the lack of uniform approaches to treatment, is an interdisciplinary problem and presents certain difficulties for diagnosis among doctors of different specialties. It is advisable to conduct a preliminary dermoscopic examination for the purpose of differential diagnosis with malignant neoplasms of the skin and its appendages.
Literature
- Domanin A. A., Solovyova O. N. Calculation of the diagnostic significance of the morphological signs of pyogenic granuloma and capillary hemangioma. In the book: Treatment-diagnostic, morphofunctional and humanitarian aspects of medicine. Tver, 2011. pp. 57–59.
- Aladin A. S., Yaitsev S. V., Korolev V. N. A case of pyogenic granuloma of the anterior surface of the neck, simulating a malignant tumor (clinical observation) // Tumors of the head and neck. 2011. No. 2. pp. 49–54.
- Novoselov V. S., Gostroverkhova I. P., Novoselova N. V. Clinical cases from the practice of a dermatologist // Russian Medical Journal. 2008. No. 23. P. 1559.
- Skripkin Yu. K. Skin and venereal diseases. M.: Triada-Farm, 2005. 168 p.
- Hebif T.P. Skin diseases: diagnosis and treatment / Trans. from English V. P. Adaskevich; edited by A. A. Kubanova. 4th ed. M.: MEDpress-inform, 2021. 700 p.
- Bogatov V.V., Zemlyakova L.I. Use of a laser scalpel in the treatment of pyogenic granulomas of the maxillofacial region // Bulletin of the Smolensk Medical Academy. 2010. No. 2. pp. 30–32.
E. N. Efanova*, 1, Candidate of Medical Sciences Yu. E. Rusak*, Doctor of Medical Sciences, Professor E. A. Vasilyeva* I. N. Lakomova** R. R. Keldasova*
* BU VO KHMAO-Yugra Surgut State University, Surgut ** BU KHMAO-Yugra Surgut KKVD, Surgut
1 Contact information
Tooth granuloma: treatment
Usually treatment is only therapeutic in nature, but its strategy may vary depending on whether the canals have been filled before.
- If the canals have not been filled, the tissues affected by caries are drilled out, and the old filling is removed. This is required to carry out high-quality mechanical treatment of the canals, which are expanded and treated with antiseptic agents. If the granuloma is small (formations up to 3 mm are considered such), then the canal is sealed immediately. If the size of the granuloma exceeds 3 mm, the treatment period increases, since it is necessary to put a medicine into the canal, which includes potassium hydroxide - this substance leads to a decrease in the granuloma or even to its complete disappearance. A temporary filling is placed for the period the medication is placed (approximately 2-3 weeks). Then a repeat x-ray is taken, which should clearly show a significant reduction in the inflammatory formation. If the dynamics are obvious, the canals are sealed and a permanent filling is placed.
- If the canals have been filled, then the first stage of treatment is their unsealing. The further sequence of actions is similar to that described in the previous paragraph. The only thing is that if there is a crown on the tooth, it will have to be removed, and after the treatment is completed, it will have to be made and placed again. Some patients do not want to spend money on re-installing a crown: the solution is to perform a root resection operation, when the upper part with the granuloma attached to it is cut off through a small incision in the gum.
Treatment options for granuloma
Treatment of the tumor consists of eliminating the source of infection and preventing relapse. Therapeutic and surgical techniques are used.
Therapeutic method
It will bring results only if the disease is detected at an early stage. The patient is prescribed antibiotics and sulfonamide medications. Timely treatment will help eliminate the infection and save the damaged tooth.
Non-surgical method
It appeared relatively recently, the essence of the method is as follows: the affected tooth canal is expanded and a substance is introduced into it that destroys the infection.
Surgical method
It is used if the granuloma has grown greatly and the use of drug therapy will be ineffective. During the operation, the dentist cuts the gum to allow pus to come out. Then a drainage is installed in the tooth, which the patient must endure for three days. Also during this period, drug therapy is carried out. After three days, another operation is performed, during which purulent sacs, tumors, or a tooth root with a cyst are removed. Then the doctor makes a decision about the fate of the tooth: it is either left or removed.
Removal is necessary in the following cases:
- the tooth is so damaged that it can no longer be restored;
- root canals cannot be treated;
- the cause of inflammation was problems in the periodontal pocket;
- the patient is undergoing a prosthetic procedure;
- cracks have formed in the area of the tooth or its root;
- There are multiple perforations of the tooth.
In other cases, doctors try to save the tooth.
Granuloma between tooth roots: treatment with antibiotics
The number of people putting off visiting a doctor until the last minute is large. There are many reasons for this: fear of pain (although modern means of anesthesia make it possible for the patient to feel nothing at all during treatment procedures), lack of free time, and reluctance to part with money. But all these reasons and excuses come to naught when the pain becomes unbearable, becoming chronic. As practice shows, as soon as a person does not sleep for a couple of nights, the issue of the need to visit the dentist is resolved by itself.
However, many people try to cure granuloma on their own using strong antibiotics, which is basically impossible. Antibiotics may be prescribed to relieve inflammation and stop the formation of pus, but nothing more. But the action of antibiotics may not affect pathogenic microorganisms located in the root canals, and it is the infection in their unsealed areas that is the only reason for the formation of granulomas.
If a patient comes to the doctor with a suspicion of granuloma, and the doctor, driven by some of his own considerations, does nothing, recommending taking antibiotics, it is better not to delay time, but to immediately contact another dentist. Some doctors simply do not like to re-treat someone’s poorly treated teeth, since repeating the same operations takes much more time, while others, if the patient comes back again, do not want to admit that they made a mistake, which for them is tantamount to realizing their own lack of competence.
How to cure granuloma in a child
The causes of granuloma annulare in children are unknown. Scientists believe that type 4 cellular immune reactions and pathologies of tissue monocytes are involved in the formation of the disease. Sometimes clinical manifestations of the disease are observed after prolonged sun exposure, insect bites, injuries, or vaccinations.
The development of granuloma annulare is a benign process characterized by the formation of nodules or papules that form a kind of ring around areas of unchanged skin. Rashes of yellowish-brown, flesh-colored or bluish color are located in the form of single or multiple lesions. Typical localization is the dorsum of the hands and feet. The lesions can merge, forming rings.
Children often experience spontaneous regression of rashes. If the process is widespread or the rash bothers you (itching, pain), treatment is prescribed. Granuloma in a child can be cured using ointments with corticosteroids and intralesional administration of hormonal drugs. PUVA therapy and pulsed laser are also successfully used.
Tooth granuloma: surgical treatment
If therapeutic treatment does not help, then surgery comes into play: the operation is performed in the presence of a destructive process affecting the gums, and anesthesia (both general and local) is used to carry it out.
There are several surgical treatment options.
Root resection
Elimination of granuloma occurs in several stages:
- a passage to the top of the tooth opens by peeling off the gum shell;
- the root canals are cleaned and subsequently filled with medicinal substances;
- excision of the granuloma is carried out;
- the area is filled with synthetic fabrics;
- the tooth is filled.
On average, the operation takes about an hour.
Hemisection
If a tooth has many roots, then this procedure is prescribed (if there are complications that prevent the root from being saved).
The treatment procedure includes:
- removal of roots under the crown;
- filling the empty space between the roots with a special dental product;
- installation of a crown;
- monitoring the condition of the tooth using x-rays.
The method is simple, while the functionality of the tooth is preserved. If necessary, some time after the procedure, the patient can resort to prosthetics, provided that the root system remains healthy.
Cystotomy
The method is used when removal of large granulomas is required.
To implement it:
- a channel is created between the affected area and the oral cavity, through which pus absorbed by tampons is removed;
- after cleaning, the cavity is treated with antibacterial agents;
- sutures are placed;
- the cavity, free from suppuration, is filled with bone cells.
Eosinophilic granuloma
This term denotes a pathology of unknown etiology, characterized by intense proliferation of reticulohistiocytic elements with the formation of infiltrates in the bones.
The bones usually affected are:
- pelvis;
- skulls;
- spine.
The disease develops slowly. The first symptoms of eosinophilic granuloma are swelling and pain in the affected area. In the future, spontaneous fractures are possible.
In children, there are cases of spontaneous stabilization and regression of the process (up to complete recovery). If it is necessary to treat granulomas, glucocorticosteroids are prescribed (locally and/or parenterally) and PUVA therapy is performed.
Measures to prevent granuloma after an extracted tooth
Preventive measures are aimed at preventing the development of the disease. They include:
- high-quality cleaning of teeth and gums on a daily basis;
- timely treatment of bleeding gums;
- regular visits to the dentist at least once a year (it is better to do this twice);
- replacing toothbrushes (old brushes accumulate bacteria that can provoke the development of the disease);
- contacting the dentist at the slightest pain associated with the gums or teeth;
- treatment of caries, periodontitis and pulpitis - quite often these diseases are the catalyst for the development of granuloma;
- the use of medicated toothpastes and herbal decoctions for rinsing;
- eating foods rich in calcium and other trace elements.
Features of prevention
The main condition for the prevention of dental granulomas is timely assistance from a dentist when caries occurs. You should not allow severe tooth decay or the development of pulpitis. The peri-root tissues are healthy until the pulp becomes inflamed. Therefore, if symptoms of caries or pulpitis appear, it is important to immediately consult a doctor.
Endodontic treatment also increases the likelihood of developing periodontitis. Therefore, it is better to eliminate caries in the early stages and avoid the need for root canal filling. If this is unavoidable, it is important to carefully choose a dental clinic - the professionalism of a specialist will help eliminate possible mistakes and prevent complications.
Complications after granuloma at the site of an extracted tooth
Lack of timely treatment and hope that the disease will go away on its own is fraught with serious consequences. Among the most common complications it is worth highlighting:
- development of periodontitis and further formation of a fistula;
- the occurrence of alveolitis is a consequence of the presence of an inflammatory process;
- formation of purulent flux;
- suppuration of the perimaxillary tissue;
- entry of pathogenic bacteria into the lymph nodes, from where they penetrate the cardiac system and internal organs (kidneys, liver and brain);
- development of facial asymmetry;
- the emergence of new foci of infection;
- infection of the body due to the penetration of pathogenic microorganisms into the blood vessels.
Timely removal of granuloma is a guarantee to avoid unpleasant health consequences.