Causes of the disease
A number of factors can provoke the manifestation of the disease, which include various influences from the outside world. Any patient can encounter this, even with good oral hygiene.
Main causes of the disease:
- pathogenic microorganisms that have entered the patient’s oral cavity;
- some viral diseases;
- toxic substances contained in food.
Another reason for the formation of salivary gland adenoma is considered to be an addiction to smoking tobacco. Smoke that enters the body contains many carcinogens that damage the glandular epithelium of the salivary glands. As a result, protective mechanisms are activated, which provokes increased cell division, resulting in the formation of an adenoma.
Middle ear hemangioma
Benign tumors of the middle ear also include hemangioma and various neurogenic neoplasms. Hemangiomas of the middle ear are manifested by the following symptoms:
- Decreased hearing;
- Ear congestion;
- Feeling of noise.
Often the first symptom of the disease is a slowly occurring paralysis of the facial muscles on the side where the hemangioma is located. For middle ear hemangioma, otolaryngologists usually perform abdominal surgery or widely remove the mastoid process.
Types of salivary gland adenoma
Adenoma is characterized by slow growth, so the patient may not even be aware of the existence of this disease in his body for decades. Many people discover the presence of the disease only when undergoing examinations for other problems, or during a routine examination. Rapid tumor growth indicates its malignant degeneration.
Classification:
- Polymorphic or pleomorphic . It is a dense encapsulated node containing light fluid, lymphoid cells and fibroblasts.
- Basal cell . It is a small, clearly demarcated node, the structure is dense, uniform, grayish-whitish or brownish in color. May be multiple.
- Canalicular . It is distinguished by the content of prismatic epithelial cells, which are collected in thin bundles.
- Greasy. This is a clearly demarcated tumor formed from different shapes and sizes of sebaceous cells, with cystic changes. The surface has a grayish-whitish or yellow color. There is no danger of relapse.
- Adenolymphoma . The tumor is mobile, contains lymph, is benign, and consists of glandular epithelial structures.
- Monoform. It consists of large cells with eosinophilic granular cytoplasm and a small dark nucleus, and is light in color.
- Adenocarcinoma . A malignant epithelial tumor develops in the large and small salivary glands, has proliferation of the epithelium in ductal formations in the form of papillary, cribriform, tubular structures. The prognosis is unfavorable.
The most common type of salivary gland adenoma by location is the parotid. Adenomas of the submandibular glands, small glands and sublingual glands are also isolated. Regardless of the location of the tumor, the only way to treat the disease is to remove the adenoma.
Diagnosis of adenomas
Diagnosis is made using:
- biopsy of a tissue sample – allows you to determine the type of neoplasm;
- CT and/or ultrasound, including transrectal TRUS, help determine the exact size and location of the tumor;
- Clinical blood and urine tests allow you to assess the overall picture and identify foci of inflammation.
Prostate adenoma is detected using digital examination, radiography and contrast urography, cystometry of the bladder and uroflowmetry of the urinary tract, determination of the level of the prostate-specific hormone PSA and a biochemical blood test. Palpation and mammography are also used to diagnose breast adenoma.
Treatment
Removal of a salivary gland adenoma is a simple surgical operation; the prognosis for treatment in most cases is favorable. The only difficulty that can be encountered during treatment is damage to the facial nerve. However, a solution has been found for this problem.
To gain access to the tumor, the surgeon dissects the facial nerve by carefully lifting it upward. Only after this the tumor is removed. Removal of the node is carried out within a few minutes in the maxillofacial departments of dental clinics. If the results of histological analysis of the tissues of the removed tumor confirm its benign nature, no additional treatment will be required.
The parotid salivary gland (PS) is the largest SG. Its main part is located in the parotid-masticatory region of the face, directly under the skin on the outer surface of the branch of the lower jaw, the smaller part is in the retromandibular fossa.
GS tumors account for 5% of the structure of cancer incidence, with up to 80% of tumors affecting large GS [5]. A separate group consists of tumors localized in the pharyngeal process of the parotid gland. They account for <20% of all GC tumors and 0.5% of head and neck tumors [4]. In most cases, these neoplasms are benign; among them, pleomorphic (polymorphic) adenomas prevail (up to 80-90%) [1]. The frequency of their malignancy is from 3.6 to 30% [2].
The generally accepted method of treating patients with pleomorphic adenomas is surgery [3]. The prognosis after an adequately performed operation is usually favorable. The relapse rate is up to 8.0%. They arise mainly due to non-radical surgery or other factors that are not fully understood. In this case, a significant role is played by hormonal and metabolic disorders [3].
In the Department of Head and Neck Tumors of the Russian Scientific Research Institute for a 5-year period (2009-2013), 5192 patients with tumors of the head and neck were observed, including tumors of the pharyngeal process of the parotid gland - 5 people (1.5%), of the number of patients with tumors SG and 0.01% - with tumors of the head and neck). Of these 5 patients, 4 tumors of the pharyngeal process were initially located in the parapharyngeal space, and only 1 had a multicentric tumor. We present a clinical observation of this patient.
Patient C
., 23 years old, medical history No. C-437/g. He was admitted to the Department of Head and Neck Tumors of the Russian Scientific Research Institute with a diagnosis of a tumor of the pharyngeal process of the right parotid gland. Complaints of discomfort in the oral cavity, difficulty chewing and swallowing food, altered speech.
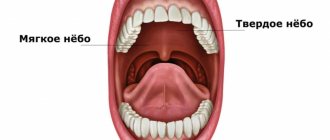
Examination of the oral cavity revealed asymmetry of the soft palate due to bulging of the right parapharyngeal space, where a neoplasm with pulsation at its superomedial edge was manually identified.
Ill for about 10 years. In 2004, and then in 2006, tumors of the parotid gland were removed in the children's department of the Russian Scientific Research Institute. According to pathohistological examination, in both cases a pleomorphic adenoma was identified (No. 26816-26817). In 2008, a relapse occurred. He was hospitalized in the department of head and neck tumors of the Russian Scientific Research Institute, where a subtotal, in the plane of the branches of the facial nerve, parotidectomy was performed with removal of the tumor located in the superficial part of the SG (Fig. 1 and 2, see color inset)
Rice. 1. According to CT data, a tumor of 53×62×60 mm, lobular in nature, of hypointense density, deforming the pharynx, is determined on the left in the parapharyngeal region.
Rice. 2. The parapharyngeal tumor was radically removed from the submandibular approach. . Conclusion: pleomorphic adenoma (No. 72483-488/08). In 2010, there was a relapse again. In this case, the tumor was located above the angle of the lower jaw, i.e. at a distance of up to 2.5 cm from the place of its first localization. There were enlarged cervical lymph nodes on the same side. A parotidectomy was performed along with the tumor, including fragments of the masticatory muscles. At the same time, lymph node dissection was carried out in the volume of IIA-B, III levels. Pathohistological examination again confirmed a pleomorphic adenoma. No oncopathology was detected in the lymph nodes of the neck.
In 2012, there was a new relapse: in the projection of the zygomatic process. The tumor was removed down to the bone. Pathohistological conclusion: pleomorphic adenoma.
It should be noted that all operations performed were performed by surgeons with 30-35 years of experience working with this category of patients. In all cases, the integrity of the branches of the facial nerve was preserved. During each hospitalization, the patient underwent a full clinical and laboratory examination, and was examined by a dentist and an ENT doctor.
At the end of 2013 (1 year after the last operation, and there were 5 of them), the patient again turned to the RNIO with a diagnosis of “tumor of the pharyngeal process of the parotid salivary gland.” Computed tomography (CT) confirmed the presence of a neoplasm in the parapharyngeal space on the right (Fig. 3 and 4)
.
Rice. 3. MRI of the parotid region. The tumor occupies the entire pterygopalatine fossa, deforming the nasopharynx with the involvement of the maxillary artery and vein, displacing the internal carotid artery and vein posteriorly.
Rice. 4. CT scan of the skull. On the right, in the parapharyngeal region, a lobular tumor is identified, deforming the nasopharynx and parotid region without signs of germination. A puncture biopsy revealed a pleomorphic adenoma. The question arose about the operation. The possibility of resection was determined by the condition of the internal carotid artery (ICA). Magnetic resonance imaging (MRI) was performed with contrast enhancement of the vessels of the parotid region, pharynx and neck (Fig. 5)
.
Rice. 5. MRI with contrast examination of the vessels of the parotid region, pharynx and neck. The vascular structures of the neck are clearly visualized. There are no signs of invasion of the tumor process into the internal, external, common carotid arteries and jugular vein. All major vessels were pushed aside without signs of tumor growth in them.
The study revealed no involvement of the ICA in the tumor process. The patient and his relatives consented to the operation.
The operation was performed under endotracheal anesthesia with intubation through a previously applied tracheostomy. A skin incision was made in the submandibular region from the anterior edge of the sternocleidomastoid muscle to the anterior belly of the digastric muscle. The external carotid artery above the lingual artery was isolated and ligated. The parapharyngeal space was opened layer by layer. The tumor is separated from the pharynx, base of the skull and other surrounding tissues using blunt force, manually and with a rasp. The pulsation of the ICA was manually determined superiorly and medially from the vaguely palpable apex of the tumor. The lower part of the tumor is dislocated into the wound (Fig. 6, see color insert)
.
Rice. 6. The lower edge of the tumor of the pharyngeal process of the parotid salivary gland is isolated into the wound.
Rice.
7. Tumor of the pharyngeal process of the parotid salivary gland, removed in fragments. The marginal branch of the facial nerve was traced. It was not possible to isolate the entire tumor at once. Removal was carried out by cutting tumor fragments (Fig. 7, see color insert). Manual revision of the operating cavity made it possible to think about complete removal of the tumor. A drainage is inserted into the cavity of the surgical wound. Pathohistological examination of the gross specimen again established a pleomorphic adenoma (No. 1997-2003/14). The postoperative period proceeded without complications. The wound healed by primary intention. There are no complaints upon discharge. Speech and swallowing are normal. The symmetry of the soft palate was restored. A visual examination after 2.5 months did not reveal any pathology. However, MRI data revealed continued growth of the tumor, spreading into the right pterygoid fossa, enveloping the ICA and growing into the ramus of the mandible.
Although a review of the pathohistological studies after all operations confirmed the diagnosis of pleomorphic adenoma, taking into account the duration of the anamnesis and the frequency of recurrence, this situation was assessed as a possibility of malignancy. A consultation was held with the participation of radiation therapists; It was decided to carry out radiation therapy. The patient tolerated radiation at a dose of 40 Gy satisfactorily. Control MRI showed a reduction in the tumor process, and therefore irradiation was continued to a therapeutic dose of 60 Gy.
Monthly examination confirmed remission. During external examination and manual examination of the oral cavity, no pathology was detected. The patient refused a follow-up MRI. He is under observation in a state of remission for 8 months.
Pleomophic adenomas of the parotid gland may have multiple primary buds. Their malignancy is characterized by a long period (up to several years). The longer pleomorphic adenomas exist, the greater the chance of their malignancy [3]. Localization of pleomorphic adenoma in the pharyngeal process of the gland is rarely observed. There are very few publications on this topic. In the presented material, due to the fact that pathohistological examination revealed a pleomorphic adenoma, it was difficult to carry out adequate treatment. In similar cases, the diagnosis should be made on the basis of clinical and morphological data, and preference should be given to clinical data.
Retrospectively assessing this case, it should be concluded that, probably, after the 3rd relapse it would be necessary to change the tactics of patient management with a transition to combined treatment (surgery and radiation therapy). The observation once again confirms the validity of the thesis about the dominant role of the clinic in making a diagnosis and developing treatment tactics.
Complications
Despite the fact that treatment of salivary gland adenoma does not pose a serious problem, it is important to remember that untimely removal of the tumor can lead to a number of complications. The most serious of them is the transformation of a benign neoplasm into a malignant one. Unlike malignant tumors, salivary gland adenoma can exist asymptomatically, only in some cases causing facial asymmetry. Therefore, if you detect the slightest swelling, you must immediately consult a doctor. Timely removal of the tumor will prevent many very unpleasant problems.
The most common postoperative complications:
- the risk of developing Frey's syndrome (occurs when autonomic nerve fibers are damaged, accompanied by redness and sweating of the operated area of the face);
- a feeling of dry mouth when the gland is completely removed.
Observation and regular consultations with a doctor can reduce all postoperative complications to a minimum.
Polyp in the ear
Benign tumors of the ear include polyps. They arise as a result of the proliferation of granulation tissue. The polyp may be located in the external auditory canal or middle ear. Neoplasms localized in the ears can spread to other parts of the skull.
Most often, a polyp is a complication of a chronic inflammatory process in the ear. At the site of chronic inflammation of the mucous membrane, gradual tissue proliferation occurs, replacing normal connective tissue. When the pathological process is localized in the middle ear, the formation may remain invisible to conventional otoscopy for a long time. As the polyp grows, it “falls out” into the external auditory canal through the perforation of the eardrum.
A polyp in the ear is manifested by the following symptoms:
- Suppuration, sometimes mixed with blood (stopping the flow of pus can be caused by blockage of the ear canal by a polyp);
- Itching, noise and pain in the ear;
- A feeling of constriction, the presence of a foreign body in the ear cavity;
- Decreased or loss of hearing;
- Headaches.
In the absence of adequate treatment, a polyp caused by an infection in the ear often becomes the cause of chronic otitis media, supports the inflammatory process and prevents the penetration of drugs to the site of infection. The growth of the polyp leads to blockage of the ear canal and deafness. Under certain conditions, there is a risk of its degeneration into a malignant tumor.
For polyps of small size, in some cases, otolaryngologists carry out conservative treatment with creams containing glucocorticoids and antibacterial drops. If the disease is fungal in nature, antifungal drugs are used. However, the main treatment for a polyp in the ear is surgery.
The polyp is cut off on an outpatient basis with a special loop or using another instrument: a curette, an ear conchotome. Radical surgery is performed in a hospital. The operation is performed if the fistula is localized in the semicircular canal. An alternative treatment option is laser removal of polyps. A modern method of treating a polyp in the ear is OTO NUS therapy in combination with endoural LILI (exposure to the pathological focus with low-frequency ultrasound through various medicinal solutions).
Make an appointment
Causes and types of ear cancer
Malignant neoplasms in the ear area occur against the background of pathological processes called precancerous. The morphological structure of malignant tumors of the external ear is diverse. In 61% of cases, morphologists identify epithelial cancer, 38% - glandular cancer.
In the external auditory canal, basal cell carcinoma is 2-3 times less common than squamous cell carcinoma. Squamous cell carcinoma with varying degrees of keratinization predominates. The initial localization of malignant neoplasms of the auricle is the posterior surface, the area of the postauricular fold and the earlobe.
The primary tumor of the external auditory canal occurs on one of its walls. The pathological process predominantly develops in the area of the lower and posterior walls of the ear canal. Ear cancer can also develop on scars. A tumor behind the ear can also be cancerous.
Make an appointment
Tumors of the external ear
Malignant neoplasms of the external ear are represented by the following tumors:
- Squamous cell carcinoma;
- Basal cell carcinoma;
- Adenocarcinoma from ceruminoma;
- Adenoid cystic carcinoma.
Oncologists detect the following soft tissue tumors in the ear and jaw area:
- Hemangioma;
- Neurofibroma;
- Neurilemmoma (schwannoma).
Fibrosarcoma or rhabdomyosarcoma can develop in and around the ear. Papillomas most often occur on the skin of the auricle. If the neoplasms are located in the external auditory canal, they often fill its lumen, resembling polyps that come from the middle ear. Ceruminoma of the external auditory canal is a very rare and long-growing tumor arising from the sebaceous (sulfur) glands.
Ceruminoma is usually observed in people over 20 years of age. With this type of ear cancer, the symptoms are as follows:
- Ear congestion;
- Hearing loss;
- Pain and discharge from the ear.
In the initial stage, the tumor is located on the wall of the external auditory canal. The tumor is pink. As it grows, it fills the ear canal and looks like a polyp. Radiologically, good pneumatization of the mastoid process is determined. Gradually, the tumor spreads to the middle ear and its walls, destroying them. These changes are determined on radiographs.
Mixed tumors of the external auditory canal are secondary. They most often originate from the parotid gland and penetrate the external auditory canal.
Nevi (benign pigmented tumors of the auricle and external auditory canal) do not differ in clinical course from nevi that are located on other areas of the skin. Soft tissue tumors (fibroma, hemangioma) arise from fibrous, fatty, muscle, vascular and other tissues.
Fibroma is most often located on the earlobe, at the sites of puncture with a needle for wearing earrings. Dimensions vary from 5 mm to 4 cm. Less commonly, the tumor is localized at the ascending branch of the helix of the auricle and at the entrance to the external auditory canal.
Hemangiomas develop in all parts of the ear. Capillary and cavernous forms of vascular tumors are more often observed. The first ones very often disappear in childhood. Cavernous hemangiomas are located in the thickness of the auricle. They occur in the form of individual or multiple neoplasms. They have a soft consistency and a bluish tint. Hemangiomas of the auricle can affect its edge and other parts. They often spread towards the external auditory canal, closing its lumen, and bleed when injured.
Chemodectoma
Chemodectoma of the middle ear develops from glomus bodies, which are normally located at the bottom of the tympanic cavity, on the dome of the bulb of the internal jugular vein and in the temporal bone. They differ in structure from glomus bodies, which are located in other areas. Depending on the histological structure and the ratio of cell accumulations, there are 3 types of glomus tumors: adenoid-like, alveolar and angioma-like. According to the clinical course, limited and widespread forms of chemodectoma are distinguished.
Chemodectomas are observed at different ages and can be multiple in both ears. Sometimes neoplasms have a malignant course from the very beginning, despite the benign structure of the chemodectoma.
Chemodectomas, which are located in the tympanic cavity, in the initial period of the disease cause hearing loss and pulsating noise in the ear. At this time, the neoplasm appears through the eardrum. Then the tumor protrudes it and causes hyperemia (redness). Gradually, the neoplasm penetrates the external auditory canal and looks like a polyp. When you try to remove it, bleeding occurs. Sometimes patients report ear pain.
Chemodectomas that originate in the jugular vein bulb first destroy the dome of the jugular fossa and spread into the tympanic cavity. As the tumor increases and bone destruction occurs, symptoms of damage to the VII-XII pairs of cranial nerves develop. Patients are bothered by noise in the ear, and otoscopic changes occur. Chemodectomas can grow into the cranial cavity.
Diagnosis of chemodectoma is carried out using radiography of the jugular fossa, pyramid of the temporal bone, attic-antral region, mastoid process. X-ray examination includes radiography of the temporal bone in three main projections and tomography in direct and lateral projections.
Chemodect treatment is surgical. Small tumors that do not destroy the eardrum are removed or exposed to ultra-low temperatures. Tumors that have spread to the external auditory canal, mastoid process, or antrum are also subject to surgical treatment. Otolaryngologists perform operations of varying scope - from tympanotomy to extended radical surgical interventions on the ear. Sometimes cryotherapy is used. For tumors that destroy the pyramid and spread into the cranial cavity, external gamma irradiation is performed, which often causes growth arrest or a decrease in chemodectoma.
Malignant ear tumors
Locally destructive tumors of the ear include basal cell carcinoma, and malignant tumors include cancer, melanoma, and sarcoma. The most commonly observed are basal cell carcinomas and cancer. The listed tumors of the outer ear, affecting the skin and spreading to the cartilaginous and bone parts of the ear, grow into the scalp, bones of the face and skull, and the parotid salivary gland. They grow either slowly or very quickly.
Cancer of the outer ear often occurs at the site of injury, long-term inflammatory processes, or age-related skin changes. Develops under the influence of the following predisposing factors:
- Burns;
- Frostbite;
- Household and professional hazards.
Cancer of the outer ear can be endophytic (flat ulcer with infiltrated edges) or exophytic (warty nodules with a wide base). A cancerous tumor, having arisen in one or another part of the auricle, infiltrates and gradually destroys the entire shell, then spreads to adjacent tissues and organs. Cancer of the external auditory canal can grow into the auricle, mastoid process, middle ear, parotid salivary gland, skull bones and cause paralysis of the facial muscles on the side of the tumor.
Cancer of the external auditory canal in the early stages of development is usually impossible to recognize, since patients do not show any complaints, and the externally pathological process resembles weeping eczema or a chronic inflammatory process, which is manifested by the formation of pale granulations. During this period, the first signs of ear cancer are often observed: itching and pain in the external auditory canal.
Cancerous tumors of the external auditory canal grow faster than tumors of the auricle and are characterized by severe bleeding. Further growth occurs towards the auricle or towards the middle ear, or in all directions at the same time. As the cancerous tumor spreads to the middle ear, surrounding tissues and bones, excruciating pain occurs and the following symptoms develop:
- Paralysis of facial muscles;
- Deafness;
- Metastases in regional lymph nodes.
Treatment of adenoma at the Mama Papa Ya clinic
Adenoma can occur in different organs, and its recognition requires an individual approach to each patient. The network of family clinics “Mama Papa Ya”, located in Moscow, offers services for the diagnosis and treatment of this benign tumor.
Advantages of the clinic:
- versatility;
- qualified personnel;
- modern equipment that allows performing minimally invasive surgical operations;
- convenience and comfort for the patient;
- affordable prices.
If you suspect the presence of an adenoma, it is recommended to make an appointment with a doctor directly at the clinic, on the website or by phone.
Reviews
Marina Petrovna
The doctor carefully examined my husband, prescribed an ECG and made a preliminary diagnosis. She gave recommendations on our situation and ordered additional examination. No comments so far. Financial agreements have been met.
Roakh Efim Borisovich
I am simply delighted with the doctor and the clinic. I haven't had fun in clinics for a long time. Everything went perfectly from a logistics point of view, strictly on time. I also received aesthetic pleasure both as a patient and as a person. I could communicate and this communication gave me great pleasure. My deepest bow to the ultrasound doctor.
Luzina Sofya Khamitovna
I really liked Dr. Vlasova. Pleasant and sweet woman, a good specialist. I received an answer to all my questions, the doctor gave me a lot of good advice. I was more than satisfied with the visit.
Evgeniya
We visited the “Mama Papa Ya” Clinic with our child. A consultation with a pediatric cardiologist was needed. I liked the clinic. Good service, doctors. There was no queue, everything was the same price.
Olga
I really liked the clinic. Helpful staff. I had an appointment with gynecologist E.A. Mikhailova. I was satisfied, there are more such doctors. Thank you!!!
Anonymous user
I removed a lump from Alina Sergeevna, the operation was great! Many thanks to her for her sensitive attention and approach to every detail.
Anonymous user
Today I was treated at the clinic, I was satisfied with the staff, as well as the gynecologist. Everyone treats patients with respect and attention. Many thanks to them and continued prosperity.
Iratyev V.V.
The Mama Papa Ya clinic in Lyubertsy is very good. The team is friendly and responsive. I recommend this clinic to all my friends. Thanks to all doctors and administrators. I wish the clinic prosperity and many adequate clients.
Belova E.M.
Today I had a mole removed on my face from dermatologist I.A. Kodareva. The doctor is very neat! Correct! Thanks a lot! Administrator Yulia Borshchevskaya is friendly and accurately fulfills her duties.
Anonymous user
I would like to express my gratitude to the staff of the clinic: Mom, Dad, and me. The clinic has a very friendly atmosphere, a very friendly and cheerful team and highly qualified specialists. Thank you very much! I wish your clinic prosperity.
Christina
I liked the first visit. They examined me carefully, prescribed additional examinations, and gave me good recommendations. I will continue treatment further; I liked the conditions at the clinic.
Anna
Good clinic, good doctor! Raisa Vasilievna can clearly and clearly explain what the problem is. If something is wrong, she speaks about everything directly, not in a veiled way, as other doctors sometimes do. I don’t regret that I ended up with her.
Osteoma
Osteoma in the ear (exostosis, osteophyte) develops mainly from the compact layer of the posterior wall of the bony part of the external auditory canal. Much less often, neoplasms are found on the lower and upper walls of this section. Endophytic osteomas penetrate into the mastoid process. Osteoma is a benign tumor that grows rather slowly.
Osteoma has the appearance of a round formation, which is covered with a skin layer, very dense when palpated with a Vojacek probe. It is treated surgically. The operation is performed after the tumor has grown to medium size. In this case, removing the tumor is technically as convenient as possible. If the tumor is small, there is a risk of not completely removing the pathological tissue. If the osteoma is large, it is possible to capture a significant part of the healthy bone tissue during surgery. This will cause a large bone defect.
Tumor of the inner ear
Inner ear symptoms occur in patients with tumors located outside this anatomical structure. Otolaryngologists do not know any neoplasms that would arise in the ear labyrinth. True cholesteatomas, which are rarely found in the inner ear, refer only to tumor-like formations, the structure of which is fundamentally different from the structure of known “tissue” tumors.
Neuroma of the vestibular-cochlear nerve is a benign encapsulated tumor that primarily develops in the internal auditory canal from the neurolemma of the vestibular nerve and subsequently grows in the direction of the cerebellopontine angle. As the tumor grows, it fills the entire space of the lateral cistern of the brain, significantly stretching and thinning the sections of the cranial nerve of the cerebellopontine angle that appear on its surface (facial, vestibulocochlear, intermediate and trigeminal). This leads to trophic disorders and morphological changes in these nerves, which disrupt their conductivity and distort the function of the organs they innervate. Filling the entire internal auditory canal, the tumor compresses the internal auditory artery, which nourishes the structures of the inner ear. Exiting into the area of the cerebellopontine angle, the tumor puts pressure on the arteries that provide nutrition to the cerebellum and brain stem.