Chronic periodontitis is one of the forms of the disease that occurs due to the fact that pathogenic microorganisms penetrate into the periodontal tissue through the openings of the root canals located at the tops of the dental roots. Chronic periodontitis of the roots is accompanied by a violation of the integrity of the ligaments that provide fixation and stability of the tooth, destructive processes of bone tissue and can lead to the formation of granulomas and large cysts.
Chronic periodontitis is a pathological process in the periodontal tissues. This is associated with the development of inflammation in the periodontium and the formation of fibrous, granulating, granulomatous tissue. In the chronic form of the disease, exacerbations periodically occur, during which swelling of the gums, loosening of teeth, the appearance of fistulas with the release of pus, etc. are observed. Specialists identify this pathology and distinguish it from similar diseases using electroodontometry, X-rays and visual examination. Lack of proper treatment leads to tooth loss due to weakening of the ligamentous apparatus and the growth of large capsules with pus.
Filling made of light-curing material for classes I and V - 2,000 rubles.
Filling made of light-curing material in classes II, III, IV - 3,000 rubles.
Placing a temporary filling - 400 rubles.
Resection of the root apex (frontal group) - 6,500 rubles.
Resection of the root apex (chewing group) - RUB 9,000.
Mechanical and medicinal treatment of canals for periodontitis (1 canal) - 1,100 rubles.
Closing perforations (MTA) - RUB 6,500.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 1,000
- The cost of an orthodontist consultation is 2,000
Make an appointment
Symptoms of the disease
General symptoms depend on the form of the pathology. When granulomas form, attacks of pain are observed when exposed to hot food. Pressure on the affected tooth and gum is accompanied by pain. The size and density of the mucosa in the affected area changes, and a granuloma forms under the bone or mucosa.
An exacerbation is accompanied by the appearance of fistulas, which grow and gradually release their contents into the oral cavity. In this case, purulent fistulas can appear not only on the gums, but also on the cheekbones, cheeks, neck, and chin. Isolation of pus may be performed along with the isolation of granulosa tissue. Then the fistula goes away, and a scar appears in its place.
The granulomatous form occurs for a long time without pronounced symptoms. Only after the granuloma grows to a large size and cysts form, the main symptoms appear: discoloration and severe pain in the tooth, development of gumboil and swelling of the gums in the affected area. Cysts that are too large can cause a jaw fracture and long-term rehabilitation.
Fibrous periodontitis is the most hidden form of pathology. There is no pain when chewing food or drinking hot drinks. Severe symptoms are observed only during exacerbation. There is general poisoning of the body due to the penetration of pus into the blood, the tooth becomes loose, and the lymph nodes in this area become larger.
Cyst - what is it and why?
A cyst is a cavity that has an epithelial lining and cystic contents. There are two types of cysts - true and pocket.
The true one is completely covered by the epithelial lining, and the pocket one communicates with the root canal, it seems to grow from it.
Cyst formation occurs in 3 stages.
At the first stage, the epithelial cells of the islets of Malasse most likely proliferate under the influence of growth factors.
During the second stage, an epithelial cavity is formed.
These epithelial cells are directed away from their source of nutrition, die, and neutrophils drag their remains into the area of necrosis. Microcavities are formed, which then merge into one and become limited by stratified squamous epithelium.
There is another theory - the theory that the epithelium covers all open connective tissue areas, resulting in necrosis.
At the third stage of cyst formation after the death of neutrophils, there are reserves of prostaglandins, as well as cytokines produced by macrophages and T lymphocytes. Together they activate osteoclasts and trigger bone resorption.
Pocket cysts have a different mechanism of development. There is a large accumulation of neutrophils near the apical foramen in response to root canal infection. The cells die, as before, and this microabscess is closed by proliferating epithelium. A so-called epithelial ring is formed. Neutrophils that remain outside the channel die and form a microcavity. The presence of infection outside the canal further attracts neutrophils, expanding the microcavity to larger sizes. A pocket cyst is called such because the enlargement of the root canal resembles an enlargement of the periodontal pocket.
Causes of chronic periodontitis
Chronic periodontitis appears in the absence of treatment of the acute form. The disease develops due to traumatic, toxic, infectious, mechanical effects on tissue.
The infectious form develops due to the penetration of pathogenic microorganisms into the oral cavity. This is due to damage to soft tissues by staphylococci, diphtheroids, and streptococci. The penetration of bacteria into tissues occurs through the openings of the root canals or through the hematogenous route. Often the infection progresses against the background of osteomyelitis, sinusitis, periodontitis, and tonsillitis.
The fibrous form often progresses after severe trauma. For example, after tissue destruction with a pin, filling, or crown. Pathology can also develop due to a strong blow.
Drug-induced periodontitis occurs due to the use of drugs that provoke coagulative necrosis of the periodontal ligament. These include resorcinol-formalin and arsenic paste. Tissue poisoning is provoked by local anesthesia, iodine, acids, etc.
Indications
The lack of a positive result after conservative and surgical treatment is the main indication for removal of affected teeth. Extraction is performed for the following symptoms:
- Significant damage to the crown.
- Severe loosening of the tooth.
- Formation of large cysts and granulomas.
- Impossibility of performing the operation due to obstruction of the canals.
- Lack of results with surgical and conservative treatment.
Contraindications
- Oral infections.
- Allergy to anesthesia.
- Intolerance to antibiotics and antimicrobial agents.
- Acute diseases of the cardiovascular system.
- Poor blood clotting.
Reviews about our doctors
I am very grateful to Evgeniy Borisovich Antiukhin for removing my three eights.
Especially considering that the lower tooth was not the simplest (it was located in an embrace with a nerve). The removal took place in 2 stages, one tooth under local anesthesia, two under general anesthesia. I had no idea that wisdom teeth could be... Read full review Sofia
28.12.2020
Words cannot express my gratitude to Elena Nikolaevna Kiseleva. This is the best doctor in the world. I got an appointment after many years of being ignored by the dentist’s office and with a bitter experience of treatment in another paid clinic, the mistakes of which had to be corrected in the first visits. Thank you for this... Read full review
Roman Stanislavovich Sh
25.07.2020
Types of chronic periodontitis and their clinical manifestations
It is customary to distinguish several forms of the disease, the diagnosis of which is necessary in order to correctly prescribe treatment for chronic periodontitis. To do this, the dentist conducts a visual examination of the oral cavity, prescribes electroodontic diagnostics and x-rays.
Chronic fibrous periodontitis
Self-diagnosis of this type of chronic periodontitis is very difficult due to the almost complete absence of clinical manifestations.
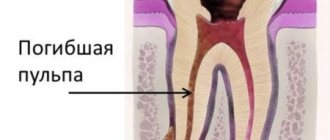
The patient does not experience pain, and there is no reaction to temperature stimuli. During the examination, the dentist notes a change in the color of the tooth, the presence of a reaction to percussion and painful probing. The tooth cavity is filled with dead pulp, which emits a putrid odor. The X-ray image clearly shows the increase in the periodontal fissure at the root apex; there is no destruction of bone tissue and cement.
Chronic granulating periodontitis
The painful sensations characteristic of this type of chronic periodontitis are not significant.
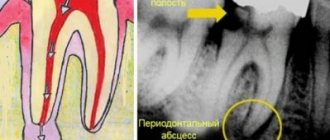
There are sensations of heaviness and fullness, and minor pain may be present when exposed to mechanical stimuli. Exacerbation of chronic granulating periodontitis is accompanied by the formation of a fistula through which pus comes out or granulation tissue grows. With this disease, the gums become loose. When pressing on the inflamed area with the blunt end of a dental instrument, a small depression appears, which disappears only after some time. The x-ray image shows the focus of the destructive processes of bone, dentin and cement.
Chronic granulomatous periodontitis
The symptoms of chronic periodontitis of this type are also practically invisible to the patient. Sometimes minor discomfort and pain may occur when biting on the affected tooth.
An examination by a dentist can reveal a change in the color of the crown of the tooth, but a carious cavity is not necessarily present. Remnants of dead pulp are found in the root canals. If the canals were previously sealed, then the quality of the filling is not good enough.
An X-ray image allows you to determine the destruction of bone tissue, which has a round shape. Often this process can be found on dental tissues or the root apex area.
Prevention
To prevent the development of granulomatous periodontitis, it is necessary to promptly identify and treat dental diseases. To do this, you need to visit a doctor at least twice a year, and not just when the problem becomes obvious. We must not forget about regular oral hygiene, as well as periodic professional teeth cleaning, since dental plaque is a breeding ground for pathogenic bacteria that cause various diseases, including granulomatous periodontitis.
Treatment of the chronic form
Good patency of the canals allows for therapeutic treatment:
- Opening a tooth.
- Antiseptic treatment.
- Cleaning the channels.
- Use of anti-inflammatory drugs.
- Installation of a temporary filling.
After the procedure, antibiotics are prescribed and re-appointed after 3 months. If the x-ray shows a cure for the disease, then the canals are treated with an antiseptic and a permanent filling is installed. Surgical intervention involves cystectomy, resection of the upper part of the root, hemisection, and root removal. Lack of results after treatment is a reason for extraction of the diseased tooth.
Second visit
After a couple of days, the doctor at the appointment assesses the patient’s condition - whether there are any swellings, whether the temperature has risen, whether the lymph nodes are inflamed, etc.
If no complaints are received, the doctor removes the temporary filling and turundas with cresophen, and then obturation of the root canals with temporary filling material. Its task is to help the bone tissue partially regenerate in the place where the inflammatory process was noted at the root apex. In addition, the substance sanitizes and disinfects the tubule cavity. Calcium hydroxide-based pastes are mainly used as temporary fillings: Calasept, Metapex.
From above, all this is covered with a new non-permanent filling.
Exacerbation of chronic periodontitis
Often patients seek treatment for acute chronic periodontitis, which manifests itself quite clearly. This mainly applies to granulomatous and granulating types, exacerbations of which occur much more often than fibrous types. Clinical manifestations during this period include:
- constant localized pain;
- swelling of soft tissues;
- the presence of a reaction to mechanical stimuli;
- painful reaction of the lymph nodes.
Recommendations after treatment
After conservative or surgical treatment, you should not eat food for 2-3 hours due to the effects of anesthesia. Pain may be experienced for 7 days after surgery. It is recommended to rinse your mouth with antiseptics and a decoction of medicinal herbs. For severe pain, it is recommended to take painkillers. If pain persists and severe swelling is observed, contact your doctor immediately.
At the same time, the crown of the tooth changes its color, the presence of a carious cavity and tooth mobility are noted. Dentists at the CELT clinic successfully treat even the most advanced and severe forms of chronic periodontitis!
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Diagnostics
In order to correctly diagnose and differentiate this type of periodontitis from fibrous or granulomatous, the dentist conducts a visual examination of the oral cavity, which allows us to identify:
- severely damaged natural tooth crown/large filling/artificial crown;
- change in color of the affected tooth;
- communication between carious and dental cavities;
- insignificant pain reaction to percussion;
- looseness of the gums, on which, after pressing with a dental instrument, a depression is formed.
During a visual examination, the specialist sees swelling of the gums, severe tooth decay, and a change in the color of the enamel. Granulating periodontitis is often observed on teeth with large fillings that have not been changed in a timely manner. Probing of pathological carious tissues does not lead to pain. When the probe is pressed on the affected mucous membrane, the gums become pale and indented. The recess is preserved for a long time. Electroodontodiagnosis is used to accurately identify granulating periodontitis. An increase in the sensitivity threshold of the pulp to 100-150 μA is detected. An x-ray is taken which shows the destruction of the jawbone.
In addition to a visual examination, dental x-rays are performed, which reveals destruction of the jaw bone, and electroodontodiagnostics, which determines an increase in the threshold of pulp excitability.