Dental periodontitis is an inflammation of an infectious nature that occurs at the membrane of the tooth root and affects the tissues of the oral cavity located next to it. Periodontitis is difficult to confuse with other dental diseases, because it has a clear symptom – severe and constantly increasing pain, which cannot be relieved by taking tablets from the pharmacy.
Treatment of periodontitis must be carried out urgently, because you risk not only losing a tooth, but also acquiring complications that are dangerous to the overall health of the body! How periodontitis occurs, what signs will help to identify the disease in a timely manner, how periodontitis is treated in dentistry, at what prices the service is offered in Moscow - we will talk about this in detail in this article.
Causes of dental periodontitis
Various reasons can lead to the appearance and development of dental periodontitis, but in the vast majority of cases the disease appears:
- Against the background of untreated dental caries and pulpitis;
- Due to poor quality treatment of tooth canals, or more precisely, mistakes made when filling the canals.
Less commonly, periodontitis occurs after injuries, incorrectly installed dental fillings, or violation of the dosage of dental medications.
Whatever the cause of periodontitis, its treatment cannot be delayed due to fear of dentists. It is important to understand that you will not stop the inflammation on your own, with pills or folk remedies, and the more it progresses, the less chance you have of saving the tooth. In addition, periodontitis can also affect neighboring healthy teeth.
How to identify periodontitis and not confuse it with caries or pulpitis? We already talked about the most striking symptom of the disease at the very beginning of the article, but the signs of periodontitis may vary depending on the form of the disease. Therefore, below we will consider the main types of dental periodontitis, as well as talk about their characteristic symptoms.
Take a short test and calculate the cost of treatment!
Take a short test
- Which teeth have caries?
- Visual assessment
- Reaction to stimuli
- Cost calculation
×
Manukyan Artavazd Genrikovich
Chief physician of the clinic
Development (pathogenesis) of periodontitis
The development of periodontal inflammation is associated with the entry of infectious and toxic contents of the root canal into the periodontal gap; the presence of an irritating agent - coccus, its waste products, and medications is necessary. In the passage of the inflammatory process in the periodontium, an important role is played by endotoxins, which are formed when the membrane of gram-positive bacteria growing in the root canals of teeth devoid of pulp is damaged, in particular, bacterial endotoxin, which has a toxic and pyrogenic effect.
With periodontitis, multiple damage to connective tissue cells and a massive release of lysosomal enzymes are observed. Endotoxin entering the apical tissue leads to degranulation of mast cells, which are a source of heparin and histamine.
Biologically active components cause a sharp increase in vascular permeability, swelling and infiltration increase. Microcirculation is disrupted, thrombosis, hyperfibrinolysis and secondary hypoxia are observed, which leads to depolymerization of the main substance. Hypoxia increases, trophism is disrupted, signs of inflammation clearly appear: local increase in temperature, pain, swelling, hyperemia, dysfunction. The fabric becomes permeable due to the formation of voids in the main substance, and its main function is fulfilled - protective. The trophic function is sharply disrupted: the cell is not able to receive oxygen and BAC from the main substance and, conversely, release waste products into it. Slagging of both cells and intercellular substance is noted, the latter is associated with dysfunction of the vascular wall.
Bacterial endotoxins activate complement components, biologically active substances are formed that increase vascular permeability, and the consequence of this is the accumulation of mononuclear lymphocytes and macrophages. These cells secrete enzymes that increase the activity of osteoclasts, which cause the destruction of bone tissue.
Signs of acute periodontitis
Symptoms of acute periodontitis are always pronounced. Among them:
- Acute aching pain, the intensity of which is constantly increasing;
- Pain increases when trying to eat;
- If treatment for periodontitis was not started on time, attacks of pain will appear more and more often, and the intervals between them will become shorter and shorter;
Against the background of intense pain, a person cannot eat, speak, sleep, and may develop an elevated temperature. In the acute form of periodontitis, significant tumors and swelling often appear in the area of the diseased tooth. The cheek may also swell. This occurs due to the active accumulation of pus in the soft tissues of the oral cavity.
Prevention
To reduce the risk of developing the disease, you should follow simple recommendations:
- Brush your teeth at least 2 times a day. It is advisable not to use hard brushes to avoid injury to the gums.
- After eating, rinse your mouth with warm, clean water or a special mouthwash.
- Use toothpicks less often.
- Visit your dentist regularly.
- Remove tartar twice a year and undergo professional cleaning.
- Get rid of bad habits. Alcohol and smoking greatly impair dental health.
Periodontitis is one of the most common dental diseases. If you take good care of your teeth and maintain oral hygiene, you can significantly reduce the likelihood of its occurrence.
Back
Symptoms of chronic periodontitis
Chronic periodontitis is a very insidious form of the disease, since it can develop completely asymptomatically. It is extremely rare for a person to feel a slight pain when trying to bite something on a sore tooth; sometimes unpleasant sensations appear when consuming hot food and drinks.
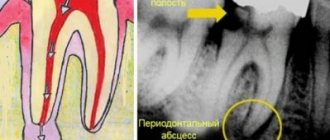
Chronic periodontitis of the tooth is diagnosed with an x-ray, which clearly shows the process of bone destruction at the apex of the tooth root. This form of the disease has its own classification, according to which there are: fibrous, granulating and granulomatous periodontitis. With fibrous periodontitis, there is almost no pain, which is why it is most often recognized either in the acute phase or during an examination by a dentist and x-rays.
Treatment of this form of periodontitis is quite simple and is carried out in 1-2 visits to the doctor. Granulomatous chronic periodontitis most often develops asymptomatically, but under the influence of certain external factors it easily turns into an acute form. The disease has its own characteristic symptom, manifested in the formation of granulomas - capsules with pus, which separate tissues affected by inflammation from healthy ones. The treatment process for granulomatous periodontitis is long and complex, it can last for several months and even require surgical intervention!
Methods and stages of treatment
Treatment of periodontitis is divided into several stages. The first and most important is tooth depulpation - removal of necrotic tissue from the root canal, its mechanical treatment and expansion, treatment with antiseptic and anti-inflammatory drugs.
Important! If a tooth affected by periodontitis was previously filled, the doctor will have to remove the filling materials from the canal and re-process and prepare it.
In the future, conservative or surgical treatment of periodontitis is carried out.
Conservative therapy
To conservatively eliminate periodontitis, local agents are used, which the doctor places into the prepared root canal. Most often these are long-acting pastes with an antiseptic and anti-inflammatory effect, “Kalosept” or “Metapex”. They are left in the canal for 2-3 weeks, and in case of extensive tooth damage, they are periodically renewed for 2-3 months. Additionally, antibiotics are prescribed, rinsing the mouth with antiseptic (chlorhexidine, Miramistin, etc.) or saline solutions, herbal decoctions, etc.
Important! During the treatment, photographs are taken that will show the dynamics. If the inflammation is stopped, treatment can be completed with a filling.
Surgery
Surgical methods of treating periodontitis are resorted to in the absence of positive dynamics, a large focus of inflammation at the apex of the tooth root (more than 10 mm in diameter), and when it is impossible to depulpate and clean the root canals (previously installed gutta-percha, stump inlays, etc.).
Several methods of surgical treatment of periodontitis are used:
- resection of the apex of the tooth root - cutting off a third of the root with granuloma through an incision on the gum;
- hemisection - removal of the entire root with tissues surrounding the root;
- root amputation - removal of the root while preserving the crown;
- separation - removal of the root along with part of the crown;
- replantation is the removal of a tooth and its subsequent treatment outside the oral cavity, and its subsequent implantation in its original place.
These methods allow you to save a tooth for a certain period of time. If they are impossible due to the destruction of most of the crown, perforation of the roots, rapid spread of infection and necrosis of bone tissue, a radical tooth extraction is performed, followed by treating the hole with antiseptics, scraping out the granuloma and filling the cavity with agents that stimulate the formation of bone tissue.
Other
How does the acute phase of chronic periodontitis manifest?
When exacerbated, chronic periodontitis of the tooth expresses itself with the same symptoms as the acute form of the disease. That is, there is a strong, aching pain, swelling of the gums and swelling of the cheek. Typically, chronic periodontitis enters the acute phase when the immune system is weakened, the flu, ARVI, or simply severe hypothermia are present. If, during an exacerbation of the chronic form, a fistula appears in the gum area, pus will flow from the area of inflammation and the pain in the tooth will gradually subside.
But this does not mean that periodontitis has gone away on its own; the inflammatory process will continue to develop and will manifest itself again under favorable external factors, which we discussed just above. Based on the type of periodontitis, a treatment regimen is selected. The price of the service depends on the regimen chosen for treating the disease. We will tell you below about all the stages of treatment of dental periodontitis in different forms and prices for procedures. But no matter in what form periodontitis develops, its treatment always begins with diagnosis.
Diagnosis of periodontitis involves examination of the oral cavity, x-rays, and examination of patient complaints. All this together helps to accurately diagnose the form of periodontitis and prescribe adequate and effective treatment.
Why periodontitis is dangerous
Periodontal inflammation is the stage following pulpitis in the spread of infection from a carious tooth.
Its focus is located at the apex of the root and is a small cavity filled with pus.
In the absence of therapy, the infectious-inflammatory process spreads to the periodontium - the intermediate tissues that separate the roots and neck of the tooth and the bone tissue of the gums.
Important! The periodontium surrounds the entire subgingival part of the tooth and plays the role of cement that fixes the tooth in the jaw. When it is damaged due to periodontitis, the likelihood of tooth loosening and loss increases many times over.
Most often, periodontitis is localized at the apical part of the root affected by pulpitis. If left untreated, the inflammation spreads further, covering the entire subgingival part of the tooth. As the disease develops, a purulent cavity forms around the roots, which sooner or later opens onto the mucous membranes of the oral cavity or onto the skin of the face. When it becomes chronic, periodontitis is accompanied by constant suppuration with the outflow of contents through a fistula - long-existing ducts, the walls of which do not grow together.
Complications
If pulpitis is neglected or treated incorrectly, concomitant pathologies arise:
- necrosis, or gangrene of neurovascular tissue;
- pulp degeneration with the formation of solid inclusions in the cavity - denticles, pulp stones;
- improper formation of hard structures - secondary or irregular dentin is actively formed.
If the infection extends beyond the dental cavity, the adjacent tissues of the maxillofacial region are involved in the pathological process. Diagnose:
- inflammation of the periosteum;
- abscess;
- osteomyelitis – purulent softening of bone tissue;
- phlegmon - purulent melting of soft tissues.
Causes of the disease
- Deep caries
- Pulpitis
- Periodontal trauma due to external influences (for example, sports injury)
- Infection through the bloodstream if there is any infection in the nasopharynx or upper respiratory tract (for example, with sore throat or tonsillitis)
- Poor quality treatment of dental canals (perforation of the root, leaving fragments of dental instruments);
- Bad habits (biting a pen or pencil, biting thread with teeth, etc.)
- Chronic problems in the endocrine system
- Decreased immunity, regardless of the cause
Important: only after an examination (including hardware) will the dentist be able to determine what caused the disease. Our network of clinics has all the necessary equipment that allows a specialist to accurately determine the stage, form and cause of the pathology.
Clinical symptoms
- Pain in the affected area, radiating to surrounding tissues
- Increased pain when biting or touching
- Swelling of the gums (not always)
- Enlarged lymph nodes
- General malaise caused by intoxication
- Increased body temperature
- The appearance of slight tooth mobility
- Possible discoloration of tooth enamel
- Fistula formation (not always)
- Discharge of pus from the gums near the affected dental element (not always)
Note: symptoms can manifest themselves either as a complex or as several symptoms. Therefore, it is important that the patient, if at least some of them appear, contacts the dentist. You can make an appointment with our specialists by phone or by leaving a request on our website.
Signs and symptoms of a dental cyst
Often the development of a cyst is completely asymptomatic or with barely noticeable symptoms: rare slight pain when biting on a tooth or mild pain when pressing on the gum. In this case, the cyst is detected completely by accident - on x-rays during the treatment of other teeth.
The main signs of a cyst begin to appear already at a late stage of development. Main symptoms of a cyst:
- Aching or nagging pain that only gets worse all the time. It is difficult to get rid of it with the help of simple analgesics and folk remedies. Initially, pain may occur when chewing on the causative tooth.
- The appearance of edema. When a cyst occurs, the gums around the diseased tooth become red and swollen.
- High temperature due to associated infection.
- Suppuration, flux and fistulous tract are external manifestations of an already formed cyst.
- X-rays and tomography are necessary to clarify the diagnosis.
Who is most susceptible to periodontitis?
Most often, periodontitis develops due to:
- bacterial infection: for example, tooth pulpitis, or due to incomplete removal of pulp decay from difficult-to-pass equine canals;
- infection is possible from the tissues surrounding the periodontium, as, for example, with sinusitis;
- injuries: more often - blows, incorrectly placed and greatly inflated fillings or crowns;
- drug exposure: penetration of potent and toxic drugs into the periodontium during the treatment of pulpitis, such as, for example, arsenic or formaldehyde.
Differential diagnosis of acute pulpitis
Differential diagnosis of acute pulpitis is carried out with various diseases. Although the symptoms of acute pulpitis are pronounced and specific, there are similarities with other pathologies. However, in making the correct diagnosis, it is more important to pay attention to the following differences:
Pulp hyperemia
With pulp hyperemia (deep caries), there is no spontaneous night pain reaction. A short painful attack is provoked by external stimuli.
Gingivitis
The presence of inflamed, swollen gums, gingival papilla, and associated pain is a manifestation of papillitis or gingivitis.
Acute apical periodontitis
Acute apical periodontitis is also accompanied by pain, but of a different nature. It is constant, aching, and worsens when biting. Palpation of the transitional fold is also painful. There is no reaction to external stimuli. The result of electroodontodiagnostics is a response with a value of more than 100 microamps.
Trigeminal neuralgia
With trigeminal neuralgia, pain occurs when certain “trigger” areas of the face are touched.
Sinusitis
Sinusitis (sinusitis) is manifested by deterioration of health, fever, and headaches. Breathing is difficult, purulent exudate is released. When you tilt your head forward, heaviness and bloating appear. The localization of these symptoms is the area of the maxillary sinus. The x-ray shows characteristic changes in the sinuses.
Alveolitis
A strong pain reaction can also manifest itself with alveolitis. An examination helps to detect the socket of a recently removed tooth. The socket is covered with a gray coating, there is no blood clot. Characterized by an unpleasant odor. Palpation of the gums in its area is sharply painful.
Acute pulpitis in children
Symptoms of acute pulpitis in children are somewhat different from those in adults. This is due to the structural features of hard tissues and pulp of temporary or permanent teeth with unformed roots.
Firstly, acute pulpitis in children is rare, mainly in healthy children with low caries activity. Partial pulpitis is an even rarer phenomenon, because the barrier between the root and coronal pulp is immature. Serous pulpitis very quickly turns purulent.
Secondly, the tooth cavity is always closed, the carious cavity is filled with light infected dentin.
Thirdly, in children, acute pulpitis is often accompanied by a periodontal reaction, swelling of the soft tissues surrounding the tooth. Regional lymph nodes become inflamed. The general condition worsens: inflammation spreads to the bone tissue.
Finally, the most common outcome of acute pulpitis of primary teeth is pulp necrosis.