Why is it so important to treat tooth decay in a timely manner?
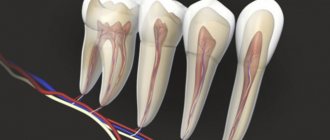
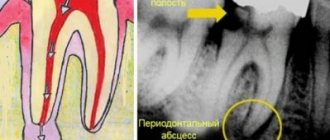
If you feel a sharp pain in a tooth affected by caries, it is quite possible that you have developed pulpitis . Pulpitis is an inflammation of the dental nerve, most often a complication of caries. Inside the hard shell of the tooth there is soft tissue (pulp), consisting of special cells and penetrated by nerves, lymphatic and blood vessels. With advanced caries, the infection penetrates into the pulp through the destroyed tooth wall, causing focal inflammation. This stage of the disease is called acute pulpitis and is characterized by acute pain in the tooth, which intensifies at night, as well as from contact with hot and cold food. If you do not consult a dentist and do not begin timely treatment of a diseased tooth, the inflammation will enter the chronic stage. Various types of chronic pulpitis are characterized either by the growth of the connective tissue of the tooth (up to the formation of a fibrous polyp), or by the decay of the soft tissues of the tooth. If tooth treatment is not started at this stage, pulpitis can lead to periodontitis - a violation of the integrity of the tissues surrounding the tooth. Periodontitis is characterized by acute pain at the slightest pressure on a tooth and threatens its loss, as well as the destruction of bone tissue and the formation of cysts.
Forms and symptoms of pulpitis
Patients usually think that the main sign of pulpitis is pain and a large carious cavity in the tooth, but this is not entirely true.
There are acute and chronic forms of pulpitis, depending on the strength of the inflammatory process affecting the pulp. Severe pain, which is often not relieved by painkillers, is characteristic of the acute form of the disease. But, if it becomes chronic, the pain subsides and practically does not bother you anymore.
As for large “holes” in a diseased tooth, the patient may not see them. Pulpitis also occurs as a result of caries hidden under a thin layer of enamel and under a previously installed filling. The pulp can become inflamed in a tooth without caries, although this happens much less frequently, due to an infection brought into the tooth with blood.
Treatment of pulpitis
The easiest way to get rid of the disease is to avoid it by carrying out the necessary preventive procedures in a timely manner. If you have caries, it is better to start treating it before various complications arise. Modern dental methods and equipment make it possible to almost completely avoid unpleasant pain during the treatment of caries and keep your teeth healthy and beautiful for a long time.
If you have already developed inflammation of the dental nerve, you need to consult a specialist as soon as possible. After examining and taking an x-ray, a competent dentist will be able to answer whether in your case it is possible to save the tooth or whether it is necessary to remove it. In most cases, removal of a tooth affected by pulpitis is carried out in two visits. First, under anesthesia, the root canal of the tooth is opened and the affected pulp tissue is removed. The dentist cleans the root canals, fills them and applies a devitalizing paste and a temporary filling. During the second visit, an X-ray examination is performed to assess the quality of canal filling and the presence of possible complications. If no intervention is required, a permanent filling is installed. In the future, to strengthen the pulpless tooth, it will be necessary to install a crown on it.
Treatment methods for dental nerve inflammation
Pulpitis is easier to eliminate at an early stage. If the inflammation affects only part of the nerve, drug treatment is possible. The pulp chamber is opened, antibacterial and anti-inflammatory drugs are placed inside, a temporary filling is placed, and upon completion of treatment it is replaced with a permanent one.
If it is not possible to save the nerve, all affected tissue is removed, the root canals are cleaned and the tooth is filled. A pulpless tooth may darken, and pain after treatment may persist for several days.
Why does a tooth hurt after nerve removal?
Pain that bothers you immediately after tooth nerve removal is normal. The tissues surrounding the tooth, damaged during pulp removal, are also penetrated by nerve fibers and have sensitivity. However, if the pain after depulpation continues for quite a long time and does not subside, you need to consult a specialist again. Most often, pain in a tooth deprived of a nerve is caused by complications after an improperly performed depulpation operation. The most common reasons are partial removal of the dental nerve, inadequate treatment of root canals (the filling substance does not completely fill the canal or extends beyond it), as well as leakage of the installed filling. Such errors lead to the creation of a focus of chronic inflammation in an already dead tooth, devoid of pulp, and the further development of periodontitis. This situation can be corrected by unsealing and secondary cleaning of the root canals using disinfectants. In some cases, it is necessary to perform a resection of the apex of the tooth root - a surgical operation during which the tooth root and the inflamed tissue surrounding it are removed through an opening in the gum. If more gentle treatment does not produce results, the diseased tooth is completely removed, followed by the creation of a dental implant in its place.
Acute pulpitis
Acute pulpitis, as we have already said, is characterized by severe toothaches that occur WITHOUT a reason and intensify at night. The main symptomatic difference between acute pulpitis and caries is that pain in deep caries is always associated with an irritant, and stops when the action of the irritant is interrupted. The pain associated with pulpitis is pulsating, not associated with impact on the tooth, is difficult to relieve with tablets, and radiates to the ear, jaw, and temple. It is difficult for the patient to determine which tooth hurts; usually he complains that half of the jaw hurts.
There are several forms of acute pulpitis, depending on the location and manifestations of the inflammatory process:
| Forms of acute pulpitis | What is the difference? | Nature of pain |
| Focal | Inflammation of the coronal part of the pulp | Paroxysmal severe pain that radiates to the jaw. |
| Diffuse | Inflammation of the entire pulp | The pain lasts 10-15 minutes with a break of several hours. Symptoms are worse when lying down. |
| Serous | Very severe inflammation in an advanced stage | Continuous throbbing pain. |
| Purulent | Pus forms in the dental canals | Under the influence of warm food or drink, the pain intensifies, and cold food relieves it. |
Reasons why the dental nerve becomes inflamed
The immune system responds to an infection that has affected the internal tissues of the tooth with local inflammation. The reason for the penetration of pathogens into the pulp may be:
- Advanced caries. A carious cavity that has reached the dentin violates the integrity of the hard tissues that protect the pulp chamber. The pulp is exposed, making it possible for bacteria from the oral cavity to penetrate into it. The risk of developing pulpitis due to caries is especially high against the background of insufficient oral hygiene , when plaque accumulates on the surface of the diseased tooth. A doctor can identify the risk of developing pulpitis during a routine examination - even before the patient has a toothache.
- Poor quality of dental services. Infection can enter the pulp during dental treatment. For example, in case of insufficient antiseptic treatment, violation of the technology of turning the crown for installation of an orthodontic structure, or incomplete filling of the root canals with filling material. The infection spreads exclusively within the pulp; timely diagnosis of such inflammation is made difficult by the absence of visual defects - the crown looks healthy, the pulp is not exposed. The patient learns that the nerve in the tooth is inflamed and something needs to be done about it by an attack of severe pain.
- The use of low-quality dental materials: antiseptics, gaskets, filling compounds.
- Hypothermia and previous acute respiratory viral infection. To chill the nerve fibers of your teeth, you don’t need to be in sub-zero temperatures for a long time—a few hours in an air-conditioned room or a trip in a vehicle with the windows open in the summer is enough.
If the nerve bundle in the pulp becomes inflamed from hypothermia or after an acute respiratory viral infection, there is a high probability of the inflammatory process spreading to the facial nerve branches and the development of trigeminal neuralgia.
- Mechanical injuries resulting in inflammation of the internal tissues of the tooth.
- Inflammatory periodontal diseases: gingivitis, periodontitis.
- The presence of cysts and granulomas in the jaw area.
First symptoms
Clinical signs of damage to the mandibular nerve are expressed in discomfort in the area of innervation: the area of the mental foramen, the lower lip, the membrane of the gums and cheeks to the borders of the second molar.
Pathology is expressed:
- Paresthesia – change in sensitivity (no painful sensations during injection, etc.).
- Dysesthesia is a change in sensitivity that brings discomfort (pain, “pins and needles”).
- Anesthesia – complete loss of sensitivity.
When extracting wisdom teeth, the lingual nerve is most often damaged (up to 2.1%). During implantation, damage to this nerve is less common and manifests itself with the following symptoms:
- increased salivation;
- speech defects;
- involuntary tongue biting;
- problems with swallowing;
- loss or change in taste;
- burning sensation of the tongue;
- numbness of the mucous membrane of the tongue and gums.
Up to 90% of lingual nerve injuries heal on their own within 7-10 weeks of onset.
Classification of manifestations
According to Seddon's classification, injuries to the trigeminal nerve are of several types:
- Neuropraxia. The damage is reversible. The sheath of the nerve fibers is not affected. There is no degeneration. Sensitivity returns a few weeks after treatment.
- Axonotmesis. Requires long-term therapy for up to six months. Fiber damage occurs and degeneration develops. The damage is reversible.
- Neurotmesis. Nerve structures, fibers and connective membranes are affected. Scars form. The pathological process is irreversible. Surgery is required.
According to the WHO classification, there are five categories of NAS lesions:
- compression or traumatic injury;
- edema;
- gap;
- final break;
- post-traumatic fibrosis.
Assessing the complexity of a clinical situation
To diagnose neurological pathologies, two research methods are used:
- Mechanoceptive. The tissue response to mechanical action and stimulation is recorded.
- Two-point irritation.
- Brush test.
- Nociceptive. Determine the perception of pain.
- Using a pin.
- Temperature test.
You can determine a taste deficiency by using a cotton pad with sugar or salt.
Research is carried out simultaneously on the affected and healthy sides of the maxillofacial apparatus.
Symptoms are documented. Areas of neurosensory deficit are measured with an accuracy of 1 mm.
Therapy concept
Medical tactics for pain and discomfort:
- Monitoring the patient and tracking the dynamics of the condition over a certain period of time.
- Drug therapy. The use of painkillers, hydrogen pump blockers, glucocorticosteroids and other drugs.
- Removing or unscrewing the rod several turns. It is carried out within 24 hours after implantation. The critical period of treatment is three months. It is during this period that improvement should occur.
- Carrying out a microsurgical operation.
There are no strict treatment protocols. The doctor selects the best option based on practical experience and knowledge.
It is generally accepted that the clinical result of the operation is achieved only if it is performed within a year after implantation.
Surgery
Indications for the operation:
- Confirmed nerve damage.
- Persistent sensory impairment for three months.
- Pain due to a pinched nerve.
The result of surgery depends on certain factors:
- Time elapsed from injury to surgery.
- Type and severity of manifestations.
- Features of blood supply in the pathological zone.
- Proper selection and preparation of the rod.
- The general health of the patient.
- Age.
- Presence of tension zones.
- Experience and practical skills of the surgeon.
Speed of diagnosis is key. Especially with minor damage. Late diagnosis threatens the formation of carpal tunnel syndrome.
Chronic pulpitis
Chronic pulpitis occurs if acute pulpitis is not treated. At some stage, acute pain subsides, but destructive processes in the pulp continue. The infection lies dormant and makes itself felt by periodic “shots” in the presence of hot, cold, sour, and sweet foods. Pain occurs when pressing on a tooth. At any moment, acute inflammation may begin again or the disease may be aggravated by a new complication.
Chronic pulpitis also has several forms:
| Forms of chronic pulpitis | Main characteristics | Nature of pain |
| Fibrous | The pulp bleeds when pressed | Short-term pain, as a reaction to cold and hot. |
| Hypertrophic | Pulp growth, which can extend beyond the open carious cavity, bleeding when eating. | There is no pain, it does not hurt when tapped, there is no reaction to irritants. |
| Gangrenous | Pulp necrosis, tooth darkening, rotten smell. | Short-term pain, as a reaction to hot food. |
Pulpitis of the wisdom tooth
Pulpitis can affect all teeth without exception. But eighth wisdom teeth have an increased risk of pulpitis. They are located far away, it is difficult to clean and treat them, so inflammation of the pulp in third molars occurs more often. Treatment of pulpitis of eights is also complicated by their inconvenient location and numerous roots. The risk of complications during endodontic treatment increases and the long-term prognosis for these teeth worsens. So in the case of acute pulpitis of a wisdom tooth, it makes sense not to treat such a tooth, but to remove it immediately.
Complications of pulpitis
Untimely treatment of acute pulpitis leads to a chronic process. A hidden infectious focus is formed in the body, which can provoke the appearance of both new dental diseases and general ailments, such as:
- flux - periostitis, purulent inflammation of the periosteum,
- osteomyelitis - inflammation of the bone tissue of the jaw,
- purulent inflammatory processes of intraoral tissues and soft tissues of the face,
- dental cyst - a benign neoplasm near the tips of the roots,
- sepsis - blood poisoning,
- The infection spreads to other organs through the bloodstream, with the heart and kidneys most often affected.
These diseases will require surgical or general systemic treatment - in no case should they be allowed to appear.
Prevention of pulpitis
The following rules will help to significantly reduce the risk of pulpitis, but they must be followed carefully:
- Treat all oral diseases in a timely manner, especially caries and gum disease.
- Pay close attention to your overall health and treat any infections as soon as they are identified.
- Brush your teeth well every day, and have your teeth professionally scaled by your dentist as needed.
- Attend routine preventive examinations at the dentist every six months. By the way, such examinations once every 6 months are free of charge.
- Treat your teeth in a reliable, trusted place to minimize medical errors and complications after treatment.