Impacted is a tooth that has not erupted and is located in the bone tissue, covered by the gum. Dystopic teeth are those that have an abnormal position - that is, they are shifted towards the cheek or tongue, rotated around their axis or tilted to the side. At the same time, some teeth can be either impacted or dystopic - that is, they are located in the bone, while being turned to the side relative to the correct vertical position. This mainly concerns “wisdom teeth” or molar eights, which are located at the very end of the dentition.
Why do wisdom teeth grow incorrectly?
Wisdom teeth, or the outermost teeth in a row, usually appear between the ages of 18 and 25. And they grow, as a rule, with serious disturbances. Only the lucky ones can boast of straight and evenly grown “eights”. Frequent problems of wisdom teeth are retention and dystopia, in most cases even both ailments at once.
The abnormal growth of wisdom teeth is explained by the fact that, firstly, they grow in adulthood, when the bone tissue is fully formed, it is very dense and hard - naturally, it is incredibly difficult to “break through” it. Secondly, modern man does not need eighth teeth - our ancestors used them to chew raw meat. Wisdom teeth don’t even have guides—baby teeth—so they have to make their own way through hard bone.
In most cases, wisdom teeth must be removed, especially if they do not appear above the gum and interfere with neighboring teeth (press on the roots of their neighbors on the side). It is also very important to check the condition of impacted wisdom teeth if you experience discomfort when opening and closing your jaw, pain in the ear, or an increase in body temperature.
Removal of impacted and dystopic tooth
An impacted wisdom tooth can be in a straight or rotated position (dystopia) - in this case it will put pressure on the roots of its neighbor. To avoid complications, such ungrown teeth must be removed. How is the operation performed? In several stages:
- mandatory administration of anesthesia: tooth extraction is a painful operation that requires serious tissue anesthesia,
- the gum is cut - access is created to the impacted tooth,
- a hole is created in the bone using a bur,
- tooth extraction: the tooth is removed immediately using forceps, or is first divided into parts using a bur and then removed from the bone tissue,
- the bone is restored: in some cases, the cavity vacated by the tooth is filled with artificial bone material, or with the patient’s own blood plasma - this measure is necessary so that empty space does not form in the bone, which can be occupied by neighboring teeth. If they begin to shift, then the entire dentition will gradually “creep” - gaps will appear between the teeth. In order to understand whether the hole will need to be filled with any material, you need to consult a doctor,
- the gum is sutured: after all manipulations are completed, the gum is returned to its place, sutures are placed on top.
The operation to remove an impacted / dystopic tooth lasts about 30 minutes to an hour. This is a fairly ordinary operation, which, when performed professionally, will not lead to any complications. In some cases, if there are a lot of uneven roots, it may take longer. The doctor can determine the approximate time of the operation based on the results of examining the image.
Complications after wisdom teeth removal
Unerupted teeth are sometimes located quite deep in the bone, so extracting them can be quite a difficult procedure and can lead to certain complications. For example, a nerve injury in the lower jaw, resulting in numbness of the lips, tongue and part of the cheek (goes away on its own after a few weeks or months), rupture of the nasal sinus (a runny nose or sinusitis forms). With complex removal of wisdom teeth, there is a high probability of fracture of the jaw, adjacent teeth or dentures. In order to avoid such complications, it is best to have wisdom teeth removed by an oral and maxillofacial surgeon who has extensive practical experience in this field.
Care after wisdom teeth removal
After removal of impacted wisdom teeth, minor pain, bleeding from the wound, and rarely, suture separation may occur. Tissue swelling and pain when chewing food and opening the jaw are also observed. If the pain does not go away within 2-3 days (at this time it is necessary to take painkillers - these can be Ketarol, Ketanov, Nise, etc., depending on the prescription after the operation), you must consult a doctor. In general, rehabilitation takes from 1 to 5 days. After a few days, you must visit a doctor for a follow-up examination of the results of treatment and removal of stitches.
What are the signs to determine tooth ankylosis, and what to do with it - whether it needs to be treated or not
In dentistry, a diagnosis such as ankylosis is often made, but it usually refers to the jaw joint. However, dental ankylosis also occurs, the treatment of which is successfully carried out in adults and children. But sometimes people do not rush to the dentist if they have dangerous symptoms, and then treat the complications. To prevent this from happening, we offer you to read material on the topic of dental ankylosis - what causes it, who is at risk, and how treatment is carried out.
What kind of pathology is this
The word "ankylosis" comes from Greek and means "bent." And in relation to a tooth, this is expressed not in the fact that it is bent, but in the fact that it is motionless and even fused with the bone socket. As is known, normally between the tooth root and the walls of the socket there is a thin layer of ligamentous apparatus - periodontal tissue, which also acts as a shock absorber when the tooth moves minimally during chewing food. With ankylosis, this layer atrophies (or is absent altogether), and as a result, cement from the surface of the tooth root tightly fuses with the bone on the surface of the socket. You can see what the smile of a patient with dental ankylosis looks like in the photo.
Good to know! The disease “ankylosis of the tooth” should not be confused with ankylosis of the jaw or ankylosing spondylitis. Ankylosing spondylitis or ankylosing spondylitis is a chronic inflammatory process in large joints (mainly the spine, legs, arms). This disease is incurable, but with the help of modern medications, negative symptoms can be successfully relieved.
What will the doctor do?
If you suspect the presence of a fragment, the doctor:
- Conducts a visual examination of the mouth, assesses the condition of inflamed tissues.
- Writes a referral to the patient for x-rays. Examines the resulting image. Any bone formations and particles are clearly visible on it.
- Based on the characteristics of the localization of fragments and their sizes, the tactics for their extraction are determined. If the particles are close to the surface of the gum, they are removed using a special tool. If they are deep, you have to cut through the soft tissue. In any case, the dental surgeon uses anesthesia so that the patient does not feel pain.
- Removes root particles and treats the wound with an antiseptic solution. Puts an antibacterial drug in it.
Soon after the operation the situation returns to normal. Now the tissues can calmly heal and recover.
Why does ankylosis occur?
Experts from the field of dentistry have not yet established the specific cause of tooth ankylosis, but, nevertheless, the factors that can provoke it are known and are presented in the following list:
- genetic predisposition: these may be hereditary parameters of the dental system or individual characteristics of the absorption of substances, bone formation,
- congenital malformations: congenital hypothyroidism, Down syndrome, cleidocranial dysostosis, etc.,
- facial injuries: for example, blows, bruises, chewing hard objects (nut shells, candy, pencils, toys),
- diseases of the ligamentous apparatus - periodontium: if the ligaments cannot recover after inflammation and begin to die, then the root gradually grows into the jaw bone,
- consuming large amounts of calcium supplements: this does not mean natural foods rich in this macronutrient, but pharmaceutical preparations with calcium. Uncontrolled use of such drugs causes pathological ossification of the facial skeleton, incl. in an unborn child and in children under 12 years of age. Therefore, calcium supplements should only be taken on the recommendation of your doctor.
- hypodontia or an incomplete “set” of permanent teeth.
Reasons for the development of pathology
There are two reasons for the development of granulomas on the root of a tooth.
1. Untreated pulpitis. The development of caries leads to the appearance of a deep cavity in the tooth. Pathogenic microorganisms enter the pulp, it becomes inflamed, and severe pain appears. Lack of medical care leads to the gradual death of the pulp. Bacteria penetrate beyond the tooth through root canals. A focus of inflammation appears at the apex of the root. We are talking about periodontitis.
A deep carious cavity in this case is not always observed. Inflammation can develop internally when secondary caries appears under the filling.
2. Poor quality endodontic treatment. Granuloma can develop at the root of a tooth in which root canal filling was previously performed. Usually there is underfilling: the doctor has not completely filled the canals with material. In the remaining voids, pathogenic bacteria develop, and the tissues surrounding the root react with inflammation.
These causes cause most cases of granuloma formation. But there are others, less common:
- poor quality orthodontic treatment;
- previous dental trauma;
- other inflammatory diseases - tonsillitis, abscess, etc.
In the latter case, the infection enters the tissues through the blood or lymph flow.
Ask a Question
Who is at risk
The pathology can manifest itself in children with a primary malocclusion, and in adults with a permanent malocclusion. As for localization, tooth ankylosis can occur both in the lower jaw and in the upper jaw. Moreover, it occurs on chewing teeth (including wisdom teeth) more often than on the front teeth (in the “smile zone”).
It is also worth closely monitoring the condition of the dental system for people with a hereditary predisposition to this disease and those who engage in traumatic sports.
Expert opinion
Emir Romanovich Omerelli
Maxillofacial surgeon, implantologist
Experience: more than 13 years
Impacted wisdom teeth are a “popular” reason for patients to visit dental clinics. In approximately half of all cases, the eighth teeth erupt with problems, and retention is the most common. It is interesting that the age of patients can be different - from 18 years to deep retirement age. It all depends on how much the impacted tooth bothers the patient. However, the sooner the problem is solved, the less problems an unerupted tooth will cause.
After surgery, it is very important to follow the precautions recommended by your doctor: you must refrain from eating for two hours after tooth extraction. For a couple of days, the food consumed should be warm - not too hot and in no case cold. It is necessary to chew on the side opposite to the operation site. You should also avoid physical activity for a while. You can brush your teeth, but as carefully as possible so as not to damage the sutures. Do not forget about the need to take antibiotics and medications that restore the body’s immune system - they will be prescribed by your doctor.
Other jobs
What symptoms can you use to identify the disease?
In most cases, signs of ankylosis can be determined independently. To do this, you need to pay attention to the dentition and find at least one of the following inconsistencies:
- the causative tooth looks shorter than the others: since its root is not surrounded by periodontal tissue, it is as if “recessed” into the jaw,
- the baby or permanent tooth has not fully erupted,
- eruption is very slow
- neighboring teeth are inclined towards the causative (ankylosed) one,
- the milk one “sits” firmly in place and does not fall out for a long time, although in terms of timing it is high time for it to be replaced by a permanent one,
- The permanent tooth has erupted on the side of the milk tooth: in this case, eruption may be accompanied by severe pain, because there is simply not enough space for the permanent one.
All of the above symptoms are more characteristic of children, while adults can walk for years with an ankylosed unit of the dentition and not attach any importance to it - because it is not always strongly “recessed” into the jaw and does not cause discomfort.
Complications of tooth ankylosis
If the problem is ignored, subsequent treatment can become longer, more traumatic and more expensive. Therefore, at any age, if ankylosis is detected, you need to contact a dentist - we’ll tell you which one later. Now let’s look at what consequences can arise due to ankylosis of even one tooth:
- difficulty chewing food,
- abrasion of the cutting edges of the incisors,
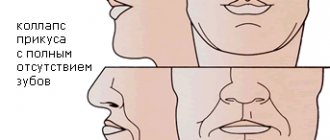
- malocclusion: for example, crowding, retention and dystopia (when the tooth does not erupt completely or in the “wrong” place - on the side, on top of the row),
- caries in places where crowded teeth touch,
- pushing forward the antagonist tooth, which is located on the opposite jaw and comes into contact with the ankylosed one when closing the mouth: as a result, it is less fixed in the bone, may begin to wobble or even fall out,
- injuries in the oral cavity: when the elongated antagonist scratches the opposing teeth and gums.
Causes of dental ankylosis
Heredity. The vast majority of cases of the disease are of genetic origin, that is, parents who have had similar problems have a very high chance of having children who will also experience ankylosis. It is recommended that such children undergo more frequent preventive examinations by the dentist in order to detect the appearance of ankylosis in the early stages and promptly eliminate its consequences.
Already existing dental diseases. Ankylosis can develop as a result of periodontal disease, as well as hypodentia - the absence of one or more teeth. In this case, the development of ankylosis is not limited to childhood or adolescence and often occurs in adult patients.
Hit. Some cases are traumatic in nature: bone fusion of the tooth root with the alveolar tissue occurs against the background of partial or complete dislocation of the tooth, which led to the death of the periodontium.
Chemical exposure. The use of products containing resorcinol-formalin in pediatric dentistry can lead to disruption of the process of root resorption and subsequent delay in the replacement of temporary teeth with permanent ones.
How is diagnostics carried out?
First, the doctor examines the patient’s oral cavity, conducts a survey, and listens to complaints. The condition of neighboring teeth and antagonists is also assessed for displacement and enamel abrasion. Ankylosis of a tooth is usually clearly visible on an x-ray; both a classic targeted X-ray and a more informative computed tomography can be done1.
Read on the topic: methods and techniques for performing x-rays in dentistry.
An x-ray shows the absence of a periodontal fissure, which normally looks like a dark thin strip about 0.2 mm wide between the root and the walls of the alveolar socket. After diagnosis, suitable treatment is suggested.
On a note! Children should be taken to an orthodontist for a preventative visit at the age of 5-6, even if there are no visible malocclusions. Because to diagnose hidden pathologies, the doctor will definitely prescribe a panoramic image, which can also be used to identify ankylosis.
Treatment in children
Ankylosis in the primary occlusion in the presence of pain and other dangerous symptoms is an indication for removal. If there is no discomfort, removal is not required, but the situation should still be monitored through regular visits to the dentist. When the permanent tooth has already formed and is close to the roots of the milk tooth, the latter should be removed. If the permanent one has erupted in the gum from the side, then the milky one is also removed to prevent complications.
On a note! Braces cannot be placed on a tooth with ankylosis, either in children or adults. Since correction with braces is possible when the periodontal ligaments are preserved in normal condition. And the ankylosed unit of the row simply cannot be “stretched” with braces, because it is immovably fused with the bone.
Treatment in adults
Adult patients should know that in most cases it is possible to do without serious intervention and without removal (if there are no direct indications for this). To restore the aesthetics of a smile with a slightly shortened crown, you can build it up with a filling or install a veneer. In the case of a very shortened tooth apex, it is better to place an artificial crown - made of ceramics in the frontal part of the row or from zirconium dioxide (can be made of metal-ceramics) in the chewing areas.
“The eldest didn’t get a double for a long time. The opposite one was replaced in time, but this one didn’t even think about staggering. I took her to the dentist and they took an x-ray. And it turned out that the root had fused with the bone, hence all the problems. The doctor immediately explained to me that it was necessary to remove it with an injection ((My daughter was afraid of injections, of course, but it was okay, she endured it, and the tooth was removed quite quickly."
Svetlana Nikulina, review from the woman.ru forum
If an adult still had to have a tooth removed due to ankylosis, then one should think about prosthetics or implantation. Moreover, the last option is preferable, because the implant restores the tooth root – i.e. There will be no loss of bone tissue at the site of the defect.
Read on the topic: what is implantation, how is it carried out and who is suitable for it.
If you install a classic bridge, then, firstly, you will have to depulpate and grind down the teeth on the outermost part of the defect, which will become a support for the bridge and will collapse from the load in 5-10 years. And, secondly, the absence of a root at the site of the defect “disables” the jaw bone in this area. The bone, left without chewing load, sags, and along with it the level of the gum decreases, and a gap forms under the denture.
Preservation of teeth with root fractures
Primary root fractures (PRF), traditionally referred to as “vertical root fractures,” are defined as “a complete or incomplete fracture that occurs in the root region of a tooth at any level, and is usually in a buccolingual direction.” It is logical that this definition of PPC is based on its anatomical location.
Since almost all teeth with PCD are pre-treated endodontically, it is reasonable to assume that there is some connection between the characteristics of endodontic intervention and the development of PCD. Based on the nature of the occurrence of PPC, the following definition was proposed: “a complication of endodontic treatment, which is characterized by complete or incomplete fracture of the dental tissues, begins in the root structure at different levels, and usually spreads in the bucco-lingual direction.” It is fundamentally important to understand that although PPC is a complication of endodontic treatment of a tooth, this does not indicate that PPC is directly related to any type of medical error during the procedure. And although treatment errors can lead to complications in the form of a fracture, not all root fractures are caused by procedural errors by the dentist, and some of the fractures develop even after completely adequate root canal treatment. Considering that PPC develops both among teeth after high-quality endodontic intervention, and in the structure of teeth after poor-quality canal treatment, we can conclude that the expanded definition of PPC includes both purely clinical and medical-legal aspects of assessing the quality of endodontic interventions.
The prevalence of PPC reaches 11-30%. A recent study by Yoshino et al in 2015 found that high prevalence of PPC was the leading cause of removal of endodontically treated teeth. In an analysis of 736 teeth from 24 different clinics, the authors were able to determine that 626 of them were extracted within 6 months after treatment, while 233 teeth were extracted as a result of the diagnosis of PPC (31.7%). Anatomically, RPCs often develop lateral to the root canal wall toward the outer root surface. Incomplete fractures extend only on one side of the root surface, while complete fractures extend in both directions, affecting two surfaces. Occasionally this leads to the root splitting into separate segments.
Timely diagnosis and proper treatment of such complications are crucial to prevent loss of alveolar bone, which can complicate further manipulations, including the possibility of dental implantation. However, the clinical and radiological diagnosis of PPC is quite difficult, and in some cases, the correct diagnosis can only be made through direct visualization of the root after surgical separation of the flap (Figure 1).
Photo 1. Diagnosis of tooth root fracture during direct imaging after flap separation.
Traditionally, teeth with PCD were considered hopeless from the point of view of functional prognosis. Possible treatment approaches for PPC have included tooth replantation after bonding the two fractured segments, but such approaches are not sufficiently evidence-based to be implemented in daily clinical practice. Therefore, the remaining treatment alternative was extraction.
For many years, there has been an ongoing debate among clinicians about whether it is worth trying to preserve a compromised tooth as much as possible, or whether it is better to remove it and immediately proceed to the dental implantation stage. In recent years, given the level of prevalence of peri-implantation complications, it has been suggested that the treatment of one’s own teeth, even those compromised by a fracture, is simpler and more predictable compared to the treatment of peri-implantitis, the problem of which continues to progressively increase in modern dental practice.
In recent years, a number of new algorithms have also been proposed, including promising alternatives for the treatment of teeth with PCD, which until now have traditionally been referred to extraction. These unique single-unit treatments for teeth with root fractures are in the early stages of development and refinement, and data on them are mainly based on single publications. However, modern endodontics offers a number of technical means such as devices for magnification and lighting, as well as a set of modern materials such as bioceramic cements, which expand the possibilities for the restoration of teeth with root fractures with the correct selection of appropriate clinical cases with a clear understanding of the difference between which tooth can still be saved and which can no longer be saved. This article will discuss modern possibilities for treating teeth with PPC.
The importance of choosing a clinical case for treatment
Modern endodontics provides many treatment options that can save compromised teeth. However, PPC still poses a diagnostic and therapeutic challenge for dentists, as root fracture is the reason why most endodontically treated teeth have to be removed. In addition, with the development of modern endodontic treatment options, new dilemmas have emerged regarding the functional prognosis of treated teeth. The topic of discussion remains the decision about the possible preservation of a compromised tooth with PPC or its extraction with restoration of the edentulous area using a dental implant. Traditionally, it was believed that the sooner a tooth with a root fracture is removed, the better, because the presence of one in the jaw provokes the development of inflammation, which, spreading to the periodontal area, provokes the formation of a destructive bone defect. Under such conditions, bone loss, in turn, compromises the prognosis of the future implant, which can be installed in place of the problematic tooth. However, each individual clinical case should be assessed objectively, since some data have shown that with an adequate selection of a suitable clinical situation, teeth affected by a root fracture with a limited distribution do not provoke the development of inflammation in the surrounding periodontium over a fairly long period of time. The selection of clinical cases of PPC suitable for conservative treatment should be based on evidence-based protocol data, taking into account the completeness of the diagnosis and available therapeutic options.
The dentist must also take into account the aesthetic needs of the patient, the duration of functioning of the treated tooth and the costs required for its restoration. When making decisions about possible conservative treatment of teeth with PCD, one should take into account not only endodontic aspects, but also periodontal, prosthetic and aesthetic components of the patient’s rehabilitation. Many factors, such as the location of the tooth, the presence of predisposing periodontal disease, the type of coronal restoration and the possibility of using modern endodontic materials and instruments, must be taken into account by the doctor when assessing the risks and benefits of conservative treatment of teeth with a root fracture.
In cases of development of PKD in multi-rooted teeth, there may be no need to preserve the root with a fracture, since it can simply be amputated. With single-rooted teeth, the situation is different, and the functional prognosis of such teeth depends on the adequate choice of treatment method. Predisposition to periodontal pathology negatively affects the prognosis of teeth with PCD. Thus, during the initial diagnosis of teeth with root fractures, it is necessary to carefully assess the presence and severity of possible adjacent periodontal lesions.
The inability to preserve a tooth (even if one with a root fracture) in the dentition significantly reduces the patient’s aesthetic profile. And although in most clinical cases implants take root absolutely without problems and serve successfully for many years, the long-term prognosis of such implants must also necessarily include the parameters of the achieved aesthetic rehabilitation. After all, if disintegration of the implant occurs in the frontal area, then the aesthetic profile of not only the immediate area of implantation is disrupted, but also the entire aesthetic profile, which is subsequently quite difficult to correct.
It should not be forgotten that in cases of preservation of teeth with PCD, gum recession and alveolar loss of surrounding bone tissue often develop in the area. Especially often, such symptoms develop in patients with a thin biotype of periodontal tissue. Thus, a thorough assessment of aesthetic and periodontal parameters should be a mandatory component of planning a comprehensive treatment algorithm for patients with PPC.
The long-term prognosis of the functioning of treated teeth with PCD is also influenced by prosthetic parameters: for example, the crown-to-root ratio, the amount of vital tooth structure and the presence/absence of tooth ferrule. In fact, adequate crown restoration is another of the most important factors affecting the survival of a tooth after treatment. In addition, due to the absence of pathognomonic radiographic signs or clinical symptoms of PPC, the prognosis of the future functioning of the compromised unit of the dentition can only be assessed after completion of the restoration of its coronal part with an appropriate superstructure.
Treatment Alternatives
If preserving a tooth with PCD is the initial goal of complex treatment of the patient, to achieve this goal, the doctor can use a number of surgical and conservative approaches, including root amputation or hemisection, apicoectomy with resection of the fractured root coronally relative to the fracture line, performing a replantation procedure, flap separation and restoration areas. Despite the variability of approaches over the past decades, there has been a change in the trend towards the subsequent effect after treatment: if previously the majority of treated teeth with PCD eventually had to be removed, now their survival rate has increased throughout the entire monitoring period.
Root amputation or hemisection
When diagnosing PPC in a multi-rooted tooth structure, the most logical treatment option is surgical amputation of the fractured root. About a hundred years ago in 1884, Farrar proposed a surgical approach that involved resection of one of the roots of the problem tooth and filling the endospace of the remaining one. At the same time, Farrar performed root resection at different levels in different clinical cases, thus sometimes leaving only a short “snip” of hard tissue in the gums (photo 2).
Photo 2. Root amputation procedure during endodontic surgery.
a. The patient had a fistula in the area of the upper molar. After diagnosis, a diagnosis of chronic apical abscess was made. b. During the surgical procedure, the mesiobuccal root was removed. c. Two years after the operation, the tooth showed no symptoms, and the presence of replacement hard tissue was noted in the amputation area.
In their study, Anitha and Rao (2015) reported that the root resection procedure to remove the cracked root fragment is completely predictive of the relative prognosis of the remaining tooth. But again, to achieve successful results of the intervention, you need to carefully approach the selection of a clinical case, taking into account the condition of the periodontium and the design of the future prosthetic structure. Depending on the specific clinical conditions, the resection procedure has several subtypes and modifications, for example, the resection can be extended to include part of the crown, and in some cases it is carried out together with orthodontic extrusion of the remaining part of the tooth. Root amputation, or hemisection, is more indicated for upper or lower molars in cases where only one of the roots is broken. Taking into account the condition of the periodontium and the location of the fracture line, resection can be performed at different levels, and sometimes it is possible to preserve even the coronal part of the root, which is subsequently filled. In cases of fused roots, amputation is not recommended. It should also be noted that although root amputation can be performed in mandibular molars, hemisection or resection is a more predictable procedure for these teeth. The large length of the root and the short distance between the teeth in the area of their furcation negatively affect the surgical prognosis of resection, since in such cases the implementation of this procedure is purely technically complicated.
Cementation of the root fracture area with further replantation
Many case reports have reported attempts to cement the root fracture site followed by tooth replantation, which have shown fairly variable results with long-term monitoring. Hayashi et al in 2004 described a case of treatment of PPC by restoring the fracture site with a composite bonded to the tooth wall, after which the latter was replanted back into the socket. In 18 of the 26 cases analyzed, the teeth continued to function successfully for another 4-76 months. At the same time, the authors noted that the treatment of teeth with a fracture that extended more than two-thirds of the length from the neck of the tooth to the apex area, as well as the restoration of distal teeth, is less successful compared to other clinical cases.
Nizam et al 2021 evaluated the results of 21 replanted teeth that were preextracted and restored in the PPC area with resin cement. After replantation, all teeth were splinted to adjacent teeth. The authors reported that out of 21 treated teeth, 2 were extracted within the first month after treatment. The values of periodontal indices (plaque index, gingival index, probing depth and clinical attachment level), as well as periapical index (PAI) in the area of the treated teeth 12 months after surgery were significantly lower compared to the initial situation. Taking into account the data obtained, the authors summarized that performing adhesive cementation and deliberate replantation of teeth with PPC can be relatively effective only in cases of treating single-rooted maxillary teeth.
Kawai and Masaka 2002 proposed a modified method for replanting teeth with PCD after restoring the fracture site by rotating the tooth 180 degrees from its original position. In this way, it is possible to reposition the fracture line below the level of the bone covering and periodontal ligaments, minimizing the risk of complications. Other authors (Hadrossek and Dammaschke 2014) have presented cases of retrograde root filling with fracture using calcium silicate cement (biodentine).
Although intentional tooth replantation may be considered a predictable treatment option in some clinical cases, restoring the fracture line with any material is itself a controversial therapeutic approach. Indeed, for such treatment, the tooth must first be extracted, without provoking any segmentation of it into parts during removal. The aspect of the development of resorption after replantation also remains problematic. Thus, a contraindication to replantation is a condition of the teeth in which they cannot be safely removed, or their periodontal status is compromised. Also, such manipulation is not recommended for patients with severe somatic diseases.
Cementation of root fracture after flap separation
More than two decades ago, Selden (1996) described the treatment of teeth with incomplete PCDs using glass ionomer cement and bone graft. Ultimately, however, the author reported that all six cases treated in this manner ultimately failed. At this time, using the capabilities of lighting and magnification, the doctor has a wide range of methods for working with the root system of the tooth, which allows achieving high accuracy of iatrogenic interventions. Modern endodontic materials, such as mineral trioxide aggregate (MTA), have been repeatedly used by doctors to restore root fracture sites. The protocol for this treatment involves creating a groove along the fracture line, which is subsequently sealed with MTA. Taschieri et al in 2010 analyzed the results of treatment of maxillary anterior teeth that were diagnosed with a root fracture. Teeth with deep periodontal pockets and radiographic evidence of periapical lesions were excluded from the study. During treatment, the flap was separated; a groove was formed along the fracture line with an ultrasonic instrument, which was then filled with MTA. The existing bone defect was filled with calcium sulfate material. After 33 months, 5 of the 7 initially treated teeth showed successful results, while the remaining 2 had to be removed during monitoring. Floratos and Kratchman in 2012 tried to treat 4 distal teeth with a similar intervention. After separation of the flap, the authors performed an oblique resection of the root, and its residual part was filled with MTA. The osteotomy area was covered with a collagen membrane, and the treated teeth were observed for 8-24 months. The results obtained were classified as successful (Floratos and Kratchman 2012). In a recent study, Taschieri (2016) reported a case of treatment of a maxillary left central incisor in which an incomplete root fracture was diagnosed. After separation of the flap, the doctor confirmed the presence of a fracture. The broken part of the root was removed and the defect area was filled with platelet-rich plasma. After 24 months, the tooth remained asymptomatic. The authors suggested that a similar surgical approach could be successfully used in the treatment of endodontic-periodontal lesions associated with incomplete PPC. Although most reports show promising results, flap separation itself carries the risk of possible gingival scar formation and the potential risk of further recession. Also, such manipulation can provoke excessive bone loss in the surgical area. Given such complications, before carrying out such manipulations, the potential risks should be carefully assessed, especially if the intervention is carried out in an aesthetically significant area.
conclusions
In order to decide what to do with a tooth that has a root fracture, you need to take into account a number of specific factors that affect the success of a possible treatment algorithm. The choice, in fact, is simple - the tooth can either be removed and the edentulous area can be restored with an implant, or the tooth can be tried to be saved. Despite the fact that extraction of teeth with root fracture remains the method of therapeutic choice, new endodontic instruments and materials allow the doctor to compete for the prognosis of the problematic unit of the dentition. To formulate any evidence-based conclusion about the algorithm for choosing an appropriate method of treating teeth with PPC, a number of additional studies are required that will make it possible to unambiguously assess the prognosis of the functioning of restored teeth in the long term.
Authors: Eyal Rosen, Ilan Beitlitum, Igor Tsesis