Fracture of the lower jaw - symptoms and treatment
Diagnosis of patients with fractures of the lower jaw is carried out in order to establish the location, number of fractures, as well as to determine injuries to nearby tissues, vessels and nerves.
Diagnostic methods are basic and additional (instrumental).
Basic diagnostic methods are carried out with a standard set of instruments in the emergency room, dental office or dressing room. The doctor finds out the patient’s complaints, learns about previous diseases and previous operations. At this stage, it is very important to establish the time of injury, since the duration of the injury plays a big role in further treatment tactics.
During the investigation, the doctor will find out whether the injury was sustained at home, at work, or during a fight, and whether it is of a criminal nature. In case of injury during violent acts, the doctor is obliged to report the incident to the police. After that, an internal affairs officer talks with the victim, finding out the details of what happened. In this regard, there is often a concealment of the real reasons for the injury, and the patient sometimes invents very ridiculous and implausible stories.
Sometimes collecting complaints and medical history is difficult or impossible due to the patient’s serious condition or alcohol/drug intoxication.
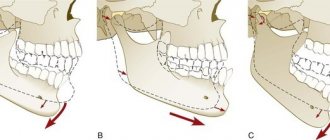
A clinical study begins with an external examination; post-traumatic swelling, changes in skin color, the presence of abrasions, hematomas, and bleeding are detected. Next, palpation is carried out, during which the nature of the swelling is revealed, inflammatory infiltrate, hematoma, and subcutaneous emphysema are excluded. Palpation of the lower jaw is carried out symmetrically, starting from the branch of the lower jaw and ending in the chin. The presence of a bony step indicates a fracture of the mandible. The degree of mobility of the fragments and the direction of their displacement are also determined.
When examining the oral cavity, special attention is paid to the mucous membrane of the alveolar part of the lower jaw, identifying violations of integrity and bleeding. The relationship of the dentition and the displacement of the central line of the lower jaw when opening and closing the mouth are determined. The landmarks are the labial frenulum, the line between the central incisors of the upper and lower jaw.
Often, the opening of the mouth with jaw fractures is limited. When rocking the lower jaw, relying on the chewing teeth and the basal edge, you can determine the degree of pathological mobility of the lower jaw and the location of the fracture.
Additional diagnostic methods:
- X-ray : an X-ray of the skull is taken in a direct projection in order to exclude fractures of other parts of the face and an X-ray of the lower jaw in lateral projections, the number of fractures, the presence or absence of displacement, diastasis (gap) and the presence of teeth in the fracture line are analyzed.
- An orthopantomogram is a more modern method, with functionality similar to an x-ray. One detailed image is taken, and it is possible to view it on the monitor screen using various programs.
- Computed tomography allows you to most accurately identify fractures of the lower jaw, measure the distance of displacement of fragments, diastasis, determine the size and number of fragments, and the presence of foreign bodies. Using certain setting modes, you can determine the violation of soft tissues (muscles, blood vessels, nerves) and the presence of hematomas.
- Assessment of the general condition of the body - examination of organs and systems of the body, identification of viral and chronic diseases. For this purpose, a physical examination, digital chest x-ray, ultrasound examination, and laboratory diagnostic methods are used. If necessary, consultations with related specialists are carried out. All this helps to select the most effective therapy for the patient, taking into account the characteristics of a particular clinical case.
Maxillary fracture
A fracture of the upper jaw can only be open and is dangerous because the upper facial jaw is close to the cavities of the mouth, nose, eyes and brain. As a result, the injury can be complicated by meningitis or inflammation of the maxillary sinuses.
The main symptom by which one can judge a fracture is pain in the middle of the face, which becomes stronger when trying to close the jaws. External signs also indicate a fracture of the upper jaw: the mouth cannot be closed, the face is elongated, and bleeding comes from the nose and mouth.
Very often, an injury to the upper jaw is accompanied by a concussion, injury to the base of the skull, which leads to dizziness, nausea, headache and memory loss. A strong blow to the face, an accident or a fall from a height can result in a fracture of the processes of the jaw, usually the upper one - in this case the bones that support the teeth are damaged.
Before surgery
- Prepare an ice pack at home.
- On the day of surgery, eat a light meal 2-3 hours before your scheduled time.
- The day before surgery, the consumption of alcoholic beverages is strictly prohibited.
- Be sure to inform your dentist about all the individual characteristics of your body and any allergic reactions, in order to accurately select an anesthetic that is safe for you.
- Visit the toilet before surgery.
- It is better to come to the operation in loose clothes without a collar.
How to speed up bone healing after a fracture?
When it comes time to heal a broken bone, our body usually knows what to do.
But in some cases, fractures heal very slowly or show no signs of healing at all for a period of time. However, the process of bone healing after a fracture can be accelerated by following certain recommendations. The healing process of a broken bone
Before moving on to the recommendations, let's look at the process of repairing a broken bone.
Stage 1: inflammation
When a bone breaks, the body sends white blood cells to the fracture site to remove foreign substances from the fracture from the blood. This causes inflammation, which stimulates the growth of new blood cells and is the first stage of recovery.
Stage 2: soft callus
The next step is for your body to create a callus around the fracture to cement the broken bone. This callus is just fibrous tissue and gets rougher over time.
Stage 3: hard callus
Gradually, the body replaces the soft callus with a hard callus that connects the bone fragments more firmly. This hard callus, which creates a lump at the fracture site, can be seen on x-rays several weeks after the fracture.
Stage 4: remodeling
The final stage of the bone repair process is remodeling, where the body replaces the callus with new, more compact bone. Remodeling makes bones stronger and improves blood circulation in bone tissue.
When a bone is fractured, doctors take certain actions aimed at achieving proper and rapid restoration of damaged tissue:
- Setting the bone in the correct position and immobilizing the fracture. If necessary, the doctor will move the displaced bone segments back into place, after which the bone will be immobilized using a cast or brace.
- Operation . In some cases, patients need surgery to replace bone fragments and stabilize the fracture, a process that may use metal plates, screws or nails. If the fracture does not show signs of healing, additional pressure is necessary. Sometimes doctors choose to do additional surgery. With the advent of the Exogen device, reoperation has an alternative that can accelerate bone healing even with non-union fractures.
- Stimulating bone growth. To help the fracture heal, you can use the Exogen device, the only stimulator that uses ultrasound waves to stimulate the body's natural healing processes, activating bone growth.
- To speed up metabolism and, accordingly, restore injured tissues, physiotherapeutic devices can be used. For example, a fracture is an indication for the use of MILTA or RIKTA laser therapy devices.
- Rehabilitation after a fracture. A fracture involves long-term fixation of the bone in order to allow the tissues to heal properly. A negative effect of prolonged immobilization may be loss of joint mobility, in other words, the occurrence of contracture. One of the reasons is that injured tissues are restored in a fixed position, which subsequently does not allow the joint to fully bend.
Doctors recommend actively developing the joint after removing the plaster or fixing orthosis using special exercises or mechanical therapy devices Artromot or Kinetek, which independently bend the joint and gradually stretch the soft tissue. If the joint has been in a fixed position for a long time (more than 1-2 months), mechanotherapy is supplemented with manual or hardware techniques aimed at increased flexion of the joint, accompanied by microtears of tissue. In the future, it is important that tissues that have undergone micro-tears are restored through movement.
In addition to developing joint mobility, it is important to restore muscle tone using special exercises or myostimulation.
Find out more about exercises for rehabilitation after knee injuries and operations on the knee and knee joint, as well as about exercises for rehabilitation after shoulder injuries and operations on the shoulder and shoulder joint
Additional Tips
Avoid lifting heavy objects, bending over, playing sports, or taking hot baths for 5 to 7 days after surgery.
Within a few days, performance and the ability to drive may be reduced.
Remember to take medications prescribed by your dental surgeon after surgery.
We kindly ask you!
Appear for examination and removal of stitches 5-7 days after surgery, in agreement with your surgeon. You must immediately notify your surgeon or clinic administrator of any changes in your health.
Recommendations for caring for dental implants
The service life of the implant depends on:
- The correctness of the surgical and prosthetic stages carried out in the dental clinic.
- The patient's compliance with the recommendations given by the dentist immediately in the postoperative period and the period after implant prosthetics.
- Careful hygienic care of the “implant-crown” structure.
- Blood supply to bone tissue and gums in the area of implantation. (Smoking cigars and cigarettes has a very, very negative effect on peripheral blood circulation, which can even interfere with implant implantation.!!!)
Types of teeth splinting
The teeth are connected into a single block using a rigid fastening structure - a splint, which can be either stationary or removable. Any tire must meet the following requirements:
- do not injure soft tissues;
- do not complicate oral hygiene;
- be hypoallergenic;
- do not cause difficulties with eating;
- do not violate diction;
- be resistant to mechanical loads.
It is important that when splinting, more healthy teeth fall into the coverage area of the structure - this will relieve the diseased teeth and allow them to “rest.” If the entire dentition is mobile, the splinting procedure will be less effective.
Since the splint makes it possible to distribute the chewing load, the more units of the dentition are involved in it, the more effective the therapy will be. Splinting the front teeth is most effective. When installing a splint on molars and premolars (on the sides), the teeth are splinted symmetrically on both sides and then connected with a bridge. This is necessary for additional strengthening, since a linear structure is much less stable than an arched one.
According to the duration of wearing, splints are divided into 3 types:
- Temporary – up to 3 months;
- Long-term – from 3 months to 1 year;
- Permanent – longer than 1 year.
The type of tire and the duration of its use depends on the task that this system solves at this stage.
For example, splinting teeth for periodontitis is performed as part of the treatment of this disease. This means that the condition of the dentition can change, both for the better and for the worse. For example, the loss of one or more teeth due to periodontitis is not uncommon. After this, it is necessary to change the shape of the structure taking into account the missing units. Therefore, temporary splints are usually used during intensive treatment.
Temporary structures must:
- not be too expensive;
- do not interfere with doctors performing medical procedures;
- subject to modification during treatment.
Permanent splints are needed as maintenance therapy.
To these are added the requirements of aesthetics and high wear resistance. However, periodontal diseases are characterized by relapses, therefore, even when using a permanent structure, it is desirable to be able to modify it.
Long-term systems are a kind of compromise between a temporary and a permanent bus. They are installed if remission is achieved, but there are doubts about its durability. Splinting of teeth can be performed:
- threads;
- removable dentures;
- crowns;
- tabs.
Temporary and long-term splinting is usually performed with threads, and permanent splinting is performed with prostheses.
Types of possible complications
With fiberglass and cable-stayed splinting, the following unpleasant consequences are possible:
- Damage to the pulp due to drilling too deep for the tire. This leads to the development of pulpitis - inflammation of the nerve, and requires depulpation of the tooth and filling of the canals.
- Allergic reactions to the material.
- Reduction in enamel thickness after professional cleaning and etching of dental tissue. In this case, sensitivity to cold and hot develops.
- If there is insufficient brushing before the procedure, bacteria may remain on the teeth. Once they begin to multiply under the tire, they lead to the development of caries and pulpitis. This requires removal of the splint and treatment of the teeth.
- Inflammatory processes of the mucous membrane near the splinting area.
Treatment of a jaw fracture
Before treatment, an X-ray of the jaw and neck must be taken to confirm the diagnosis. Treatment consists of antiseptic treatment of the open wound, stopping bleeding, comparing fragments and bones, and immobilizing the jaw. In order for the bones to heal, a splint is placed on the jaw. How long a jaw fracture takes to heal depends on the severity of the injury; most often the splint is removed after a month and a half. Then the motor functions of the damaged jaw are restored.
Stopping bleeding:
To control bleeding, it is necessary to bite down on a gauze pad placed by the dentist in the oral cavity. The pressure promotes the formation of a blood clot in the socket. If you have heavy bleeding that has not stopped within an hour of tooth extraction, you should bite into a regular tea bag. Tannin in tea helps in the formation of blood clots. Hold the tampon or tea bag until the bleeding stops.
Additionally, cool the extraction area, apply a cold compress to the face in the area of tooth extraction for 10-15 minutes. at one o'clock. A slight bleeding on the first day after removal is normal.