Leukoplakia is small areas of altered mucous membrane, most often the pathology occurs in the oral cavity and genitals, but is possible in any organ lined with mucous membrane: in the stomach, on the eyelids, in the nose. At its core, leukoplakia is a precancer with the potential for malignant transformation.
- Causes of leukoplakia
- Classification of leukoplakia
- Localization of leukoplakia
- Symptoms of leukoplakia
- Diagnosis of leukoplakia
- Treatment of leukoplakia
- Treatment prices
- Prognosis for leukoplakia
- Disease prevention
Leukoplakia is an area of dense surface epithelial cells. Normally, the upper layers of the skin and mucous membrane regularly and painlessly die and slough off. With hyperkeratosis, a variant of which is considered leukoplakia, the process of removing dead cells is disrupted, keratinized cells remain in place, forming a multilayered whitish island.
Causes of leukoplakia
What exactly causes leukoplakia is not known. A cause-and-effect relationship with long-term local inflammation is assumed, because in some cases the pathological area is located directly in the projection of the traumatic factor.
Among the main causes of pathology are long-term trauma:
- mechanical - a fragment of a tooth can injure the mucous membrane of the cheek, a denture can injure the gums; in older women, prolapse of the genital organs with prolapse and eversion of the vagina acts as a traumatic factor;
- chemical injury is caused by toxic tobacco smoke, chewing betel nut and nas, prolonged and uncontrolled use of vaginal gels and estrogen suppositories;
- physical - with frequent consumption of hot drinks and dishes;
- operating room, when scar changes change tissue trophism; this happens after invasive gynecological interventions, for example, coagulation of cervical erosions.
The following factors predispose to the development of leukoplakia against the background of chronic trauma to the mucous membrane:
- hormonal imbalance - age-related involution of the genital organs is accompanied by slight vulnerability of the mucous membranes;
- infection with papilloma virus, Candida fungi, caries;
- generalized infectious process; Pathology is often detected in tuberculosis patients; an example from the history of medicine is leukoplakia in syphilis;
- immunity disorders due to chronic viral infections or natural age-related decrease in the body's defenses;
- metabolic diseases, mainly diabetes, obesity.
Perhaps the initiation of mucosal pathology requires a hereditary predisposition to degenerative processes with the loss of genes that control the process of cell keratinization. This option is suggested by a family history of leukoplakia of the vulva and vagina, but so far reliable genetic evidence for this has not been found.
Reasons for development
The main cause of leukoplakia of the tongue is considered to be the presence of the Einstein-Barr virus in the human body; it is the most common on the planet (at least 95% of the entire population has suffered from the diseases caused by the virus). The agent is transmitted mainly through biological fluids, often through saliva.
No wonder the main pathology it causes, infectious mononucleosis, is called the kissing disease. However, this disease most often affects children and adolescents, while adult patients develop immunity to mononuclear infection by the age of 25.
If a person’s immunity is not reduced, and infection with the Epstein-Barr virus does occur, leukoplakia can be practically asymptomatic, but associated diseases often develop against the background of this pathology. These include lymphogranulomatosis (a malignant lesion of lymphoid tissue) and Burkitt's lymphoma (the hematopoietic system is affected here, and the disease has an extremely unfavorable prognosis).
In addition to the fact that hairy leukoplakia is diagnosed in almost all patients with HIV infection, the following factors can lead to its development:
White coating on the root of the tongue
- abuse of tobacco products;
- tongue cancer;
- blood diseases, such as leukemia;
- regular negative effects on the oral mucosa of ultraviolet rays;
- deficiency of vitamins B and A in the body;
- constant irritation and injury to the soft tissues of the gums, lips, cheeks and tongue due to crooked teeth, crowns, bridges, incorrectly installed braces and dentures;
- autoimmune diseases - HIV, AIDS, rheumatoid arthritis, diabetes;
- hormonal imbalances;
- long-term use of medications that strongly suppress the immune system.
When the Epstein-Barr virus enters the body, especially if the patient is over 45 years old, tends to smoke and has chronic diseases, the immune system becomes defenseless, which leads to active replication of the enemy agent. In such situations, the manifestations of hairy leukoplakia will be striking and will force the patient to urgently consult a doctor.
Pathology can be caused by several types of viruses
Classification of leukoplakia
In ICD-10, leukoplakia is recognized as a non-inflammatory disease, and upon microscopy it is keratoses of varying severity, often with dysplasia - a violation of cell ripening and differentiation.
Translated from Greek, leukoplakia means “white plate”; this name reflects the appearance of the pathological lesion. Not in all clinical situations does leukoplakia look like a plate. Cellular processes do not proceed in the same way: somewhere thickening prevails with significant desquamation, somewhere destruction predominates, therefore leukoplakias are classified by type.
There are several classifications, but all of them highlight:
- simple or flat - this is a spot of cloudy epithelium, as if covered with a delicate and clearly demarcated white film that cannot be removed;
- verrucous - looks like a flat whitish granular wart, rising above the unchanged mucosa and rough to the touch;
- erosive or erosive-ulcerative form, when linear erosions and ulcers with undermined edges that heal poorly are formed on a flat whitish spot;
- soft - with uneven borders, a fringed, patchwork or mosaic-like white spot with patches of maceration of the epithelium, often covered with colonies of fungi in the form of curd masses.
According to WHO classification there are:
- inhomogeneous, that is, of uneven structure, which includes verrucous, spotted, nodular and erythroplakia - a whitish spot with numerous red inclusions;
- homogeneous - structurally homogeneous.
Symptoms
Signs of hairy leukoplakia usually appear gradually and do not have an acute, pronounced character. First, the patient notices the appearance of small folds along the lateral edges of the tongue, which are whitish in color and resemble the surface of a washboard. To the touch, the affected areas differ from healthy mucous tissue; they are rougher and rougher.
If at this stage a person does not seek help from a doctor and does not receive the necessary treatment, then the atypical formations on the sides of the tongue begin to merge into larger areas of lesions, taking on the appearance of plaques without a clear outline. These formations do not cause the patient discomfort, pain, burning or itching, in addition to a pronounced cosmetic defect. Unpleasant sensations may appear when palpating the affected areas of the mucous membrane or when eating too hot or cold food.
In most cases, areas of keratinized tissue on the tongue are located symmetrically, for example, on both sides; less often, the pathological process spreads to the soft palate and the inner sides of both cheeks. This is due to the fact that the patient can for a long time attribute the appearance of fleecy formations to mechanical injuries to the mouth, poor hygiene and other factors.
Localization of leukoplakia
Most often, the pathological focus is localized in the oral cavity and on the genitals of women; it is less common in men. During endoscopic examination, the disease is found in the pharynx and larynx, stomach and rectum.
Typical locations are the clitoris, vagina and cervix, head of the penis, mouth.
On the cervix, the lesion may be located at the external pharynx, where the appearance of the epithelium changes, and near scar changes.
In the oral cavity - on the cheek at the junction of the upper and lower dentition, on the soft palate.
In smokers who do not remove the cigarette until it is completely burned, leukoplakia forms on the red border in the projection of the smoldering cigarette.
Prevention
To date, there are no specific preventive measures for hairy leukoplakia, which is caused by the Epstein-Barr virus. However, measures to prevent infection with any viral infection include the use of barrier methods of contraception, avoidance of promiscuous sexual intercourse and regular blood tests.
Other forms of leukoplakia can be prevented by following these rules:
- regularly visit the dentist, identify and treat inflammatory diseases of the oral cavity;
- install high-quality dental fillings, dentures and braces;
- Take care of your oral cavity regularly, in addition to brushing your teeth, get rid of bacterial plaque using mouth rinses, use dental floss after meals;
- prevent injury to the oral mucosa;
- promptly identify and treat chronic and autoimmune diseases;
- stop smoking and drinking alcohol;
- Do not abuse spicy and salty foods, introduce foods rich in protein and fiber into your diet.
Natural prevention should include measures to strengthen the immune system, such as hardening, playing sports, and walking in the fresh air. It is necessary to follow a daily routine, eat well, avoid stress and nervous overload.
As it became clear, the appearance of atypical formations on the tongue is an alarming sign. It should alert a person and force him to immediately consult a dentist in order to avoid complications and the disease progressing to an advanced form, fraught with the development of oncology. Patients over 50 years of age, suffering from chronic diseases and having a weakened immune system should be especially attentive to their health.
Symptoms of leukoplakia
The clinical picture of leukoplakia depends on the location and shape of the lesion.
When the vagina and cervix are affected, as a rule, there are no complaints and pathology is detected during examination. The lesion on the vulva or penis causes chronic itching and burning when exposed to urine.
Symptoms of oral leukoplakia are determined by the form of the lesion:
- flat flows unnoticed;
- verrucous causes a feeling of tightness, spicy and sour foods cause a burning sensation;
- erosive pain and interferes with eating, reacting to any food with a sharp increase in pain;
- soft usually develops on the cheek near the teeth, the thickening can be bitten, and the resulting wounds are painful.
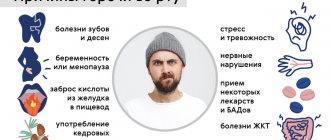
Leukoplakia of the oral cavity: causes of the disease
The reasons causing the development of the disease include:
- Smoking. When using tobacco, the oral cavity is exposed to various irritants, including thermal (incoming smoke has a temperature of about 60 degrees Celsius) and chemical (nicotine, tar and combustion products). No less dangerous is chewing tobacco, which is also a provoking factor.
- Eating either very hot or very cold food on a regular basis for a long time.
- Mechanical trauma (bad bite, sharp edges of teeth, orthopedic structures installed with violations).
- Metal seals that cause galvanic currents.
- Inhalation of vapors of gasoline, benzene, varnishes and paints, as well as other resins.
- Hormonal imbalance, constant stress and lack of retinol.
Diagnosis of leukoplakia
Leukoplakia is a benign process, but severe dysplasia (CIN) can be hidden under its mask, and this is cancer in situ or stage 0. In the simple form, malignant degeneration is diagnosed in every 20th first-time patient; with erythroplakia, only in every tenth there are no signs of malignant transformation.
The final diagnosis of the disease is made only after a morphological examination of the pathological area. At the first stage, during an examination for cytology, cells are scraped off the surface of the spot, then a biopsy is taken for histological examination of the formation.
To track treatment results, it is necessary to know the initial boundaries of the pathological focus and their changes. The boundaries are determined using infrared light scanning - optical coherence tomography or the luminescence method, when the pathology area is irradiated with ultraviolet light. The color of normal and altered mucous membranes is not the same. In gynecology, colposcopy plays an important role, supplemented by multiple magnification of the area with treatment with special solutions.
Features of treatment
It is necessary to undergo treatment. With FSM, the answer to the question “can leukoplakia go away on its own?” definitely negative. With leukoplakia, changes in the mucous membrane are irreversible. The condition can only get worse. It’s better not to take risks, otherwise, waiting for it to “go away on its own,” you can wait until a malignant tumor appears. And then long-term and serious treatment will be required, with a lot of side effects.
If leukoplakia goes away on its own, this means one thing – the diagnosis was wrong. Even a simple LSM needs to be treated.
If LSM is combined with an inflammatory process, it is treated immediately. Antibacterial, antiviral, anti-inflammatory drugs are prescribed (depending on the disease). For endocrine disorders, medications that affect hormonal levels.
Leukoplakia often develops against the background of hypo- and vitamin deficiency. Therefore, treatment is supplemented with preparations containing vitamins E, A, C.
Leukoplakia of the cervix is removed. Various methods are used for this:
- medicinal cauterization (for simple LSM);
- cryodestruction;
- laser removal;
- loop electroexcision;
- knife conization.
According to WHO protocols, drug treatment is recommended for local, local lesions, a single focus of simple leukoplakia. Modern chemical coagulants penetrate to a depth of 2.5 mm and destroy pathological areas. When using them, there is a high probability of relapse.
Removal of leukoplakia is carried out in the first phase of the menstrual cycle, immediately after the cessation of menstruation. Since this significantly reduces the risk of bleeding. Allows the cervix to recover before the next cycle begins.
Cryodestruction
The pathological focus of the cervix is destroyed by freezing. A cryoprobe (a metal, very cooled disk) is applied twice. Touch duration is 3 minutes. Then the tissues are thawed for 5 minutes, and the cryoprobe is again in contact with the uterine tissues. When exposed to cold, the affected areas are destroyed.
The procedure is painless (sometimes patients feel a short-term attack of cramping pain).
Peculiarities:
- cryodestruction is effective for small foci of leukoplakia;
- To carry out the procedure, expensive medical, absolutely dry carbon dioxide and nitrous oxide are used;
- can be performed without anesthesia;
- no side effects (bleeding);
- carried out on an outpatient basis, after cryodestruction there is no need to stay in the hospital;
- The duration of the operation is 15 minutes.
Cryodestruction is not recommended if a histological examination of the biopsy specimen is required. For large lesions, the effectiveness of the procedure is no more than 80%. It is not performed when the pathological area is 2 mm larger than the cryoprobe, more than 75% of the cervix is affected, and leukoplakia has spread to the vaginal wall.
After cryotherapy, patients with menstrual irregularities have a high probability of relapse.
High intensity laser treatment
During laser vaporization of LSM, pathological areas are evaporated and burned. In this case, nearby tissues are not damaged.
Peculiarities:
- laser treatment is carried out on an outpatient basis;
- vaporization destroys not only leukoplakia, but also microorganisms, so the procedure is sterile, there is no risk of infection;
- when the process spreads to the vagina, laser treatment is carried out in 2 stages (leukoplakia on the cervix is immediately removed, at the beginning of the next menstrual cycle the pathological process of the vagina is coagulated);
- the procedure lasts 15 minutes;
- no anesthesia required;
- complete healing occurs on days 16–40;
- after the procedure there is no stenosis of the cervical canal;
- no risk of bleeding.
The procedure is more effective than cryotherapy and is used to treat large and small lesions.
Disadvantage: impossibility of conducting histological examination of the material, the probability of relapse is 2–3%.
Loop electroexcision
Leukoplakia is excised using a heated thin wire (tungsten or stainless steel). The operation is performed using electrosurgical equipment. A low voltage is applied to the wire loop, which simultaneously removes leukoplakia lesions and coagulates surrounding tissue.
Peculiarities:
- It is performed on an outpatient basis; there is no need to stay in the hospital after the procedure;
- excision is done under local anesthesia;
- the operation is bloodless;
- the removed tissue is sent for histological examination;
- even large lesions are treated;
- the method is effective in more than 90% of cases.
After electrical excision, scabs appear at the site of the excised tissue. As they heal, they peel off and fall off. During this period, minor bleeding and discharge are possible.
An incorrectly performed operation can lead to:
- implantation endometriosis;
- exacerbation of ovarian inflammation;
- menstrual dysfunction;
- pain in the lower abdomen.
If the procedure is performed by a highly qualified specialist, the risk of side effects is minimal.
This method is used for the treatment of cervical cancer with atypia and further histological examination of the biopsy specimen.
Knife conical excision
This method is used if other methods are not available or with an advanced form of cervical cancer, when there is a high risk of leukoplakia degenerating into non-invasive cancer.
Conical excision is a major surgical procedure.
Peculiarities:
- the operation is performed under general or epidural or spinal anesthesia;
- lasts at least 1 hour;
- the patient is usually discharged from the hospital on the same day or the next;
- the removed fragment is sent for histological examination.
The method is traumatic. There is a risk of bleeding and stenosis of the cervical canal. For recurrent bleeding, antibiotics are recommended.
Important! LSM removal is an organ-saving procedure to preserve reproductive function. With this disease, there is no need to remove the cervix, much less the uterus itself and its appendages. WHO does not recommend these operations, even if the patient insists due to fear of pregnancy.
Treatment of leukoplakia
Treatment begins only after verification, when dysplasia and intraepithelial cancer are completely excluded.
At the first stage, it is necessary to remove the cause of the disease - chronic injury. For leukoplakia of the oral cavity, sanitation is performed - dental treatment. With the help of a narcologist, the patient is asked to quit smoking, he is trained in correct and adequate individual oral hygiene.
With gynecological leukoplakia, the balance of sex hormones is normalized; in case of vaginal prolapse, surgical treatment is recommended.
Correction of concomitant diseases that support leukoplakia is required: anti-inflammatory and antifungal therapy, treatment of chronic infections, diabetes control and weight loss for obesity.
To increase the body's immune resistance, a program of nutritional support and therapeutic nutrition is drawn up, supplemented with microelements and vitamin complexes.
Local therapy is immediately prescribed - various rinses (douches, baths) with astringents and antiseptic solutions, resorption of buccal tablets, in gynecology - vaginal sprays and suppositories. The use of folk remedies is excluded - rosehip and sea buckthorn oils, ointments and gels containing aloe juice that actively stimulate proliferative processes. It has been proven that all malignant tumors originate in uncontrolled proliferation, therefore such “home remedies” for leukoplakia are harmful.
The positive effect of physiotherapeutic procedures is noted if there are no contraindications from other diseases.
The entire program is carried out for several weeks on an outpatient basis with regular follow-up examinations to assess the dynamics of the process.
In case of persistent pathological changes, especially with progression, the hospital stage is resorted to for invasive intervention. The focus of the disease is completely removed by cryodestruction - liquid nitrogen, exposure to a laser beam or radio wave scalpel, and excised during a minor operation.
Very good results are achieved with photodynamic therapy (PDT) - a gentle and at the same time radical method of removing pathology of the mucous membrane in any anatomical area, including damage to hollow organs - the stomach and bladder.
For leukoplakia due to cicatricial deformation of the cervix, reconstructive surgery is performed.
Leukoplakia of the oral cavity: treatment with medications
Treatment involves the complete elimination of irritating factors that led to the development of the disease:
- to give up smoking;
- grinding down sharp edges of teeth;
- sanitation of the oral cavity;
- replacement of fillings;
- use of products to protect the surface of the lips.
Additionally, a course of vitamin A is prescribed, lasting at least a month, which inhibits the process of tissue keratinization.
If the measures taken do not cause complete disappearance of the manifestations of the disease, surgical intervention is allowed: the lesion is excised, depending on the degree of development of the disease, cryodestruction or electrocoagulation is used.
Ulcers deserve special attention, as they can develop into cancerous tumors. For their treatment, drugs are prescribed that enhance the process of tissue regeneration and epithelization. If there is no positive dynamics, surgical intervention cannot be avoided.
A person with leukoplakia must constantly visit the dentist for examination to prevent malignant degeneration of the cells.
In addition to quitting smoking, the patient’s diet is adjusted: during treatment, spicy and too salty foods are excluded from the diet, and it is recommended to eat more vegetables and fruits.
Drugs prescribed:
- products that restore the epithelium (the most effective was 30 percent tocopherol acetate, which is applied to damaged areas three times a day for 15 minutes, after which it is washed off with water);
- antiseptics (after each meal it is recommended to rinse your mouth with a solution of chlorhexidine at a concentration of 0.05%);
- analgesics (their use is justified in the presence of pain. Lidocaine, applied to the mucous membrane before meals, has worked well).
Under no circumstances should you use drugs that have an irritating effect, as otherwise this can lead to the formation of cancer cells.
If there is no improvement within a couple of weeks, surgery is prescribed: this can be either excision with a scalpel or the application of cold in the form of a liquid stream of nitrogen.
Treatment prices
The cost of outpatient treatment of leukoplakia is relatively low, because the methodical and regular implementation of the doctor’s recommendations is of decisive importance.
The main financial costs come from the initial diagnosis of the process, examination to assess the effectiveness of conservative therapy and correction of probable risk factors. In case of leukoplakia of the oral mucosa, dental treatment will be required; in the presence of concomitant diseases that support the pathology, specialist consultations and, possibly, additional studies are necessary.
The cost of the hospital stage consists of payment for a short-term hospital stay, anesthesia during surgery or manipulation, invasive intervention and control examination to assess its effectiveness.
Leukoplakia and pregnancy
Ideally, FSM should be treated before pregnancy. Since this period can provoke excessive growth of pathological areas due to changes in hormonal levels.
What to do if the disease is detected in a pregnant woman? In this case:
- colposcopy is performed, if there are no signs of invasive cancer, then a repeat examination is scheduled 12 weeks after birth;
- A biopsy can cause heavy bleeding, so it is recommended for strict indications.
A pregnant woman diagnosed with cervical leukoplakia should not panic. Nervous experiences will harm her and the child, but will not bring any benefit. Instead, it is better to contact a good specialist to confirm the diagnosis. If FSM has not been ruled out, wait until the baby is born. Then, after healing and cessation of postpartum bleeding, undergo treatment.
Consequences of leukoplakia
LSM does not cause complications if detected early and treated adequately. This is a benign disease. If the therapeutic approach is incorrect, the following consequences of cervical leukoplakia arise:
- reproductive dysfunction (difficult to get pregnant, problems may arise during pregnancy and childbirth);
- cervical cancer.
LSM is dangerous because over time it degenerates into malignant neoplasia. Therefore, it must be treated immediately.
Prognosis for leukoplakia
The danger of leukoplakia is the progression of the process with the likelihood of malignant transformation. Regardless of the form of the disease, the development of a malignant process is observed in a third of all cases. Moreover, malignancy of a simple form, although probable, occurs in a delayed period - after several years and, as a rule, when therapy is ignored. If treatment for verrucous and erosive types of disease is refused, malignant degeneration is noted in every 4-5 cases.
Primary erythroplakia, as a variant of inhomogeneous leukoplakia according to the WHO classification, is already 90% suspicious for cancer in situ at the stage of primary diagnosis. The likelihood of malignancy increases especially significantly in women who smoke - almost 70%. Taken together, all inhomogeneous forms are four times more likely to develop into cancer than homogeneous leukoplakia.
Prognosis and complications
The disease progresses rather slowly, i.e. represents a sluggish pathology, with periods of subsidence and increase in symptoms. But it is important that in the absence of treatment for oral leukoplakia , the disease is constantly growing and irreversible (that is, it does not go away on its own). The gradual transition (degeneration) into inhomogeneous forms is a transition to a precancerous state and even the onset of oral cancer.
The simple, most common form of leukoplakia (homogeneous form) degenerates quite rarely and practically disappears with treatment and elimination of provoking factors (for example, permanent damage to the mucous membrane by orthopedic structures). But other forms of the disease, such as oral verrucous leukoplakia, have a high risk of becoming cancerous. Therefore, even after successful treatment of oral leukoplakia, certain precautions and prevention must be taken, since this disease has a tendency to return.
Disease prevention
Prevention of leukoplakia is based on hygiene and a healthy lifestyle, since smoking and obesity, caries infection and chronic inflammation are among the risk factors for diseases predisposing to mucosal pathology.
Trauma to the oral mucosa is potentially preventable with prompt dental treatment. Maintaining hygiene is not only not a problem, but is greatly facilitated by household gadgets: electric toothbrushes and irrigators. The advisability of using rinses by dentists is questioned, because they wash out not only pathological, but also necessary microflora, destroying the protective barrier of the mucous membrane.
Gynecologists have abandoned electrocoagulation of cervical erosions, which form scars with subsequent leukoplakia. Today in medicine, gentle invasive technologies are used, with maximum results with minimal damage.
Taking care of your own health requires regular preventive examinations. We are ready to help you 24/7, call us.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Bernadsky Yu.I. / Fundamentals of maxillofacial surgery and surgical dentistry//M.: Med. lit., 2007.
- Ksembaev S.S., Nesterov O.V. /Precancers of the oral mucosa, red border of the lips and facial skin// - Kazan: Publishing house. "Fatherland", 2011.
- Prilepskaya V.N., Bebneva T.N., Shilyaev A.Yu. and others/ Leukoplakia of the cervix associated with HPV infection// Ros. Vestn. obstetrician-gynecologist, 2012, vol. 12, no. 4.
- Rabinovich I.M., Rabinovich O.F., Ostrovsky A.D./ New possibilities for diagnosing leukoplakia of the oral mucosa // Dentistry, 2007, special issue.
- Chogovadze N., Jugeli M., Gachechiladze M., Burkadze G./ Cytologic, colposcopic and histopathologic correlations of hyperkeratosis in reproductive women // Georgian Med. News. 2011, V.11, No. 200.
- Williamson BA, DeFrias D., Gunn R., et al./ Significance of extensive hyperkeratosis on cervical/vaginal smears // Acta. Cytol., 2003, V. 47, No. 5.
Leukoplakia is a hyperkeratosis of the oral mucosa (ORM), accompanied by inflammation of the stroma and usually occurring in response to chronic exogenous and endogenous irritations [12, 22, 29].
Leukoplakia refers to one of the types of keratoses, characterized by a chronic course and affecting the oral cavity and the red border of the lips [2] under the influence of endogenous and exogenous factors.
Leukoplakia is usually diagnosed in middle age, and the prevalence of the disease increases over the years. Idiopathic leukoplakia of the oral cavity accounts for 10% of cases, and leukoplakia caused by exo- and endogenous factors accounts for 90% [49]. Men are more often affected [44].
Etiology and pathogenesis.
Despite many works devoted to leukoplakia, the question of its etiology still remains open [20, 23, 33, 43]. It has been established that the appearance of areas of leukoplakia on the oral cavity is provoked by weak but long-acting irritants [36]: hot or spicy food, strong alcoholic drinks, tobacco and betel, meteorological (cold, wind) and occupational factors (aniline paints and varnishes, pitch, coal resins, phenol, some benzene compounds, formaldehyde, products of dry distillation of coal, gasoline vapors, bromine, etc.) [7].
The main exogenous causes of impaired keratinization of the oral mucosa include consumption of alcohol, hot, hot and spicy foods, as well as smoking [4, 45].
Recently, a relationship has been identified between the presence of a viral infection (namely human papillomavirus - HPV), the possible onset of the development of leukoplakia and its subsequent malignancy [2, 18, 35].
Chronic trauma to the oral cavity by sharp edges of decayed teeth and improperly manufactured dentures can lead to limited hyperkeratosis and the formation of leukoplakic plaques. The galvanic current that occurs when dissimilar metals are present in the alloy of the prosthesis can also contribute to the disruption of keratinization of the mucous membrane [5, 16]. When leukoplakia is localized on the red border of the lips, chronic injury from a cigarette, pipe, or mouthpiece is important [16, 46].
Leukoplakia is an occupational disease of people working in chemical production and in hot shops [40].
Endogenous factors also have a huge impact on the occurrence and clinical course of leukoplakia.
A relationship has been established between the occurrence of leukoplakia and stress, hormonal disorders [10], the presence of pathology of the gastrointestinal tract (GIT) [9, 15], lack of vitamins A, E, B12 [24, 27, 38, 47, 48], as well as genetic predisposition [13, 14, 19, 32].
There is a connection between the occurrence and development of leukoplakia and chronic candidiasis infection [31, 54].
Some patients are diagnosed with endocrine diseases, in particular diabetes types 1 and 2. The causes of leukoplakia are indicated by fluctuations in the level of the ratio of sex steroid hormones associated with age-related involution, which disrupts the processes of metabolism and protein synthesis and, in turn, reduces the resistance of tissues to exposure to unfavorable factors, but a direct correlation between these factors and the occurrence of leukoplakia was not observed [10, 15].
The relationship between the presence of leukoplakia and HPV remains controversial, although many patients with leukoplakia have HPV type 16 [2, 39, 42, 51].
Classification of leukoplakia SOP
According to the modern WHO classification, 10th revision (1999), a distinction is made between homogeneous and inhomogeneous leukoplakia. Non-homogeneous leukoplakia, in turn, is divided into erythroplakia, nodular, spotted and verrucous leukoplakia [19, 22, 28, 34, 50]. Evidence has accumulated that inhomogeneous leukoplakia, especially macular leukoplakia, is epithelial dysplasia in 50% of cases and is characterized by a high incidence of malignancy [8].
In 2005, WHO adopted another classification of head and neck diseases, in which the concept of “epithelial precancer” appears [52], which, in turn, includes erythroplakia and leukoplakia SOP. According to this, leukoplakia is histologically divided into focal epithelial hyperplasia (without atypia), low, moderate and high grade dysplasia. For the last 3 types of leukoplakia, the concept of “squamous intraepithelial neoplasia” (Squamous Intraepithelial Neoplasia - SIN) from 1 to 3 degrees of severity was introduced. The main feature of the SIN classification is a clear display of each stage of malignant transformation of the epithelium of the oral cavity [53].
It should be noted that this classification is primarily pathomorphological and complements the clinical diagnosis itself.
Histological structure of unchanged epithelium of the oral cavity
The unchanged, non-keratinized stratified squamous epithelium of the oral cavity includes a basement membrane, a basal layer, represented by 1 row of cells having a cylindrical or cubic shape; Next comes the parabasal cell layer, consisting of 1-2 rows of cells located above the basal ones and having no connection with the basement membrane, then the spinous layer, which contains 5-6 rows of large, irregularly shaped cells with processes, then flattening of the cells and their turning flat. On the hard palate, dorsum of the tongue and gums in the keratinized epithelium, adjacent to the spinous layer is a granular layer, consisting of elongated cells with keratinosomes and keratohyaline granules, as well as a stratum corneum with rows of keratinized cells, in which nuclei and cytoplasmic organelles are not visible. Cytologically, from the basal to the superficial keratin layer of the epithelium, a progressive decrease in the nuclear-cytoplasmic ratio and accumulation of intracellular keratin is noted [3].
Clinical and morphological characteristics of leukoplakia
The clinical picture of leukoplakia depends both on the form of the disease and the factor causing it, as well as on the location. Leukoplakia is a chronic disease; patients often cannot clarify the moment of its onset. Clinically, leukoplakia is manifested by hyperplastic processes in stratified squamous epithelium under the influence of various damaging agents and is expressed in the formation of superficial hyperkeratosis. The parabasal, basal and superficial layers of the epithelium change. Clinically, leukoplakia has several forms; histologically it can be characterized by various nosological processes - from benign hyperkeratosis to invasive squamous cell carcinoma. Therefore, all excised tissue must be sent for pathomorphological examination, which should include histological and immunohistochemical (IHC) examination.
IHC research is a method for identifying the specific antigenic properties of malignant tumors. IHC methods are used to localize a particular cellular or tissue component (antigen) in situ
by binding it to labeled antibodies and are an integral part of modern cancer diagnostics, providing detection in tissues of various cells, markers of proliferation, cell maturity, and acanthosis factors.
Subsequently, specific antibodies and reagents are used to visualize antigens.
Leukoplakia is a strictly clinical term; it is not currently used for morphological description. With leukoplakia, 4 types of changes can be detected: focal epithelial hyperplasia; squamous intraepithelial neoplasia grade 1 (SINI), squamous intraepithelial neoplasia grade 2 (SINII), and squamous intraepithelial neoplasia grade 3 (SINIII) [17].
With focal epithelial hyperplasia, an increase in the thickness of the epithelium is noted due to an increase in one of the components of the basal, spinous (acanthosis) or superficial (hyper- and parakeratosis) layers. It may be accompanied by inflammatory and reactive cytological changes.
In grade I squamous intraepithelial neoplasia, the epithelium contains cells with slightly altered cytological characteristics; changes are limited to the lower third of the epithelium; at the same time, normal maturation of epithelial cells in the upper 2/3 of the epithelium is maintained. Mitoses of a normal configuration limited to the basal layer may be detected, and hyperkeratosis is also possible.
With squamous intraepithelial neoplasia of grade II, altered cells with atypical cytological characteristics are observed already in the lower and middle third of the epithelium. Large nucleoli are detected in the nuclei; thus, cellular atypia is more pronounced. Differentiation of cells and tissues is preserved in the upper third of the mucous membrane, mitoses are observed in the intermediate and parabasal layers.
In grade 3 squamous intraepithelial neoplasia (SIN III), mitotic activity is detected in actively proliferating cells; they occupy more than 2/3 of the epithelial layer. However, they do not have the cytological atypia characteristic of carcinoma in situ
. Cell differentiation is preserved in the superficial layers. Hyperkeratosis may be present. As neoplastic changes in the epithelium increase, inflammatory phenomena intensify in the underlying dermis, accompanied by infiltration of lymphocytes.
Clinically, the process usually begins with the so-called preleukoplakic stage, which is characterized by inflammation of the oral cavity. This stage is rarely observed on the red border of the lips [12].
After this, keratinization occurs, and the so-called flat, or simple, form of leukoplakia develops, which is a uniform keratinization of a limited area of the mucous membrane, which is the result of epithelial hyperplasia and is accompanied by chronic inflammation of the stroma. Most often, this form of leukoplakia is localized on the mucous membrane of the cheeks, along the line of closure of the teeth and in the corners of the mouth, on the tongue. The affected areas of the mucosa may have different shapes; Thus, keratinization of a limited area of the mucous membrane of the cheek is possible in the form of stripes with clear boundaries and irregular outlines, which cannot be removed by scraping.
There are almost no subjective sensations with flat leukoplakia. Patients may notice a cosmetic defect in the form of a whitish area of the mucous membrane or roughness. The disease is characterized by varying degrees of thickening of the epithelial layer and involvement of the lamina propria of the oral cavity in the chronic inflammatory process; Clinically, the inflammatory reaction has the appearance of chronic inflammation or does not manifest itself at all. An important feature of this form of leukoplakia is that the areas of the oral cavity that have undergone keratinization do not rise above the surrounding tissues.
Pathomorphologically, this form of leukoplakia is described as focal epithelial hyperplasia, in which manifestations of hyperkeratosis alternate with parakeratosis. If keratinization is of the nature of parakeratosis, the phenomena of acanthosis are most pronounced. The lamina propria of the oral cavity in the affected area has an inflammatory infiltrate of mononuclear cells and plasma cells, which alternates with foci of fibrosis and sclerosis. The connective tissue is plethoric, edematous, loosened. The parabasal layer of the epithelium is prominent. The thickness of the spinous layer is 40-50 rows of cells, acanthosis is noted.
Thus, parakeratosis in flat leukoplakia is more often combined with epithelial hyperplasia, in which the basement membrane remains well defined as a line separating the thickened epithelium from the underlying stroma.
The flat form of leukoplakia can proceed for years without changes or can develop into a verrucous form.
Verrucous leukoplakia is a special form of leukoplakia. Its main clinical sign is an area of pronounced keratinization that rises significantly above the level of the SOR and sharply differs in color from it. Foci of hyperkeratosis have a bright milky white color.
There are plaque and warty forms of verrucous leukoplakia [30]. In the plaque form, limited milky-white, sometimes straw-yellow, rounded formations with clear contours are identified, rising above the surrounding mucous membrane. Verrucous leukoplakia with warty growths has the most pronounced tendency to malignant transformation [1, 8, 21, 26].
The warty variety of verrucous leukoplakia is characterized by dense grayish-white bumpy formations, rising 2-3 mm above the level of the mucous membrane; it has a greater potential for malignancy than plaque. A number of foreign and domestic authors note that it is verrucous leukoplakia that in 70% of cases transforms into squamous cell carcinoma [6, 8, 11, 25, 37].
Histologically, the epithelial cover of the mucous membrane is sharply thickened due to the proliferation of the horny and granular layers. In the cytoplasm of the cells of the granular layer, the amount of keratohyalin increases. The most superficial cells have the appearance of thin scales with dense homogeneous eosinophilic protoplasm and degenerating nuclei. Thin connective tissue papillae protrude deeply into the thickness of the integumentary epithelium. Acanthosis is pronounced; in the underlying, edematous and loosened connective tissue, chronic inflammation, hyperemia, and cellular infiltration are determined. With verrucous leukoplakia, pronounced hyperkeratosis is found, rarely combined with small foci of parakeratosis; sometimes the stratum pellucida is involved in the pathological process; the granular layer consists of 4-5 rows of cells with well-defined granulomas, the spinous layer - of 8-12 rows of cells. It is possible to identify atypical cells. In some cases, acanthosis is accompanied by elongation and expansion of epithelial processes. Changes in the cells of the spinous layer are observed. The cells are of different sizes and shapes, have large hyperchromatic nuclei containing on average 2-4 large nucleoli.
The erosive form of leukoplakia is the most malignant [41]. With the erosive form of leukoplakia, cracks and erosions appear, which are inevitably subject to mechanical and thermal stress.
Erosion occurs as a result of injury to foci of simple and verrucous leukoplakia by mechanical and thermal factors. As a rule, this is observed on the mucous membrane of the tongue, cheeks, and red border of the lips. With increased keratinization and the appearance of infiltration at the base of bleeding and non-healing erosion, we can talk about the malignancy of the process.
Histological examination shows that the mucous membrane is thickened, the spinous layer and intercellular spaces are expanded. Strands of epithelium protrude deeply into the thickness of the connective tissue layer, delimiting elongated, thin papillae - acanthosis. The epithelium is loosened in places; Erosion forms in places where epithelium is lost. Chronic inflammation is observed in the lamina propria of the mucous membrane, intercellular infiltration with an admixture of plasma cells and mononuclear cells is pronounced.
If squamous cell carcinoma is suspected, the histological picture is characterized by the appearance of oval-shaped areas of hyperkeratosis with so-called “cancer pearls”. Complexes of atypical squamous epithelial cells with invasive growth into the lamina propria of the mucous membrane are identified. Atypical cells have cytological signs of malignancy, including a high nuclear-cytoplasmic ratio, prominent 1 or more nucleoli, nuclear hyperchromasia and pleomorphism, and pathological mitoses.
Thus, the pathologist's report will not contain a clinical diagnosis, but diagnoses (SIN), such as focal epithelial hyperplasia, squamous epithelial neoplasia of varying degrees (from 1st to 3rd), the presence or absence of atypical cells, hyperkeratosis, verrucous leukoplakia or squamous cell carcinoma [17].
Based on the above, leukoplakia is a clinical term. The pathomorphological report contains a description in accordance with the 2005 WHO classification: the degree of damage to the mucous membrane is described depending on the depth. The presence of hyperkeratosis and hyperplasia should be considered as confirmation of the clinical diagnosis of leukoplakia. The leading clinical sign of verrucous leukoplakia is foci of hyperkeratosis that rise strongly above the surrounding mucosa, and with ulcerative-erosive leukoplakia - foci of erosion.
If frequent mitoses and a cluster of atypical cells with several large nuclei are described, we can talk about carcinoma in situ
. Leukoplakia is considered a precancerous disease. Its verrucous and erosive-ulcerative forms are most prone to malignancy, therefore, during surgical treatment, pathomorphological examination, including IHC, is mandatory.