© Author: Z. Nelly Vladimirovna, laboratory diagnostics doctor at the Research Institute of Transfusiology and Medical Biotechnology, especially for SosudInfo.ru (about the authors)
Fibrin is a solid, insoluble protein, consisting of fibrous, rather long, threads. Fibrin is a protein that is unstable in plasma, so it simply does not circulate in the blood. Fibrin owes its formation to an extraordinary situation that activates the hemostatic system, such as damage to the vascular wall as a result of injury or, for example, an inflammatory reaction at the site of formation of an atherosclerotic plaque. And in the bloodstream there is its precursor - soluble fibrinogen (first blood coagulation factor - FI), which, like many other proteins, is synthesized in the liver parenchyma and in response to damage to the blood vessel under the enzymatic influence of thrombin on the wound is converted into fibrin.
When fibrin is no longer needed, the fibrinolytic system dissolves the clot (fibrinolysis). Experts believe that in the blood there is a constant process of converting some very small amount of fibrinogen into fibrin, but this problem is also constantly solved by fibrinolysis.
There is no standard for fibrin itself in clinical laboratory diagnostics. Since this substance is not normally detected in the blood , an analysis examining this indicator is not performed. The quantity and quality of fibrin is judged by the level of fibrinogen in the blood, also examining other factors of the coagulation system as part of the coagulogram.
The process of fibrin formation
Processes of formation of fibrin and fibrinogen
Fibrin formation is a complex chemical process. It consists of several stages:
- Cleavage of two peptides A and two peptides B from the fibrogen molecule under the influence of thrombin with the subsequent formation of fibrin monomer. The resulting monomer consists of two identical particles connected by disulfide bridges. Each particle consists of 3 different polypeptide chains.
- Spontaneous transformation of fibrin monomer into a clot, which is called fibrin aggregate or unstabilized fibrin. This process is accelerated by substances that carry a positive charge and inhibited by substances with negatively charged particles. During aggregation of the monomer, molecules from globules are transformed into fibrils - thread-like proteins. Different types of chemical bonds and hydrophobic forces are involved in the creation of unstabilized fibrin. They can be weakened in environments that cause denaturation. Due to denaturation, the fibrin aggregate can be reduced to a monomer.
- Unstabilized fibrogen is affected by a fibrin-stabilizing factor, due to which the structure of the aggregate changes. Due to the appearance of covalent bonds in polypeptide chains, the fibrin aggregate is stabilized into a fibrin polymer. If a person suffers from congenital or chronic diseases accompanied by a deficiency of fibrin-stabilizing factor, the aggregate form will not be able to stabilize into a polymer. Then a clot does not form from fibrin.
Many fibrin polymer molecules cooperate to form threads. They capture platelets and other blood cells and form them into a spongy substance. It gets confused, becomes denser and forms a blood clot.
What is fibrin?
Fibrin threads
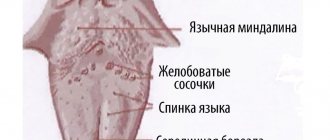
Fibrin is a high molecular weight protein that is a derivative of fibrogen synthesized by the liver. It has the form of long cross-striped or smooth fibers. Clots of these fibers form the basis of a blood clot, which is formed during blood clotting.
Unlike fibrogen, which is the first coagulation factor, fibrin is not constantly present in the plasma. It appears due to extraordinary situations that activate the homeostasis system - the body’s ability to maintain consistency regardless of environmental factors. Such extraordinary situations are wounds and inflammations that arise due to a violation of the integrity of tissues and blood vessels.
↑ Exodus
Thrombocrit is higher than normal: symptoms and treatment
The outcome of fibrinous inflammation of the mucous and serous membranes is not the same. After the films are rejected, defects of varying depths remain on the mucous membranes - ulcers; with lobar inflammation they are superficial, with diphtheritic inflammation they are deep and leave behind scar changes. On serous membranes, resorption of fibrinous exudate is possible. However, fibrin masses often undergo organization, which leads to the formation of adhesions between the serous layers of the pleura, peritoneum, and cardiac membrane. As a result of fibrinous inflammation, the serous cavity can become completely overgrown with connective tissue—its obliteration.
The significance of fibrinous inflammation is very great, since it forms the morphological basis of many diseases (diphtheria, dysentery), and is observed during intoxication (uremia). When films form in the larynx and trachea, there is a risk of asphyxia; When films in the intestines are rejected, bleeding from the resulting ulcers is possible. After fibrinous inflammation, long-term non-healing, scarring ulcers may remain.
Authors: A. I. Strukov, V. V. Serov
The role of fibrin in inflammation
Fibrin networks limit the focus of inflammation
Fibrin synthesis begins immediately after fibrogen comes into contact with the enzyme thrombokinase, which is released from damaged or destroyed tissues. After this, a fixation reaction occurs, during which fibrin captures pathological substances and blocks them. Thus, fibrin prevents inflammation from spreading to healthy tissue.
Fibrin also prevents the inflammation itself from growing. At its very initial stages, when active division of leukocytes and their migration to the site of inflammation has not yet begun, fibrin molecules surround the site in a circle and prevent its spread.
What complications are possible after tooth extraction?
What does it mean that fibrinogen levels in the blood are higher than normal?
It happens that a fairly quick process of tooth extraction does not go as desired. Complex cases are when the duration of the removal itself lasts longer than usual, and the doctor has to perform more manipulations. The procedure itself is complex, which means that the recovery process may be burdened with some difficulties
Usually the doctor warns you how long the painful sensations will last, how to relieve them, and what to pay attention to.
Table. Possible complications after tooth extraction
| Name of pathology | Description | Notes |
| Gum tissues become swollen and the oral mucosa becomes inflamed. | You will need to take antibiotics |
| Swelling, purulent accumulations, throbbing pain | Occurs due to infection of the wound |
| Inflammatory process in the hole itself, infection in the oral cavity | Requires medication |
| Explained by incorrect actions of the doctor | Requires surgical correction and medication |
| Advanced stage of alveolitis | Complex treatment |
First, a diagnosis is made, then the doctor will tell you what therapy will be needed. But problems can begin, for example, at night. If you see not white, but gray plaque at the site of the wound, call an ambulance. This is alveolitis, wound infection, a dangerous complication that requires prompt intervention.
Symptoms of alveolitis
The doctor removes the pus with special instruments, possibly a solution. You will also need to take medications, and antibacterial therapy is also possible. It is impossible to bring the condition to the most advanced stage: complications are difficult to treat.
Treatment of alveolitis
What is RFMK, why is it important during pregnancy
RFMK in a blood test: what is it? norms of analysis indicators, reasons for increase
During bleeding, the main thing is to stop the “leakage” of liquid tissue; This is facilitated by the blood itself, which is capable of coagulating, forming clots that clog the wound. Such clots (thrombi) contain a solid protein substance, fibrin, which is produced when the body signals damage to blood vessels. The wound has healed, the fibrin has completed its task - and then the clot needs to be dissolved. The body begins a process called fibrinolysis, through which blood clots dissolve.
Blood clots, as is known, form inside blood vessels under the influence of negative factors, preventing normal blood flow. Here, too, fibrin cannot be avoided.
Fibrin is a protein substance with a fibrous structure that helps form blood clots
During fibrinolysis, the protein, as a rule, does not completely degrade; fibrin particles continue to circulate in the blood. The abbreviation RFMC stands for soluble fibrin-monomer complex; the indicator characterizes the level of fibrin breakdown - when too many protein particles remain in the blood, the threat of blood clots and blockage of blood vessels increases. The pathology was called thrombinemia, to confirm the diagnosis, the patient was sent to take a blood test RFMC.
In people who are not prone to thrombosis, there are practically no fibrin grains in the blood.
The normal RFMC value for an adult is 3.38–4 mg per 100 ml.
What happens to the expectant mother's blood?
During pregnancy, not only hormonal changes occur in a woman’s body; to the systemic and pulmonary circulation a third is added - the uteroplacental one. This circle appears after full maturation at 16–18 weeks of the temporary organ - the placenta, which is responsible for the nutrition and respiration of the fetus. From now on, the baby receives nutrients and oxygen from the bloodstream through the umbilical cord connected to the placenta, and “production waste” is removed through the umbilical veins.
The third circle sets the body a new mode of operation, which is not easy to adapt to; Now the load on the circulatory system has increased sharply. Blood flow indicators change, for example:
- the volume of blood circulating through the veins and arteries increases;
- blood density (clotting) increases; the liquid tissue seems to be preparing for childbirth, when large blood losses are inevitable and it is necessary to stop the bleeding more quickly;
- in the plasma the level of blood cells, as well as the proteins prothrombin and fibrinogen (a precursor of fibrin), jumps.
It turns out that a pregnant woman’s blood thickens for objective reasons, so doctors do not consider a moderate increase in the amount of fibrinogen to be a pathology. For expectant mothers, a RFMC norm different from the standard was established - up to 7.5 mg per 100 ml.
The appearance of a pregnant placenta changes the ratio of blood cells and increases the density of liquid tissue
How the RFMK changes at different times
The signal for an increase in fibrinogen in the blood is the formation of the placenta; Until this moment, the RFMC of the expectant mother differs little from the standard one. Here are the norms for each trimester:
- first (1–14 weeks) - up to 5.1 mg/100 ml; the body has not yet detected changes in the composition of the blood, since there is no placenta and the intensity of blood circulation is the same;
- second (15–28 weeks) - up to 6.5 mg/100 ml; the placenta has formed, the need for additional blood has increased for the normal supply of the temporary organ;
- third (29–40 weeks) - up to 7.5 mg/100 ml; closer to childbirth, the placenta “grows old”, the baby’s place does not remain in the womb for long; the body begins to realize that major blood loss is on the way, it’s time to defend itself; The thickness of the blood increases, and the concentration of fibrin particles also increases.
However, everything is good in moderation. If the RFMC produces too high numbers, it means that dangerous changes are occurring in the pregnant woman’s body that can have a detrimental effect on the health of the mother and fetus, and in some situations, threaten the lives of both
Therefore, it is important to control such an indicator as RFMK
In the 3rd trimester, increased vigilance is required, since as the size of the fetus and, accordingly, the uterus increases, the reproductive organ begins to put pressure on the inferior vena cava, the largest vessel in the body. As a result, the speed of blood flow in the veins of the legs decreases, creating favorable conditions for the formation of blood clots.
Fibrin threads in a smear in women
Good afternoon Help decipher the results of the analysis. Laparoscopy is coming. Will they accept me for surgery with such tests? What is fibrin in a smear?
Microscopic picture: V - Flat epithelium of the surface layer 5-10 in n/z. Leukocytes - single in the field of view. Mucus + Fibrin + Microflora - rod-shaped, morphotype similar to lactobacilli + C - Flat epithelium of the surface layer 2-5 in p/z. Leukocytes - single in the field of view. Mucus + Microflora - the same as in “V” Neisseria gonorrhoeae were not found in the preparation.
Trichomonas vaginalis was not found in the preparation.
3 answers
Hello! Please help me decipher the smear. The presence of fibrin is of concern. Microscopic picture:
V- Flat epithelium of the superficial, intermediate layer in moderate quantities Leukocytes - 2-7 in the small space Mucus +
Microflora – cocci in moderate quantities, rods - single.
C- Flat epithelium - single cells Leukocytes - 2-6 per cell Mucus +++ Fibrin
Microflora – cocci in small quantities.
What should I do if I have a similar but different question?
If you did not find the information you need among the answers to this question, or your problem is slightly different from the one presented, try asking an additional question to the doctor on the same page, if it is on the topic of the main question.
You can also ask a new question, and after a while our doctors will answer it. It's free. You can also search for the information you need in similar questions on this page or through the site search page.
We will be very grateful if you recommend us to your friends on social networks.
Medical portal 03online.com
provides medical consultations via correspondence with doctors on the website. Here you get answers from real practitioners in your field.
Currently, on the site you can get advice in 48 areas: allergist, anesthesiologist-resuscitator, venereologist, gastroenterologist, hematologist, geneticist, gynecologist, homeopath, dermatologist, pediatric gynecologist, pediatric neurologist, pediatric urologist, pediatric surgeon, pediatric endocrinologist, nutritionist, immunologist a , infectious disease specialist, cardiologist, cosmetologist, speech therapist, ENT specialist, mammologist, medical lawyer, narcologist, neurologist, neurosurgeon, nephrologist, oncologist, oncourologist, orthopedist-traumatologist, ophthalmologist, pediatrician, plastic surgeon, proctologist, psychiatrist, psychologist, pulmonologist, rheumatologist, radiologist , sexologist-andrologist, dentist, urologist, pharmacist, herbalist, phlebologist, surgeon, endocrinologist.
We answer 97.11% of questions.
What is nephrolithiasis - symptoms and treatment
The diagnosis of nephrolithiasis is made when hard crystalline deposits, or “kidney stones,” as they are called, are found in the kidneys. They usually form in the calyx, pelvis or parenchyma of the kidney. Men are more susceptible to nephrolithiasis; women and children are less likely to suffer. The risk factor includes people aged 25 to 50 years.
Have you been trying to cure your KIDNEYS for many years?
Head of the Institute of Nephrology: “You will be amazed at how easy it is to heal your kidneys just by taking it every day.
Our readers successfully use Renon Duo to treat kidneys. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
What is nephrolithiasis (disease (nephrolithiasis, from Greek)? How to treat the disease?
Reasons for development
Normally, the salts found in the kidneys dissolve and are excreted from the body along with urine. However, due to a number of circumstances, this process may be disrupted. If the urine becomes highly concentrated, the salts dissolve less well and begin to condense with particles of dead epithelium, microorganisms, and blood leukocytes. Gradually crystallizing, they form stones.
The following factors contribute to the risk of developing nephrolithiasis (disease (nephrolithiasis, from Greek) (disease (nephrolithiasis, from Greek):
- First of all, this is the nature of nutrition. The predominance of animal proteins, fats, and foods high in acids in food can contribute to the appearance of pathology.
- A small amount of urine excreted per day is also a risk factor. This can occur with insufficient fluid intake, excessive sweating, or obstruction of the ureters.
- The situation is aggravated by possible urinary tract infections and their untimely treatment (a process the purpose of which is to alleviate, relieve or eliminate the symptoms and manifestations of a disease or injury, pathological condition or other disability).
- In addition, the reason for the formation of stones can be rapid weight loss, for example, with excessive dieting.
Other known causes of nephrolithiasis (disease (nephrolithiasis, from Greek) are the composition of drinking water, a sedentary lifestyle, as well as a hereditary predisposition.
Classification of the disease
Kidney stones with nephrolithiasis differ in shape, size, composition and location. Knowing exactly what type they are is important for proper diagnosis and treatment. According to the chemical composition, stones are of the following types:
• Oxalate - formed by combining oxalic acid and calcium. It occurs most often (in approximately 80% of cases). The cause of development is excessive consumption of vitamin C, contained in vegetables and fruits, with impaired metabolism.
Excessive consumption of coffee and chocolate may be a risk factor. Oxalates differ from other types of formations in their increased hardness and sharpness, due to this they more often provoke bleeding. • Urates are the second most common among all cases of nephrolithiasis.
The reason here is an excess of uric acid salts.
• Phosphate - develop with excessive formation of phosphoric acid salts, as a rule, in people whose diet is dominated by a dairy-vegetable diet. They have a smooth structure and cause less damage to internal organs, but they grow very quickly. Phosphates occur in approximately 5% of all cases.
Source: https://vsedlyavasdamy.ru/info/niti-fibrina-v-mazke-u-zhenshhin/
The normal level of fibrinogen in the blood of women, men and children
Only a specialist can interpret the data obtained from a blood test for fibrinogen in combination with other laboratory parameters and the patient’s medical history.
The norm of fibrinogen in a biochemical analysis of blood serum ranges from 1.8 to 4 g/l. It should be noted that the minimum level of fibrinogen in the blood is 0.5 g/l - only in this case is it possible to maintain homeostasis in the human body.
Normal (reference) values are the same for both sexes and all ages. The exception is pregnant women.
Fibrinogen levels during pregnancy by trimester
Normally, fibrinogen increases significantly during pregnancy. This is due to the need to prepare a woman’s body for childbirth, during which blood loss is inevitable. During a physiological birth, the expectant mother loses about 300 ml of blood, and during a caesarean section this figure reaches 750 ml. In order to prevent excessive bleeding, the blood coagulation system is activated.
When interpreting the obtained data, it is necessary to take into account the gestational age, since the reference values for them are different. The table shows the maximum permissible indicators of the criterion under consideration.
| Gestation period, weeks | Normal values, g/l |
| 1 – 14 | 2,2 – 4,35 |
| 14 –20 | 2,85 – 5,28 |
| 210 – 30 | 3,1 – 5,68 |
| 30 – 35 | 3,1 – 5,73 |
| 35 – 42 | 3,3 – 6,2 |
The maximum increase in fibrinogen is typical for the third trimester during pregnancy, since the woman’s body activates all systems and organs in preparation for labor.
How to identify the disease
If the patient notices changes in his body that are similar to the first signs of the disease, he should immediately consult a doctor. The following activities will help to make a correct diagnosis:
- General blood and urine tests will determine the stage of the inflammatory process.
- Radiography allows you to track changes in the esophagus and detect a hernia or ulcer.
- Daily pH-metry. The procedure lasts 24 hours. Helps determine the level of gastric oxidation.
- Endoscopy. Determines the degree of the disease, the presence of erosions and edema.
- Biopsy. This is a test that requires taking a tissue sample.
- Diagnosis may consist of an initial examination of the oral cavity and palpation of the abdomen.
Possible complications due to untimely treatment:
- Heavy bleeding.
- Stomach ulcer.
- Scarring.
Body protection
The formation of insoluble fibrin helps protect the body from blood loss, as well as from inflammatory processes. However, such a reaction causes pain and swelling, tissue damage, and disruption of their functionality. This is subsequently eliminated by reparative processes. At their early stage, special substances are produced that cause fibrin depolymerization. Such a reaction, even at the very beginning of the inflammatory process, can inhibit the effect of protein on the pathological focus.
Treatment with folk remedies
It is possible to use folk remedies. It cannot be said that such treatment is effective, but it is excellent as a preventive measure. A course of therapy correctly drawn up by the attending physician can be used in parallel with folk remedies. But only after consulting a doctor.
Examples of home therapy:
- Flax seeds. Their mucus envelops the esophagus, thereby preventing the formation of a fibrinous film and erosion, and reduces acidity. To prepare a healing decoction, just boil one teaspoon of seeds in half a glass of water. You need to take the decoction for up to a week.
- Chamomile. Prepare a special herbal mixture of chamomile, lemon balm, and licorice root. You need to take this decoction about 4 times a week. Chamomile will help relieve inflammation and swelling.
- Dill. Pour boiling water over the ground dill and leave for about two hours. Drink the infusion before meals.
Excess and lack of fibrin - is it dangerous?
Fibrin deficiency complicates wound healing
In fact, there is no concept of a norm regarding the amount of fibrin. First of all, doctors look at the results of a coagulogram and the level of fibrogen.
The normal amount of fibrin in areas of inflammation depends significantly on the ratio of coagulation and anticoagulation factors. Fibrin should facilitate the recovery period, but not disrupt the healing process.
If there is little fibrin in the affected tissue area, this will lead to undesirable consequences:
- expansion of the focus of inflammation due to blood coagulation disorders and the lack of a high-quality fibrin framework;
- slow healing of wounds, often accompanied by secondary intention (this is the name for independent wound healing with the subsequent formation of a large scar);
- the risk of bleeding increases.
Fibrin clots without fibrinolysis hinder regeneration processes
There are cases when, during inflammation, the amount of fibrin, on the contrary, significantly exceeds the norm, and fibrinolysis has not yet begun. This is fraught with the development of such pathological processes:
- exacerbation of the nature of inflammation with the appearance of severe pain, severe swelling and even complete cessation of blood circulation at the site of inflammation;
- severe delay in regeneration;
- compression of blood vessels due to blockage by blood clots and blood clots;
- violation of phagocytosis (cellular nutrition) and massive cell death.
In a healthy person, the level of fibrin (rather fibrogen) should also not fluctuate greatly. With increased concentrations of this protein, a person becomes more prone to developing blood clots. These blood clots can break off and wander uncontrollably through the vessels. It happens that a blood clot gets into some important vessel and clogs it; due to the cessation of blood circulation, a person can die. With a reduced concentration of fibrin, there is a predisposition to bleeding. With such a violation, you can lose a lot of blood even due to a banal cut.
How and where can you see “ready” fibrin?
Fibrin can be seen on a wound that was initially purulent, drained and began to heal by secondary intention. After some time, during the healing process, a white coating forms along the edges of the wound - this is fibrin, which protects the site of the lesion and forms future tissue. However, on a wound in which the bleeding has just stopped, fibrin, although present, is unlikely to be detected with the naked eye.
Fibrin can be seen in an ulcer formed on the skin or mucous membranes (for example, in a duodenal ulcer during endoscopic examination), and the presence of this substance at the bottom of the ulcer indicates that it has already begun to prepare for healing (stage 2 - remission stage inflammatory process).
The presence of fibrin in a smear from the urogenital tract (both men and women), viewed under a microscope, may indicate that an inflammatory process is taking place in this area. However, this is an indirect sign. And in order to establish (or suspect?) a diagnosis, a complete description of the biocenosis present in the smear is necessary, that is, fibrin in such cases does not seem to be an independent object of study and means little for diagnosis.
Fibrin threads can also be observed in blood taken without a preservative solution. As the blood coagulates, it forms a clot, releasing serum. In plasma (blood taken with a preservative), fibrinogen is preserved, which is how it differs from serum, so plasma does not lose the ability to form fibrin filaments, which is achieved by adding calcium chloride to this biological medium. These methods are used to prepare hemagglutinating sera that determine human blood groups.
Experiments performed
Scientists conducted experiments on animals, during which it turned out that proteases introduced from outside before the inflammatory process can prevent its development completely, and in some cases the pathology was mild. Experience has shown that the use of tryptic substances in most cases stops the development of inflammatory processes at the onset of the disease.
When prophylactic doses of enzymes were administered, protein formation decreased.
Fibrin is not just a protein, but the creator of a protective barrier around the pathological focus, which protects against disease. Subsequently, this insoluble component serves to build connective tissue. It also participates in regeneration processes. The formation of scar tissue depends on the duration of storage and the amount of fibrin produced by the body.
So what is fibrin and what is it for? This substance is produced by the body's cells in such an amount that is necessary to quickly stop bleeding and which will help quickly restore damaged tissue. In some cases, fibrin is a pest. If it is produced and deposited in large quantities, the protein can cause harm to the body. As far as is known, fibrinolysis is a long process that is not able to dissolve all excess protein. Moreover, this process requires certain conditions.
To get rid of excess fibrin, special enzyme treatment is prescribed.
Fibrin and inflammation
The main function of fibrin is the formation of a coagulation and stopping bleeding, of course, there is no doubt about its significance, however, the role of this substance in the course and completion of the inflammatory process is also important, but is not so widely known to people in non-medical professions, so I would like to dwell a little on the topic: “ Fibrin and inflammation."
Fibrin formation occurs immediately after fibrinogen comes into contact with tissue thrombokinase, released from damaged (wound) or destroyed (ulcer) tissue. This local reaction, in which toxins are captured by fibrin and enclosed in a bundle, is adaptive and is called the “fixation reaction.” It is very important for the body, because at the very early stages, even before white blood cells - leukocytes, “feel” that the scene of an accident awaits them, fibrin will create a barrier around the source, which will counteract the spread of infection throughout the body. That is, it should be recognized that immediately deposited fibrin can rightfully claim a very important and necessary protective role. And the negative changes, which, one way or another, will be present in a small area, will try to take on the problem, protecting other, more important organs (internal) from evil.
What are these changes and how can they be recognized? Quite easy, because each of us has repeatedly observed in ourselves how a recent, even small scratch turns red, swells, and causes discomfort. This insoluble fibrin, formed in the first minutes of the accident, creates significant difficulties for local blood circulation, and sometimes even stops it altogether. Naturally, the site of injury swells and hurts. In order for the reader to understand the entire biochemical process occurring on a wound or ulcer, we will try to describe it sequentially:
- At the moment of transition of fibrinogen into fibrin (1st stage of fibrin formation), enzymes present in the inflammatory focus, which are capable of subjecting proteins having disulfide bridges to tryptic hydrolysis (fibrin monomer, as is known, has them), already begin their activity, acting as inhibitors inflammatory process;
- At stage 2 (formation of fibrin polymer), tryptic enzymes try in every possible way to inhibit fibrin polymerization. These proteases, breaking down fibrin and other protein macromolecules into smaller organic compounds (amino acids, peptides), transform the viscous thick exudate formed on the wound into a more liquid state, in addition, they inhibit the formation of new large molecules that are difficult to dissolve;
- Proteolytic enzymes - proteases (for example, plasmin) at the repair stage trigger the mechanism of destruction of fibrin clots and, thus, restore tissue.
By the way, thanks to numerous and comprehensive studies, it was found that the introduction of proteolytic enzymes before the inflammatory reaction on the wound takes effect makes it possible to prevent its development, which means that, in fact, a person receiving proteases from the outside after various traumatic situations is prevention of inflammation.
Upon completion of the inflammatory process, scars often form in its place - it is the fibrin formed in this area and preserved for a long time that provides the basis for the proliferation of connective tissue cells.
Examination and diagnosis
The prescription of treatment procedures and other measures depends on a complete and correct diagnosis. When identifying the causes of a disease, auscultation or listening to the affected areas plays an important role. Any qualified specialist will say that fibrinous pleurisy during auscultation is characterized by an accurate determination of the location and type of detected noise.
X-ray examination is the most widely used. The data obtained is supplemented by blood tests that determine the presence of anemia, leukocytosis or increased ESR. A urine test can reveal total protein, the content of red blood cells or epithelium, and a biochemical blood test determines the presence of foreign bodies - sialic acids and fibrinogen.
Detection of fibrinous-purulent pleurisy is possible using a microslide - a glass slide on which the test material is placed. All infected samples are examined under a microscope, after which the causes of the disease are determined. The diagnosis can be definitively confirmed by X-ray or ultrasound examination. These methods make it possible to accurately determine the areas of the pleura covered with fibrin, as well as the sites of fusion of the petals.
Reasons for decreased fibrinogen
Intoxication can cause low fibrinogen
- Chronic liver diseases with symptoms of insufficiency of its synthetic function (chronic hepatitis of a high degree of activity, or cirrhosis of any etiology);
- Poisoning of any etiology;
- Pregnancy;
- Disseminated intravascular coagulation syndrome during the period of widespread thrombosis of small vessels (the consumption of fibrinogen and fibrin at the local level is increased, so the total concentration of plasma fibrinogen decreases), during the period of hypocoagulation;
- Overdose of fibrinolytic drugs (streptokinase, alteplase, human fibrinolysin);
- congenital disorder of fibrinogen synthesis.
Granulation tissue formation
After just two days, in areas free of blood clots and necrotic tissue, you can notice pink-red nodules - the size of millet granules. On the third day, the number of granules increases significantly and already on the 4-5th day the surface of the wound is covered with young granulation tissue. This process is clearly noticeable on an incised wound.
Due to the fact that in a gaping wound it is impossible for newly formed capillaries to connect with the capillaries of the opposite side of the wound, they bend and form loops. Each of these loops is a framework for the above cells. Each new granule is formed from them. Every day the wound is filled with more and more granules, so the entire cavity is completely contracted.
Functions of fibrin protein
Fibrin is involved in the regeneration of nerve fibers
The fibrin protein does not have many physiological functions, but each of them is very important for the body. There are a few of them:
- Stop bleeding. When the tissue is damaged and bleeding begins, a rapid (in the absence of blood clotting pathologies) transformation of fibrogen into fibrin occurs. Fibrin forms a blood clot, which clogs the vessel and prevents blood loss.
- Anti-inflammatory effect. Once at the site of inflammation, fibrin envelops pathogenic agents and prevents them from entering healthy tissue.
- Participation in the process of regeneration of nerve tissue.
When fibrin fulfills its biological function, the body tends to reduce its concentration in the blood. This process is called fibrinolysis - the process of dissolving blood clots and blood clots.
Details about blood coagulogram parameters
Causes of low fibrinogen:
- donation, taking steroids, etc.
- chronically low levels of fibrinogen, impaired synthesis from birth;
- liver diseases;
- unbalanced diet.
Reduced protein concentrations characterize the inability to fully coagulate blood and a tendency to spontaneous bleeding.
Increased fibrinogen level:
- inflammatory processes, alas, the most varied - acute pharyngitis, rheumatoid arthritis, infectious mononucleosis, pyelonephritis, etc.;
- massive tissue destruction (sepsis, lung abscesses, gangrene, ulcers, etc.);
- tumor formation;
- heart attack, stroke, cerebrovascular accident;
- peripheral vascular diseases (atherosclerosis of the arteries, vascular damage in diabetes mellitus, thrombophlebitis, chronic venous insufficiency);
An increased or decreased fibrinogen level does not always indicate health problems.
A minor effect on the indicator in an adult can also be exerted by:
- smoking;
- taking hormonal-based contraceptives, estrogens;
- loads;
- stress;
- diabetes;
- cholesterol;
- obesity.
In adults, the norm ranges from 2-4 g/l, in pregnant women up to 6 g/l, in children the fibrinogen content is 1.25–3 g/l.
Activated partial thromboplastin time (aPTT):
Characterizes the period of time required for the platelet reaction. An increased thromboplastin time characterizes a tendency to uncontrolled bleeding and prolonged blood clotting.
The aPTT concentration can also be affected by high levels of lipids in the blood and the presence of heparin impurities in the blood sample.
– 24-35 seconds, the norm for men is 14-20 s.
Lupus anticoagulant:
Immunoglobulin identifying antibodies. Antibodies affect platelet response time. Must always be zero. An increased concentration indicates the presence of autoimmune diseases, thromboembolism, Libman-Sachs disease (lupus), cerebrovascular accident, as well as infertility and AIDS.
Adhesion, aggregation:
Adhesion is the adhesion of platelets to a damaged surface. A decrease indicates kidney disease, leukemia; increased – atherosclerosis, thrombosis, heart attack, diabetes mellitus. The norm for women carrying a child is usually higher (see table below).
Prothrombin and antithrombin:
Proteins involved in the formation and resorption of blood clots. Prothrombin is formed in the liver.
Thrombin time is a special laboratory generally accepted indicator that characterizes the external pathway of hemostasis activation.
Prothrombin index (PTI) - the indicator is measured as a percentage and characterizes the time of the 2nd stage of coagulation - the formation of proteins. PTI norm is 72-123%.
A PTI blood test can indicate diseases of the abdominal organs (liver and gastrointestinal tract). Increased prothrombin indicates:
- thromboembolism;
- pre-infarction state;
- polycythemia;
- malignant formation.
Decreased indicates an acquired deficiency or a deficiency from birth. Often, decreased prothrombin characterizes vitamin K deficiency. Prothrombin is the main important indicator for diagnosing hemostasis.
International normalized ratio (INR):
INR blood test allows you to systematize blood coagulogram data. The ratio (INR) was developed by the International Committee on Thrombosis and Hemostasis and the International Committee for Standardization in Hematology for ease of drug prescribing.
Using the INR indicator, doctors assess the effect of prescribed medications.
D-dimer:
After the destruction of the blood clot (during the breakdown of fibrin), a protein fragment - D-dimer - is observed in the blood. After restoration of the affected part of the body, the protein plasmin is formed, which destroys and destroys blood clots.
The number of fragments in the blood allows us to identify the work of two processes at once: the formation of blood clots and their dissolution (fibrinolysis). A balance is required between thrombus formation and fibrinolysis. Lack of balance informs hemostasis.
The norms for indicators in adults and children are presented in the table below. Deciphering the blood coagulogram will reveal the discrepancy in each indicator: what it is and how much it should be.
Soluble fibrin-monomer complexes (SFMC):
Few people have heard of the RFMK blood test. The RFMC blood test is an additional indicator; it is included in the coagulogram and is considered an important laboratory test that characterizes the hemostatic system. Many experts consider the RFMC blood test to be an indicator of thrombinemia (the formation of small blood clots) and the onset of DIC.
What does a smear show on flora in women: main analysis indicators
A study of vaginal flora is necessary to identify and identify bacteria and determine the degree of their danger. This method is the least expensive and popular for diagnosing inflammatory processes and diseases that can be contracted during sexual intercourse.
The advantage of this method is that taking a smear for analysis is completely painless. When taking a smear, minor subjective discomfort is possible. A smear is taken during an examination by a gynecologist, then a sample of vaginal contents is placed on a laboratory glass.
Later, upon arrival at the laboratory, the sample is stained to distinguish and identify microbes.
What does a gynecological smear show on vaginal flora in women, what infections can we talk about? Let's discuss further.
Main indicators in gynecological analysis
The vaginal environment in women is not normally sterile.
Many microorganisms constitute the vaginal flora. Among these microorganisms there is constant competition for space and food.
The most common representatives of the vaginal flora are lactobacteria and bifidobacteria .
In many ways, they themselves determine the microclimate of their habitat, releasing alcohol, peroxide, and acids, including lactic acid, in the process of their life, as a result of which the pH of the vaginal environment has a value in a smear on the flora, which characterizes an acidic environment.
These bacteria secrete enzymes that prevent other microbes from multiplying.
So what does a smear reveal for flora in women?
Leukocytes and red blood cells
The number of white and red blood cells is determined in the selected smear. The norm for a healthy woman is 10–15 leukocytes, and about 2 erythrocytes.
If the analysis is taken immediately after menstruation , then the number of leukocytes can be up to 25. If the patient is pregnant, then the leukocyte level is allowed to be no more than 30.
A lot of white blood cells indicate an infectious disease, then you need to retake the test.
Here you need to take into account all conditions that additionally affect the level of leukocytes - pregnancy, menstruation, colds. If all these cases are excluded, then an inflammatory process is suspected.
Phagocytosis
What does phagocytosis mean in a flora smear? Phagocytosis is the process of capture and destruction of foreign cells (for example, pathogenic bacteria) by leukocytes.
The smear may reveal incomplete phagocytosis - the presence of undigested microbial cells inside leukocytes. This happens when there is an infection or if the body is exposed to:
- stress;
- unfavorable ecology;
- poor nutrition.
Cytolysis
Cytolysis in the analysis means the presence in the vagina of a non-inflammatory process caused by the excessive proliferation of a special type of lactobacilli that produce hydrogen.
Their uncontrolled growth leads to alkalization of the vaginal environment and cytolysis (destruction) of epithelial cells.
Epithelium
What does a large amount of epithelium in a smear on the flora in women indicate, what to do if there is a lot of it?
The presence of squamous epithelium in a smear for flora in women is the norm, provided that it has a certain type and quantity.
It is considered normal to have 5 to 10 squamous epithelial cells in the selected sample.
When taking a smear test for flora at a gynecologist, deviations from the norm:
- Decreased or absent epithelial cells, indicating death of the epithelium due to increased testosterone levels and/or decreased estrogen levels.
- A significant excess of epithelial cells in the smear may appear for the following reasons:
- inflammation in the mucous layer of the vaginal walls;
- diseases that can be contracted during coitus;
- vaginitis;
- candidiasis;
- inflammation of the cervix and urethra;
- renal and genitourinary infectious and other diseases.
Ectopia is not a disease, but requires observation.
Fibrin
Fibrin is a blood plasma protein. Its detection in a smear means the presence of an inflammatory process.
Slime
In healthy patients, mucus can be found exclusively in a vaginal smear. If mucus is found, for example, in the urethra, then this indicates inflammation. A vaginal sample may normally have moderate or low amounts of mucus, designated ++ and +, respectively.
In addition, excess mucus may indicate poor hygiene or improper smear sampling.
Doderlein sticks
Doderlein bacilli should normally predominate in the vaginal microflora.
These are lactobacilli that secrete lactic acid , which is necessary for the formation of normal vaginal microflora.
If lactobacilli are present in the vagina in sufficient quantities, infections do not develop there, since lactic acid prevents other bacteria from multiplying.
If the number of these beneficial microorganisms is reduced, then the vaginal pH shifts to the alkaline side. Inflammation may occur.
In a normal smear, lactobacilli make up 95% of the total flora.
Opportunistic flora
In gynecology, opportunistic microbes are those microbes in a flora smear that may not cause any diseases until they begin to multiply excessively. The main types of such microbes:
- cocci;
- ureaplasma;
- diphtheroids;
- Candida mushrooms.
Cocci
Cocci are round shaped bacteria.
According to the staining method, there are gram-positive and gram-negative.
Gram-positive cocci (staphylococci, streptococci and enterococci) are opportunistic, their presence is considered normal within the following limits:
- staphylococci – up to 104;
- streptococci – up to 105;
- enterococci – up to 105.
Gram-negative cocci are causative agents of dangerous diseases. These include gonococci, the causative agents of gonorrhea.
Ureaplasma
These are very small bacteria that, when multiplied above 104 units, cause inflammatory diseases. They prevent conception.
Leptothrix
This is a representative of the anaerobic UP flora, a gram-positive rod-shaped microorganism. Leptothrix itself in a flora smear is dangerous only during pregnancy and can cause a miscarriage.
In non-pregnant patients, the discovery of leptothrix is not a cause for concern.
Diphtheroids
As representatives of the UP flora, they can be present in a smear in small quantities. When their level is exceeded, vaginosis begins . Diphtheroids are similar to the bacteria that cause diphtheria, Corynebacterium.
If corynobacteria were found in the flora smear, their quantity is determined. In case of moderate amounts, a course of drug treatment is prescribed.
If corynebacteria are more than a certain threshold, then additional research needs to be carried out for the presence of other infections, since these bacteria are often associated with others.
Klebsiella
A representative of the flora, Klebsiella under certain conditions (with decreased immunity, pregnancy) can cause urinary tract diseases .
Candida mushrooms (soor)
What does a positive soor in a flora smear give? If fungi of the genus Candida are isolated from a smear, this indicates candidiasis.
These fungi are also representatives of the UP flora; they are introduced into the vagina from the outside. Candidiasis is caused by decreased immunity.
With candidiasis, a smear on the flora can be found:
- filaments of pseudomycelium (mycelium). Pseudomycelium is represented by filamentous growths of blastospores with constrictions.
- blastospores (spores). If blastospores are detected in the analysis of a vaginal smear for flora, it means that the woman’s body is affected by candidiasis. The number of blastospores depends on the prevalence and stage of the disease. Blastospores are embryonic forms of cells formed by budding from maternal forms of cells. If blastospores are found in a smear on the flora, it is necessary to examine the female body for yeast spores of fungi.
Key (atypical) cells
The key cells in a smear for flora are epithelial cells on the surface of which microorganisms have collected (this is especially typical for gardnerella in women, which causes bacterial vaginosis). The presence of atypical cells in a smear is a sign of an infectious disease .
Scarcity and abundance
Based on a smear sample, the type of microflora is determined:
- scanty - contains only lactobacilli;
- medium – lactobacilli + up to 10 leukocytes;
- mixed – lactobacilli + up to 30 leukocytes + cocci;
- abundant - almost no lactobacilli, a lot of leukocytes, mucus and cocci.
What determines the degree of purity
Based on the results of analyzing a smear sample for flora, the degrees of vaginal cleanliness are distinguished:
- The flora is mainly represented by lactobacilli. Few white blood cells, moderate amount of epithelial cells, moderate amount of mucus. Normal, good local immunity.
- The flora is represented by lactobacilli + cocci + yeast. Few white blood cells, moderate amount of epithelial cells, moderate amount of mucus. Variant of the norm.
- The number of leukocytes is increased. Flora – cocci, yeasts, fungi, lactobacilli are few. Lots of epithelial cells and mucus. An inflammatory process that requires treatment.
- White blood cells are everywhere. Flora – cocci, yeast, fungi, lactobacilli no. Lots of epithelial cells and mucus. Severe inflammatory process requires treatment.
With 1 and 2 degrees of purity, the environment in the vagina is acidic and slightly acidic, in the case of 3 and 4 - slightly alkaline and alkaline, respectively.
Source: https://beautyladi.ru/chto-pokazyvaet-mazok-na-floru/
Causes of erosion
One of the versions that substantiates the appearance of an erosive process in the stomach is the vital activity of infectious bacteria Helicobacter pylori. This version is confirmed by the detection of antibodies to infection in the blood of over 90% of the examined patients.
Risk factors for the development of erosive gastritis are:
- intoxication and burns on the surface of the stomach;
- surgical manipulations on the digestive tract and heart, organ transplantation and any type of abdominal surgery;
- long-term depression with stress, states of shock and nervous shock;
- gastropathy due to the use of NSAIDs, antiarrhythmic drugs, analgesics, corticosteroids;
- eating poorly chewed, rough, spicy, hot food;
- smoking and alcohol abuse;
- throwing bile into the gastric sac;
- a high increase in the acidity level of gastric juice with a simultaneous decrease in the resistance of the membrane.
In some situations, the appearance of erosive damage to the stomach with the simultaneous presence of benign and malignant neoplasms, inflammatory pathologies of the stomach, lungs and liver, and pathologies of the cardiovascular system is noted. Thrombosis or stagnation of blood in the portal vein is often combined with erosive gastritis. Hemorrhagic erosions are often a complication of a hiatal hernia, concentrated near it.
RFMK analysis
To determine RFMC in the blood, various types of tests are carried out, the mechanism of which is based on the ability of certain chemicals to lead to the rapid combination of existing RFMC and the formation of a gel-like substance - an analogue of a blood clot.
The most commonly used are the ethanol and protamine sulfate tests. Both of these substances, when mixed with the test plasma, cause a gel-like clot to fall to the bottom of the test tube in the presence of RFMC. To determine specific concentration indicators, blood plasma is diluted with a neutral buffer solution, the numerical answer determines the last positive result (at the maximum dilution). Many laboratories use automatic analyzers - special devices that calculate the concentration of RFMK.
Enzyme treatment
Recently, special attention has been paid to the properties of enzymes. This is especially true for proteases. To treat fibrin enzymes, substances of this type are used. They help dissolve excess protein, thereby preventing serious complications such as blood clots.
The properties of proteolytic enzymes are different. They are able to have fibrinolytic and immunomodulatory effects on the body, as well as improve blood circulation and work as decongestants and anti-inflammatory substances.
Since thrombus formation is based on the production of fibrin, a protease is needed that causes the breakdown of this substance. Without such an enzyme, it is impossible to break the protein into molecules, therefore, there will be no improvement in blood microcirculation.
With local exposure to protease, it is possible to remove necrotic plaque, resolve fibrinous formation, and liquefy viscous secretions.
5.2.4. Coagulation in vivo
The distinction between “internal” and “external” pathways of the coagulation cascade is arbitrary and is used, firstly, for didactic reasons, and, secondly, it simplifies the interpretation of the results of in vitro coagulation tests.
In the body, the “external” and “internal” pathways are not isolated from each other, but represent a single system. Thus, in patients with hereditary deficiency of factor XII, prekallikrein or ICH, APTT is increased (a test that reproduces the internal coagulation pathway in vivo), but there is no hemorrhagic syndrome (on the contrary, thrombosis may be observed due to hypoactivation of fibrinolysis). Therefore, these proteins are not essential components for the functioning of hemostasis in vivo. “Contact” factors appear to be of limited importance in coagulation to stop bleeding, but are necessary for the formation of fibrin during the inflammatory reaction, during wound healing, and, in addition, carry out the internal triggering of fibrinolysis.
External (fast) activation has a dominant role in triggering hemostasis. TF is the key to initiating coagulation. In case of tissue damage and disruption of the integrity of the vascular cell wall ,
those not included in the vascular walls and blood come into contact with the plasma, which leads to the immediate formation of a complex in the plasma.
TF intake can also occur when:
a) intensive movement of fluid from tissues into the blood (blood loss, dehydration, decrease in blood volume);
b) activation of endothelial cells, monocytes and macrophages (blood stasis, hypoxia, acidosis, action of various proteases and other substances);
c) entry into the bloodstream of heterogeneous thromboplastin (for example, with amniotic fluid embolism).
The formation of the TF-VIIa-Ca 2+ complex directly leads to the activation of factor X and, ultimately, to the formation of a fibrin clot.
Thus, the VII-TF-Ca 2+ complex plays a major role in the coagulation cascade in vivo.
The coagulation cascade is like an avalanche: from the moment blood coagulation starts to the formation of fibrin, there is an intensive increase in the number of sequentially activated molecules. Thus, one molecule of factor IXa activates several dozen molecules of factor X, and one molecule of Xa activates many molecules of factor II (prothrombin). It is in connection with the presence of this mechanism that the theory of coagulation functioning is called “cascade”. If a few milligrams of plasma factors are needed to trigger coagulation (for example, the concentration of factor VII is 5 mg/l, factor XII is 30 mg/l, and for effective blood clotting it is enough
=======================================================================
Fibrin is a solid, insoluble protein, consisting of fibrous, rather long, threads. Fibrin is a protein that is unstable in plasma, so it simply does not circulate in the blood.
.
Fibrin owes its formation to an extraordinary situation that activates the hemostasis system, such as damage to the vascular wall as a result of injury or, for example, an inflammatory reaction at the site of formation of an atherosclerotic plaque
. And in the bloodstream there is its precursor - soluble (first blood coagulation factor - FI), which, like many other proteins, is synthesized in the liver parenchyma and in response to damage to the blood vessel under the enzymatic influence of thrombin on the wound is converted into fibrin.
When fibrin is no longer needed, the fibrinolytic system dissolves the clot (fibrinolysis). Experts believe that in the blood there is a constant process of converting some very small amount of fibrinogen into fibrin, but this problem is also constantly solved by fibrinolysis.
There is no standard for fibrin itself in clinical laboratory diagnostics. Since this substance is not normally detected in the blood
, analysis examining this indicator is not performed. The quantity and quality of fibrin is judged by the level of fibrinogen in the blood, also examining other factors of the coagulation system in the composition.
Introduction
At a time when surgeons widely used gastric resection in the treatment of patients with peptic ulcers, the outstanding Soviet surgeon, then head of the Department of Surgery at Irkutsk University, Prof. V.S. Leviticus said: “Stomachs are also needed in Siberia...”. This thesis regarding the spleen could become an epigraph to this article.
Injuries to the spleen are a severe injury to the abdominal organs, and their incidence ranges from 17 to 23% [1-4], and is steadily increasing.
Currently, outdated ideas about the “uselessness” of the spleen as an organ are being revised. At the same time, ideas about the role of the spleen in the body and the complex of pathological changes associated with its removal have become significantly more complicated.
The functions of the spleen are normally divided into primary and secondary. The main, or protective, functions, the loss of which can threaten life, include: removal of corpuscular antigens from the bloodstream, i.e. mechanical blood filtration function. After this, determined lymphocytes are activated to transform into immunocompetent cells. In the thymus-dependent zone of the white pulp, the formation of lymphoblasts occurs, in the thymus-independent zone there is proliferation of lymphocytes and the formation of plasma cells. This is how another important function of the organ is realized - the formation of antibodies. In addition, the main functions of the spleen include the synthesis of properdin and some other peptides that modulate phagocytic activity [5-7]. The secondary functions of the spleen are the destruction of pathologically altered blood cells, especially red blood cells; participation in iron metabolism and bilirubin formation; depository role of the organ.
Thus, the spleen is a department of the lymphatic system and acts as an organ of the system of phagocytic mononuclear cells. The loss of the spleen triggers certain mechanisms to compensate for lost functions, but it is almost impossible to completely compensate for its absence, and this leads to the development of post-splenectomy hyposplenism syndrome. This syndrome is dangerous due to the occurrence of increased susceptibility to surgical infection, up to the development of fulminant sepsis, as well as a predisposition to parasitic, fungal and viral diseases [8-13]. In this regard, any method proposed for organ preservation should be welcomed, carefully analyzed and, if possible, introduced into widespread surgical practice.
The spleen is covered with a thin connective tissue capsule and on top of it the visceral peritoneum is still closely fused with it. Due to the abundance of blood vessels and the looseness of the pulp, the slightest trauma to the organ can lead to rupture of the capsule and damage to the parenchyma, which are accompanied by massive bleeding. Even minor decapsulation of the spleen causes bleeding that does not stop on its own [14-16].
Despite a fairly wide range of standard methods for stopping bleeding in cases of damage to the spleen (special sutures, compressive hemostatic meshes, various types of coagulation, etc.), splenectomy is performed even with injuries that are insignificant in area and depth [17, 18].
Recently, due to the recognition of the importance of spleen preservation, interest in splenorrhaphy has been revived [1, 19, 20]. However, since the spleen has a dense network of vessels, a small amount of connective tissue and deposits large volumes of blood, the sutures often cut through, and quite severe bleeding occurs from the injection sites. The result most often is splenectomy. The well-known disadvantages of suturing the spleen stimulate the search for new methods of local hemostasis, one of which is compression of the organ with a hemostatic mesh [8, 21].
Physical methods of stopping bleeding were also used in ancient times - cauterization with hot objects, exposure to hot or cold solutions, steam, ice, etc. Thanks to technical progress, electrocoagulation has become widespread; other contact modifications, such as thermocoagulation, laser, ultrasound, plasma coagulation, etc., are less in demand. [22-24].
Over the past three decades, the interests of surgeons have been associated with the hemostatic capabilities of adhesive substances. Of these agents, the most widely known are cyanoacrylate adhesives, the properties of which have been well studied in traumatic injuries of the liver, its resections and operations on the pancreas. The experience of using these adhesive compositions for splenic trauma is very limited [8]. A study of morphological substrates in the area of glue application showed the formation of coagulation necrosis and aseptic inflammation, which in a number of cases led to the appearance of secondary bleeding.
Interesting message from V.A. Kubyshkina et al. [25] on the use of biological absorbable glue “Rabrom-Pax” for benign tumors of the spleen. The authors were able to perform organ-preserving operations, and the separated parts of the spleen were connected with a substance without seams and strengthened with a greater omentum. Unfortunately, the composition of the drug is not reported.
Adhesives based on fibrin polymers are considered the most promising means of biological hemostasis [26]. The main advantage is their composition from biological blood components; when applied to a damaged area, they imitate the physiological mechanism of hemostasis. However, fibrin compositions, as a rule, are two-component and are applied to tissues using injection needles, sprays, catheters, and double-syringe applicators are used, which creates certain difficulties when using them in emergency surgery.
The hemostatic capabilities of such biological hemostasis agents as dry thrombin and collagen sponge are limited due to poor fixation to the wound surface.
The successful combination of collagen substance and fibrin glue components is reflected in the TachoComb preparation.
Indications for the use of one or another method of hemostasis have not been sufficiently developed, as a result of which the very idea of organ-preserving operations may be discredited [27, 28].
The purpose of our study is to experimentally substantiate and clinically confirm the hemostatic capabilities of the fibrin-collagen substance (FCS) TachoComb for spleen injuries.
Material and methods
FCS "TachoComb" (Austria) is a ready-to-use sterile collagen plate coated with fibrin glue components consisting of fibrinogen, thrombin and aprotinin. Upon contact with a bleeding surface, the clotting factors contained in the collagen covering layer are released and thrombin converts fibrinogen into fibrin, which provides a powerful hemostatic effect.
The hemostatic properties of FCS were compared with those of the hemostatic collagen sponge - GCG (Russia), Tabotamp (TB) - oxygenated cellulose (USA), Gelaspon (TC) - foamed gelatin (Germany).
The hemostasis experiment was performed on 24 mongrel dogs: 6 animals were taken into the acute experiment, 18 - into the chronic one.
The hemostasis experiment was carried out according to the following scheme. On the free surfaces of the spleen, rectangular wounds with a depth of 3 mm and an area of 4 cm2 (2×2 cm) were made using a standard method using a sharp method. The intensity of bleeding was assessed using the method of weighing napkins, collecting the flowing blood for 15 s. After determining the intensity of bleeding, plates of GCG, TB, GS and FKS with an area of 9 cm2 (3x3 cm) were placed on the wound and pressed tightly and held for 3 minutes. Then the pressure was removed and the time of bleeding cessation was determined by imprints on clean gauze pads. The intensity of bleeding (if any) was determined by the same method as before application. As a control, we used the simultaneous application of wounds of the same area and configuration in a remote location of the organ. Bleeding was stopped by applying pressure with a dry, clean gauze pad.
In chronic experiments, pathomorphological changes in the wounded area and the results of FCS application were studied. In this case, the material was obtained from animals under sterile conditions under anesthesia on the 1st, 3rd, 7th, 14th, 30th, 60th day after bleeding stopped. To do this, pieces of tissue were taken with scissors from the areas where the bleeding wound was simulated. Samples were fixed in 10% formaldehyde, embedded in paraffin according to standard techniques, sections (4-5 µm) were stained with hematoxylin and eosin and picrofuchsin according to Van Gieson. Microscopic examination of the preparations was carried out with working magnifications of a light microscope of 100, 200 and 400 times. During the morphological study, special attention was paid to the dynamics of the vascular reaction and the course of the inflammatory process. In addition, macroscopic changes occurring in the drug and control wounds at the same time were assessed.
In clinical practice, operations for splenic trauma were performed in 75 patients. The analysis of the results was carried out over 10 years (1999-2008).
The technique for applying FCS to splenic wounds depends on the depth and location of parenchymal damage. In case of decapsulation of an organ on any surface, it is enough to apply a plate of the drug and fix it tightly. In case of ruptures of the spleen along the diaphragmatic surface, it is necessary to pinch the vascular pedicle with your fingers before application and hold it for the entire period of fixation, otherwise blood may leak from under the edge of the plate. Hemostasis of central ruptures (in the area of the vascular pedicle) of the spleen using FCS is unacceptable, since there is a high risk of secondary bleeding. Splenectomy should be resorted to.
Results and discussion
Under the conditions of an acute experiment, a comparative assessment of the hemostatic effectiveness of the presented drugs when inflicting flat wounds of the spleen was carried out.
In table 1
data are presented for determining the intensity of bleeding when using various biopolymers applied to splenic wounds and held for 3 minutes.
After application of GCG and TB to splenic wounds, the intensity of bleeding decreased by 4 and 5 times, respectively. The GS drug stopped bleeding significantly worse (from 2117.3±234.5 to 1331.3±232.8 ml/min), although the difference in results was significant. When using the FKS biopolymer, the bleeding stopped completely.
Within 10 minutes, complete cessation of bleeding occurred with the use of FCS (2.8±0.7 min) and TB (9.3±0.5 min). GCG and GS did not stop bleeding during these periods.
Thus, the hemostatic activity of biopolymers GCG, TB and GS when applied to spleen wounds turned out to be clearly insufficient. In a similar situation, the FKS biopolymer stopped bleeding within 3 minutes.
In a chronic experiment, we studied the processes occurring in the area of application of FCS and its involution at various times.
A study of the healing of splenic wounds closed with FCS biopolymer showed that the inflammatory reaction in the wounds is of an aseptic post-traumatic nature and completely subsides by the 7th day after surgery. The FCS plate does not cause acute inflammation or local toxic reactions in tissues. The biopolymer stimulates early activation of the fibroblastic reaction and angiogenesis. The mesothelial cover is restored on the surface of the plate on days 7-14. Biodegradation of FCS occurs after 30 days of application of the drug to liver wounds and occurs by replacing collagen with delicate scar tissue with further absorption by macrophages.
Clinical data
We analyzed 75 case histories of patients with splenic injury. Their average age was 35.4±3.2 years. Among the patients there were 71 men and 4 women. Blunt abdominal trauma was observed in 47 patients, iatrogenic injuries to the spleen were noted in 28 people. These injuries were caused by decapsulation of the organ during traction during gastrectomy or gastrectomy, during sanitation of the abdominal cavity due to peritonitis, during revision of the abdominal cavity.
Types of surgical procedures for spleen injuries are presented in Table. 2.
In 24 cases with massive injuries of the spleen (III-IV degrees), splenectomy was forced to be performed. In 5 cases during iatrogenic decapsulation, the spleen had to be removed due to the lack of FCS in the operating room.
In 46 patients, during the first operation, it was possible to preserve the organ by using electrocoagulation with the application of GCG and tight packing (4 patients) and application of the FCS biopolymer (42 patients).
Of the 4 patients whose bleeding was stopped by electrocoagulation and GCG application, 3 underwent reoperation due to developed bleeding and splenectomy was performed. In one observation, hemostasis was achieved, but a subdiaphragmatic abscess occurred, which required opening and drainage.
In 42 patients, bleeding was stopped by application of FCS. In 19 patients of this group, fairly extensive iatrogenic damage was observed (over an area of more than 2 cm). 23 patients were admitted with blunt abdominal trauma; laparotomy revealed a grade I-II rupture of splenic tissue. In all observations, the application of FCS biopolymer plates made it possible to achieve reliable hemostasis and avoid splenectomy. At the beginning of mastering the technique, in one case of damage to the spleen in the hilum area, we were forced to use two FCS plates, since after applying the first plate, blood leaked from under the edge of the platinum. Hemostasis was insufficient due to the fact that heavy bleeding did not allow the drug to fully demonstrate its adhesive capabilities. After short-term clamping of the supply vessels, complete hemostasis was achieved with another plate of the substance.
In not a single observation of hemostasis in cases of spleen injury through the application of FCS, recurrent bleeding was noted, and there were no complications associated with the surgical area.
Here are two clinical observations. The first demonstrates hemostasis from a fairly extensive injury to the splenic tissue.
Patient K.,
37 years old, was admitted with a clinical picture of intra-abdominal bleeding while intoxicated and in a state of second degree hemorrhagic shock. He doesn’t remember the time of injury and doesn’t name the cause. Symptoms of anemia are expressed. The patient underwent emergency surgery. Up to 1 liter of blood with clots was found in the abdominal cavity, which were removed. During the audit, a diagnosis of splenic rupture (6×3×2 cm along the diaphragmatic surface) and hematoma of the greater omentum was established. Attention was drawn to the large size of the spleen and signs of developing cirrhosis of the liver with the presence of portal hypertension. Bleeding from a ruptured spleen was stopped by applying FKS biopolymer in one layer. The patient was discharged for outpatient treatment on the 9th day. No complications were observed.
This observation is demonstrative in that bleeding from the splenic parenchyma was stopped in conditions of portal hypertension caused by liver cirrhosis, apparently of alcoholic origin.
The second observation concerns iatrogenic damage to the spleen caused by draining the abdominal cavity in a patient with widespread peritonitis.
Patient K.,
60 years old, admitted on May 22, 2001 with a diagnosis of blunt abdominal trauma, peritonitis. The circumstances and timing of the injury are not reported. The condition is serious. Anemic. There are peritoneal symptoms. After 2 hours of preoperative preparation, diagnostic laparoscopy was performed, which revealed widespread purulent peritonitis. After laparotomy, a rupture of the ileum along the antimesenteric edge measuring 1×0.5 cm was found, which was the cause of severe peritonitis with multiple fibrinous deposits on the peritoneum and the development of paralytic intestinal obstruction. The wound of the small intestine is sutured. The abdominal cavity is washed and dried. Nasointestinal intubation was performed. The patient was in the intensive care unit, where he received intensive care. On May 23, 24 and 26, inspections and sanitation of the abdominal cavity were carried out, included in the peritonitis treatment program. During the last sanitation of the abdominal cavity, the spleen was damaged - decapsulation of the organ measuring 2x3 cm and active bleeding were observed. The bleeding was stopped by applying a plate of FCS biopolymer pre-moistened in a solution of an antibacterial drug. A control drain was installed in the left subphrenic space. No more sanitation of the abdominal cavity was performed, since the phenomena of peritonitis resolved and no revisions were required. No blood discharge through the drainage was observed. The drainage was removed on the 3rd day after the last relaparotomy. The patient recovered.
Thus, experimental and clinical data from a study of the results of using FCS for spleen injuries suggest the emergence of a promising drug that expands the possibilities of final hemostasis. The use of the FCS biopolymer in both traumatic and iatrogenic injuries of the spleen was successful, and hemostasis was carried out not only in “normal” situations, but also in the presence of aggravating factors - portal hypertension and peritonitis. No complications or secondary bleeding were observed.
Causes and symptoms
As soon as a yellow coating appears on the tongue, the reasons for its formation may be hidden in the work of internal organs, as well as in the reaction of the mucous membrane to external irritants. The most common reasons include:
- Indigestion;
- Early stage of pancreatic and liver diseases;
- Side effect of taking vitamins and antibiotics;
- Angina;
- Blockage of the bile ducts.
Each of these reasons can only be a direction for further research, but often they occur simultaneously, while the yellow tongue stably maintains the density of plaque and its location, without reacting in any way to treatment attempts.
The main symptom, in addition to visual changes, will be bad breath, which persists even with regular brushing of teeth and use of mouthwash.