Causes of jaw tumors
Tumor diseases tend to change their nature of origin, which is why it is not possible to name a single cause for the occurrence of a tumor in the jaw. Modern medicine continues to study various types of circumstances that provoke a tumor process in the jaw. The only reason for the appearance of a tumor, as all experts believe, is a jaw injury. In all other respects, opinions differ to a greater or lesser extent. The nature of the injury can be either prolonged (internal injury to the oral mucosa) or isolated (bruise of the jaw). Also a common cause of the disease are foreign bodies (material for filling a tooth or its root) and inflammatory processes that develop over a long time.
Adverse habits such as smoking and poor oral hygiene contribute to the occurrence of neoplasms. There is a high probability of a jaw tumor appearing during chemotherapy and radiotherapy treatment.
Tumors of the jaws can manifest themselves as a distant focus of cancer pathology.
Classification of jaw tumors
Tumors of the jaws are of the following types:
- Odontogenic - organ-nonspecific formations associated with the tissues that form the tooth.
- Nonodontogenic - organ-specific formations associated with bone.
In addition to this classification, tumors can be benign or malignant, occurring in epithelial (epithelial) or mesenchymal (mesenchymal) tissues. Combined neoplasms—epithelial-mesenchial—may occur.
The main representatives of benign organ-specific tumors are:
- ameloblastoma;
- odontoma;
- odontogenic fibroma;
- cementoma.
The main representatives of benign organ-nonspecific tumors are:
- osteoma;
- osteoid osteoma;
- osteoblastoclastoma;
- hemangioma.
Malignant organ-specific neoplasms include cancer and sarcoma.
Benign odontogenic tumors
Ameloblastoma. Its characteristic feature is a pronounced change in the shape of the face associated with a violation of symmetry proportions as a result of the development of a tumor located in the lower jaw. The violation of symmetry can be mild or pronounced. The degree of distortion of the face shape is influenced by the size and position of the tumor. For example, the localization of a tumor along the body and ramus of the lower jaw is characterized by a change in the shape of the lower lateral part of the face. The color of the skin does not change, and it can be easily moved in the area of the tumor.
Inflammatory processes accompanying the tumor can give similar symptoms to phlegmon or mandibular osteomyelitis. During palpation, the body of the tumor is felt, which makes it possible to assess the degree of distortion of the shape of the face. The lymph nodes located directly next to the tumor do not change in size, and the deformed area is clearly defined. The formation has a thick filling and a wavy surface. Examination of the oral cavity reveals thickening of the alveolar ridge, soft tissue may be swollen, and teeth tend to shift or move.
Odontoma . Often this type of tumor is diagnosed in adolescence. The tumor has similar symptoms to other tumors localized in the jaw bones. The course of the disease is quite slow and ambiguous. During development, there is a gradual swelling of the jaw bones, which leads to delayed or absent teeth eruption. Large tumor sizes can change the shape of the jaw or contribute to the formation of a fistula. Despite the fact that the course of the disease passes practically without symptoms, the upper layer of the jaw may be damaged, and the tumor itself may contain teeth or their rudiments. When diagnosing, it is necessary to differentiate the tumor from adamantinoma. Odontoma can be simple, complex, soft or mixed.
Odontogenic fibroma . The nature of the development of this neoplasm is very slow; the tumor is mainly diagnosed in young children. A clear symptom of tumor development is impaired teething; pain is not observed during the period of tumor growth. Odontogenic fibroma can be located equally on both jaws and is rarely accompanied by an inflammatory process. It differs from similar neoplasms in its composition, which includes remnants of the epithelium that forms the teeth.
Cementoma . The hallmark of a tumor is the presence of cement-like tissue. The tumor grows quite slowly and is manifested by a change in the shape of the jaw. The tumor is clear and round, has pronounced boundaries, most often affects the upper jaw and is almost always connected to the root of the tooth.
Benign non-odontogenic tumors
Osteoma . This tumor is not often diagnosed, and men are more susceptible to developing osteoma than women. It occurs mainly during adolescence. The development of the tumor occurs without pain, is quite slow and is localized in the nasal cavity, orbit or sinuses of the upper jaw. Tumor growth can occur both inside the jaw bones and on the surface. The mandibular location of the tumor is characterized by pain and a violation of the symmetry of the face, as well as the motor abilities of the jaw in this area. The maxillary localization of the tumor leads to failure of nasal breathing, doubling of the image perceived by the eyes, and bulging of the eyes.
Osteoid osteoma . The main symptom of the development of this tumor is the presence of pain, which intensifies with the progression of the tumor. It is noted that people with osteoid osteoma especially feel increased pain at night. Establishing a correct diagnosis is made difficult by the nature of the pain syndrome, which tends to spread, resulting in the activation of other diseases. In diagnosing a tumor, the action of medications (analgesics) that suppress the occurrence of pain helps. The affected areas appear swollen, and the motor function of the joints is impaired. The difficulty of making a diagnosis is due to the small size of the tumor and the absence of special symptoms.
Osteoblastoclastoma . The tumor is a single separate formation. It is extremely rare to see a double appearance of a tumor on adjacent bones. Mostly young people under the age of 20 are susceptible to developing the disease. The most pronounced symptoms are increased pain in the jaw, impaired facial symmetry and tooth mobility. The manifestation of the main symptoms depends on the location of the tumor. The peri-tumor tissues become pronounced, and fistulas begin to appear. Quite often, patients notice an increase in average body temperature, the cortical layer becomes thin, which can cause a fracture of the lower jaw.
Hemangioma . As an independent disease, it is relatively rare; a combination of hemangioma of soft facial tissues or the oral cavity with a jaw hemangioma is often diagnosed. The disease is characterized by a color change in the mucous membrane to bright red or blue-purple shades. This symptom is the main one at the time of diagnosis. However, diagnosis can be difficult in situations where the soft tissues of the oral cavity are not involved in the inflammatory and tumor process. Increased bleeding of the gums and root canals is considered to be a symptom of isolated hemangioma.
Symptoms of dental periostitis
- slight swelling above the gum,
- enlarged lymph nodes,
- you can easily detect a tooth that has become a source of infection with signs of periodontitis or pulpitis;
- with general intoxication (fever, weakness, sleep disturbance and loss of appetite);
- with pain that spreads from the jaw to the neck, temple, eye area and intensifies with pressure on the tooth;
- with limited mobility in the temporomandibular structure;
- with noticeable swelling of the cheek.
Malignant tumors of the jaws
Malignant jaw tumors are not observed in patients as often as benign ones. Oncological damage is accompanied by pain that has the ability to self-propagate. Teeth become loose and prone to rapid loss. Some tumors, due to their morphological manifestations, can cause fractures of the jaw bones. With the progression of a malignant tumor, erosion of bone tissue is observed, while the growth of the parotid and submandibular glands is noticeable, and the masticatory muscles increase. The source of the disease penetrates the cervical mandibular lymph nodes.
Some tumors affecting the upper jaw extend into the eye socket or nasal cavity. As a result, complications of the disease may occur in the form of bleeding from the nose, a suppurating one-sided runny nose, difficulty with nasal breathing, pain in the head, increased production of tears, bulging eyes and double vision.
Malignant tumors affecting the lower jaw quite quickly penetrate the soft tissues of the mouth and cheeks, begin to bleed, resulting in disruption and difficulty in closing the jaws.
Malignant tumors originating from bone tissue are characterized by rapid progression and penetration into soft tissues, which leads to disruption of facial symmetry, increased pain and the rapid appearance of foci of disease in the lungs and other organs.
Malignant tumors of the upper jaw
Clinical manifestations of malignant neoplasms of the upper jaw are diverse, but not pathognomonic and depend on the initial location of the tumor, prevalence, shape and direction of preferential growth, and morphological structure.
Since epithelial malignant tumors originate from the mucous membrane of the maxillary sinus, in stages 1 - 2 they are usually an accidental finding (for example, during gairotomies), because tumors of such prevalence are not available for visual observation, symptoms may resemble ordinary sinusitis, or even absent. This explains the predominant detection of malignant tumors of the upper jaw in stages III-IV. In a significant proportion of patients, the first symptoms are pain of various types in the upper jaw, radiating to the head. Often the disease is manifested by pathological changes in the nasal cavity: one-sided difficulty or complete absence of nasal breathing, serous-purulent or bloody discharge. More rare first symptoms of malignant tumors of the upper jaw are unilateral profuse lacrimation, swelling of the eyelids or soft tissues of the face of the corresponding side, and impaired skin sensitivity. Some patients, as the first sign of disease, note a tumor in the upper jaw that is already visible to the naked eye.
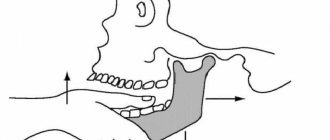
To fully characterize the clinical manifestations of malignant tumors of the upper jaw and accurate topical diagnosis, in 1933 the Swedish oncologist Ohngren proposed a conditional division of the jaw into sectors. It is carried out by drawing an imaginary inclined plane starting from the inner corner of the orbit and going to the corner of the lower jaw. Two sectors or segments are obtained: superior posterior and inferior anterior. The second plane passes sagittally through the center of the maxillary sinus and divides each of the previous segments into lateral and medial parts.
Thus, two lateral and two medial segments arise:
- superoposterior external;
- superoposterior internal;
- inferoanteroexternal;
- inferoanterointernal.
Clinical observations confirm the feasibility and practical significance of the Ongren scheme, since it allows one to accurately determine the location of the tumor, since the lesion of each segment is characterized by certain clinical manifestations. Correct assessment of the symptoms of the disease allows you to timely suspect a malignant tumor and take the necessary measures. The danger hidden in delaying treatment for malignant tumors of the upper jaw is so great that it should be considered justified in all unclear and suspicious cases to resort to a comprehensive examination of the patient.
Neoplasms of the superoposterior outer segment. The main direction of growth of tumors in this localization is the pterygopalatine fossa and the orbit. Neoplasms of this group cause early exophthalmos. In this case, the eyeball shifts inwards, and diplopia appears. Obstruction of lymph and venous outflow associated with tissue germination by a tumor leads to swelling of the eyelids and narrowing of the palpebral fissure on the side of the tumor lesion. As the tumor grows further, facial asymmetry increases.
When a tumor grows into the pterygopalatine and infratemporal fossa, compression of the venous plexuses located here occurs, which impedes the outflow of venous blood and ultimately leads to lymphostasis in the retrobulbar tissue, zygomatic region and lower eyelid. This manifests itself as chemosis in combination with exophthalmos.
As they spread towards the tubercle of the upper jaw, tumors of this segment cause restriction of mouth opening due to contracture of the internal pterygoid muscle under the influence of tumor infiltration of its fibers and, in part, pressure on the coronoid process of the lower jaw branch. Tumors of the superior posteroexternal segment, earlier than other localizations, may be accompanied by the appearance of pain or paresthesia in the area of innervation of the 2nd branch of the trigeminal nerve of the corresponding side. Pain can radiate to the premolars and molars of the upper jaw. When the Eustachian tube grows, pain occurs in the ear area.
Thus, the deep location of malignant tumors of this segment under the cover of such anatomical formations as the zygomatic bone, the tubercle of the upper jaw, the ramus of the lower jaw with the surrounding muscles, leads to a long-term asymptomatic course of the disease. Only after the destruction of the upper or posterior (infratemporal) walls of the maxillary sinus and the beginning of tumor disintegration do symptoms characteristic of malignant growth appear.
Neoplasms of the inferoanteroexternal segment . They tend to spread to the area of the temporomandibular joint (TMJ), infratemporal fossa, oral cavity, and cheeks. Among the first symptoms of tumors of this localization, pain radiating to the ear should be noted, which is due to the involvement of the II and III branches of the trigeminal nerve in the process. In a later period, contracture occurs due to damage to the internal pterygoid and masticatory muscles. With a tendency to spread inward, the lateral wall of the pharynx and the palatine tonsil are affected. With outward growth, facial asymmetry appears. Invasion of the external carotid artery or its branches can lead to heavy, repeated bleeding, one of which can be fatal.
Malignant tumors of this segment do not manifest themselves for a long time; only after the walls of the maxillary sinus are destroyed, the first symptoms of malignant growth are detected, but they are late.
Neoplasms of the superoposterior internal segment . Tumors of this segment tend to spread towards the cells of the ethmoidal labyrinth and orbit (the incidence of the latter is 20-25%). Tumors of this location are also diagnosed late, because located in an area that is difficult to access for research. Infiltrating the tissue of the orbit, the tumor displaces the eyeball anteriorly and laterally, limiting its mobility. Already in the early stages of the disease, patients notice the appearance of lacrimation on the affected side. Later, swelling and hyperemia appear in the area of the inner corner of the eye due to secondary developing dacryocystitis and tumor growth into the lacrimal sac and lacrimal ducts. At this stage, visual acuity usually does not change.
When the tumor spreads towards the nasal cavity, unilateral, first mucous, then mucopurulent or sanguineous discharge appears from the corresponding nasal passage, and difficulty breathing. Sometimes nasal discharge becomes foul-smelling. During rhinoscopy, you can see bleeding tumor masses covered with purulent plaque, resembling granulations, located in the upper part of the nasal cavity. Sometimes it is possible to find out from the anamnesis that the first manifestation of the disease was a distortion or disappearance of the sense of smell, which is associated with damage to the receptor apparatus of the olfactory nerve. Headaches follow.
If the tumor spreads to the ethmoid labyrinth, then varying degrees of exophthalmos may develop with optic nerve atrophy and decreased visual acuity. Often patients are bothered by pain in the area of innervation of the 2nd branch of the trigeminal nerve. There may be a loss of skin sensitivity in the cheek area.
If the tumor tends to spread to the nasopharynx, then from there it often grows into the body of the main bone. This stage is characterized by pain radiating to the temple. Further development of the tumor process can lead to growth into the cranial cavity with the appearance of signs of damage to a number of cranial nerves (II, III, IV, V, VI). Diplopia, decreased visual acuity, neuralgic pain in the superciliary region appear, and the corneal reflex is absent.
Neoplasms of the inferoanterointernal segment . The tumor spreads into the nasal cavity of the corresponding side, as well as onto the anterior wall of the maxillary sinus and the alveolar process of the upper jaw. Tumors of this location are diagnosed relatively early. Gradually destroying the alveolar process, hard palate, and the anterior wall of the maxillary sinus, the tumor grows into the mucous membrane. Bone destruction leads to gradual loosening and loss of often intact teeth. Involvement of the nerve endings of the alveolar processes in the tumor process leads to gradually increasing pain in the teeth and jaw. The destruction of blood vessels causes bleeding gums. The alveolar process is deformed, becomes thickened, as if swollen. Tumor tissue protrudes from the sockets of fallen or removed teeth, bleeding profusely and resembling granulation tissue. When the tumor process spreads to the anterior wall of the maxillary sinus, the nasolabial fold becomes smoother and progressive facial asymmetry appears.
When it grows into the nasal cavity, difficulty or complete absence of (one-sided) nasal breathing occurs, bloody or pus-laced discharge with an unpleasant odor appears, but the sense of smell is not impaired.
Characteristics of the origin of the main symptoms of malignant neoplasms of the upper jaw
For convenience, the variety of symptoms of malignant tumors of the upper jaw can be grouped as ocular, nasal and dental.
The leading symptom of tumors in this location is pain. With primary damage to the maxillary sinus, they occur almost simultaneously with the detection of a tumor or precede the appearance of visual signs of a tumor by 1 to 6 months. They are of the most varied nature, irradiating to different areas of the head. The intensity and nature of pain depend on the type and location of the tumor and the extent of the process. With limited tumor damage, constant dull pain in the upper jaw area predominates, intensifying in a horizontal position and when tilting the head, due to a rush of blood and increased pressure on the nerve trunks. As the tumor spreads towards the alveolar process of the upper jaw, toothaches arise with irradiation to the temple and TMJ. In the later stages, painful constant headaches occur.
The occurrence of toothache often leads to diagnostic errors and interventions on intact teeth, which do not eliminate the pain.
With sarcomas of the upper jaw, pain of a very different nature is observed: dull, aching, boring. Their irradiation is the same as in cancer.
The use of thermal procedures, as well as physical therapy, leads to increased pain and accelerated tumor growth.
The persistence of pain in malignant neoplasms of the upper jaw is a characteristic feature that distinguishes them from inflammatory processes.
Nasal symptoms . In most patients, as the malignant tumor grows, unilateral progressive difficulty breathing is observed until it is completely absent. Discharges of various types appear: mucous, bloody, fetid-purulent. In the early stages, reactive inflammation of the mucous membrane of the maxillary cavity around the focus of tumor growth is observed, which leads to irritation and hypersecretion of the epithelium of the mucous membrane. The transparent mucous discharge from the maxillary cavity enters the nasal cavity through the natural opening in the middle meatus. Patients, as a rule, believe that this is the result of a cold and do not consult a doctor, using vasoconstrictor nasal drops or thermal procedures at home. Subsequently, the secretion becomes purulent due to the addition of a secondary infection. Putrid discharge mixed with blood indicates an advanced process, accompanied by the disintegration of the tumor.
It has been noticed that fetid purulent discharge from the nose is more characteristic of cancer, and putrefactive discharge with streaks of blood is more characteristic of sarcoma of the upper jaw.
Difficulty in nasal breathing . It occurs due to the fact that the tumor, having completely filled the maxillary sinus, displaces its medial wall towards the nasal septum, and in later stages grows into the medial wall of the maxillary sinus, fills the middle and lower nasal passages, displaces and then grows into the nasal septum. At this stage, in addition to copious mucous discharge, nosebleeds appear from the growing tumor tissue. The tumor masses, having filled the nasal passages, protrude from the nasal opening. In the later stages of the disease, the nose shifts to the healthy side.
Difficulty opening the mouth . Contracture is rarely observed in the early stages of the tumor process in the upper jaw. The appearance of this symptom is associated with the tumor growing into the pterygoid, masseter or temporal muscles, i.e., when the tumor has already spread beyond the maxillary sinus. This symptom is typical for tumors located in the posterior sinus near the TMJ. When a tumor grows into a joint, first a reactive inflammation occurs in it, and then the tumor directly grows into it. In addition to contracture, pain in the joint is observed, which intensifies while eating and talking.
Ophthalmological symptoms . Pathological changes in the area of the eyelids, orbit and eyeball often indicate the presence of a malignant tumor of the upper jaw. Observed: unilateral lacrimation, swelling of the eyelids and narrowing of the palpebral fissure, exophthalmos or displacement of the eyeball in various directions, limitation of its mobility, diplopia, decreased visual acuity.
Swelling of the eyelids - occurs as a result of tumor spreading into the eye socket. Due to compression of the blood and lymph outflow pathways, lymphostasis occurs. Swelling can occur due to inflammatory changes of a reactive nature in adjacent soft tissues. Swelling of the lower eyelid causes a narrowing of the palpebral fissure and its upward displacement. When the tumor spreads towards the nasolacrimal duct, one-sided profuse lacrimation is observed.
As the tumor grows towards the orbit, the contours of its lower wall are disrupted. The orbital margin first becomes dense, lumpy, and later areas of softening appear. Almost simultaneously, swelling of the orbital tissue increases, and purulent conjunctivitis develops. Sometimes malignant tumors of the maxillary sinus first spread to the ethmoidal labyrinth and then grow into the orbit, which leads to displacement of the eyeball. The direction of displacement depends on the location and preferred direction of tumor growth. With sarcomas, displacement of the eyeball is observed earlier than with cancer.
The early stages of exophthalmos are usually detected not by the patient himself, but by those around him. Severe exophthalmos leads to impaired closure of the eyelids. Displacement of the eyeball to one side or another causes diplopia. With direct exophthalmos, diplopia does not occur. When the lower wall of the orbit is destroyed, enophthalmos (retraction of the eyeball) is formed.
If a malignant tumor grows into the motor muscles of the eyeball, its mobility is limited and vision is impaired. Tumor infiltration of the eyeball or optic nerve leads first to partial and then complete loss of vision.
Metastasis of malignant tumors of the upper jaw occurs mainly through the lymphogenous route. With sarcomas, hematogenous spread is possible. The outflow of lymph from the paranasal sinuses and upper jaw is carried out into the retropharyngeal and upper deep cervical lymph nodes. From the anterior sections, lymph flows into the submandibular lymph nodes.
Regional metastasis of malignant tumors of the upper jaw is a fairly rare phenomenon. With the upper internal localization of cancer, it was observed in 7.3%, lower - in 14.9% (Paches A.I., 1983). According to Yu.I. Vorobyov, the frequency of regional metastasis of tumors of this localization is generally 21.4%, and poorly differentiated and undifferentiated forms of cancer metastasize more often than differentiated forms of squamous cell carcinoma.
Distant metastases are observed from 3.4 to 9%.
The general condition of patients with malignant tumors of the upper jaw in the early stages may not be affected. But during the period of tumor imaging, a progressive decrease in body weight is usually observed. This can be expressed to varying degrees and depends not only on the stage of the tumor process, but also on the location, growth rate and spread. Thus, with the appearance of early contracture and pain in the TMJ area, weight loss begins earlier and is nutritional in nature due to difficulty eating. During the period of tumor disintegration and the addition of a secondary infection, patients experience symptoms of anemia due to intoxication from the disintegrating tumor, as well as repeated bleeding. Simultaneously with a decrease in the percentage of hemoglobin, the number of erythrocytes progressively decreases, the number of leukocytes increases, and the ESR sharply accelerates.
In the later stages of the disease, aniso- and poikilocytosis is observed. In the peripheral blood formula, as a rule, there are no sharp changes, only sometimes there is a slight decrease in lymphocytes and an increase in rod-nuclear leukocytes.
The skin of patients is characterized by increasing pallor. In later stages, the skin becomes sallow gray with a jaundiced tint. Many patients complain of general weakness, fatigue, a sharp decrease in appetite, and inability to work.
Diagnosis of jaw tumors
The nature of the formation of tumors, both malignant and benign, is sluggish, which significantly complicates the diagnosis of the disease in the initial stages. In this regard, contacting specialists and making a diagnosis occurs at later stages of development of the neoplasm. The reason for this is not only the specificity of the disease with a characteristic asymptomatic course, but also the careless attitude of people towards their health, neglect of regular preventive examinations, and a lowered level of awareness of the seriousness of the disease associated with the development of cancer.
It is possible to determine a possible tumor of the jaw through high-quality collection of information provided by the patient about his condition, complaints about any ailments. A thorough examination of the oral cavity and facial skin is also carried out to identify tumors. In the diagnosis of neoplasms, one of the main roles is played by palpation examination, which makes it possible to determine the size and location of the neoplasm. It is also necessary to take x-rays and conduct a computed tomography scan of the paranasal sinuses. A radionuclide study, which records infrared radiation from the human body, can help in making a diagnosis.
The increased size of the lymph nodes located near the neck and in the lower jaw indicates the need for a biopsy. If there is any doubt about determining the nature of the tumor, you should consult with an otolaryngologist and perform rhinoscopy and pharyngoscopy. If there is insufficient information, you should contact an ophthalmologist for qualified advice.
Diagnosis of the disease
First of all, the dentist will conduct an examination. Periostitis is usually quite easy to diagnose. The patient's complaints, external signs and changes in the oral cavity are assessed:
- swelling and redness of the gums, pain when pressed;
- a cushion on the inside of the gum and the presence of a cavity filled with pus (submucosal or subperiosteal abscess);
- a painful, mobile tooth with a crown and roots damaged by caries.
To clarify the stage and depth of periostitis, the doctor may prescribe an x-ray or radiovisiography of the jaw. All studies are carried out in SM-Dentistry clinics using modern equipment.
Treatment of jaw tumors
Basically, all benign tumors are subject to surgical treatment, during which the tumor is removed with excision of the jaw bone to healthy areas. This treatment helps prevent recurrence of the disease. If teeth are involved in the tumor process, then most likely they will have to be removed. In some cases, gentle removal using curettage is used.
Malignant tumors are treated using a complex method, including surgical treatment and gamma therapy; in particularly difficult situations, a course of chemotherapy may be prescribed.
The postoperative period involves orthopedic restoration and wearing special splints.
Osteomyelitis of the jaw - symptoms and treatment
Treatment is carried out only in a hospital under the supervision of a physician and can be medicinal and surgical [9]. Individually, these methods are ineffective and can even harm the patient. Treatment regimens depend on the stage of the disease.
Treatment of acute and subacute osteomyelitis
At the first visit, the neglected damaged tooth is urgently removed. Then the oral cavity is thoroughly washed with antibiotics. This must be done to remove germs and pus from the wound.
In the following days, the wound is treated with disinfectants and injections of antimicrobial drugs are administered. With their help, it is possible to act directly on the source of infection and prevent it from spreading. In addition to the main treatment, nutritional compositions with vitamins C and B are used.
At the subacute stage of the disease, it is important to contain the spread of infection and prevent inflammation from spreading to surrounding tissues.
For this use:
- IVs with antibiotics;
- drugs that reduce or suppress inflammation;
- rubber drainage for exudate drainage.
Vitamin complexes and preparations are also introduced into the bloodstream to cleanse the body of microbes and their waste products. Specific medications and dosages are selected by the attending physician.
Physiotherapy methods can be additional therapy after the main treatment: UHF therapy or treatment with non-constant currents. They are believed to speed up the healing process [7][16].
Treatment of chronic osteomyelitis
If necrotic cavities appear with decay of the bone and surrounding tissue, surgery will be required. To do this, the damaged area is dissected, the affected areas are removed and a splint is applied. Subsequently, using x-ray methods, the doctor monitors how the bone tissue is restored [11].
To help the body fight infection, additional antibiotics are taken in tablets. Metronidazole is most often prescribed and its effect is enhanced by drugs from the group of 3-4th generation cephalosporins.
If the patient's condition does not improve, then fluoroquinolones or Rifampicin are added. The main task of antibiotics is to prevent bacteria from multiplying [7]. Medicines help reduce inflammation and keep the pathological process within the affected area.
Also, the oral cavity is treated daily with bactericidal agents, droppers with vitamins and plasma-substituting fluids are used, which cleanse the body of toxins.
Additionally, it is recommended to rinse your mouth with infusions of chamomile, St. John's wort, mint and comfrey. Herbal remedies reduce inflammation, speed up recovery and have virtually no side effects.