Trigeminal neuropathy (trigeminal neuralgia) is a chronic pain syndrome that involves the trigeminal (5th cranial nerve). Trigeminal neuropathy is a type of neuropathic pain (pain associated with injury or damage to a nerve). The usual or “classic” form of the disease (the so-called “Type 1”) is characterized by attacks of intense pain in the form of a burning sensation or shock that last from a few seconds to two minutes. These attacks can occur in group episodes lasting up to two hours. The “atypical” form of the disease (the so-called “Type 2”) is characterized by constant aching, burning, stabbing pain of somewhat less intensity than with type 1. Both forms of pain can occur in the same person, sometimes at the same time. The intensity of pain can lead to disability, both physical and mental.
The trigeminal nerve is one of 12 paired nerves that exit the brain. The nerve has three branches that carry sensory sensations from the upper, middle and lower parts of the face, as well as the mouth, to the brain. The ophthalmic or superior ramus provides sensory sensation to most of the face, forehead, and front of the head. The maxillary or middle branch provides sensation to the cheek, upper jaw, upper lip, teeth and gums, and side of the nose. The mandibular or inferior branch innervates the lower jaw, teeth and gums, and lower lip. With trigeminal neuropathy, more than one branch may be affected. In rare cases, there may be manifestations of neuropathy on both sides at different times. Even less common is bilateral involvement.
Trigeminal neuropathy occurs most often in people over 50 years of age, although the condition can occur at any age, including in infants. The possibility of developing trigeminal neuropathy increases slightly with multiple sclerosis when it occurs in young people. The rate of new cases is approximately 12 per 100,000 people per year; the disease is more common in women than in men.
Causes
Trigeminal neuropathy can be associated with a variety of conditions. Neuropathy can be caused by blood vessel compression on the trigeminal nerve as it exits the brainstem. This compression causes the protective covering around the nerve (myelin sheath) to wear or become damaged. Symptoms of trigeminal neuropathy can also occur in patients with multiple sclerosis, a disease that damages the myelin sheath of the trigeminal nerve. Rarely, symptoms of neuropathy may be due to nerve compression by a tumor or arteriovenous malformation. Damage to the trigeminal nerve (possibly as a result of oral surgery, stroke, or facial trauma) can also lead to neuropathic pain.
Probability of occurrence
The mandibular nerve fascicle is a fragment of the trigeminal nerve. It provides sensitivity to intraoral and facial tissues, and is responsible for contraction of the facial muscles and dentofacial apparatus. The bundle consists of motor and sensory fibers and nuclei.
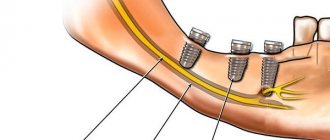
The inferior alveolar nerve (IAN) is located in the lower jaw and is one of the three endings of the trigeminal nerve. The NAN borders the root system of the mandibular arch. In this regard, there is a high risk of damage during dental treatment.
The statistics of nerve damage are especially high during the period when dental operations were performed without the use of modern technologies.
According to the latest data, the incidence of nerve damage during dental implantation does not exceed 3%. Of this number, only 1.7% end up with permanent neuropathy.
According to some dentists, these data are underestimated, and the percentage of damage to NAS reaches 30%. In any case, this issue should be given sufficient attention.
Symptoms
The intensity of pain from trigeminal neuropathy varies depending on the type of neuropathy, and can range from sudden, severe and stabbing to constant, aching, burning. Intense attacks of pain may be triggered by vibration or contact with the cheek (for example, when shaving, washing the face or applying makeup), while brushing teeth, eating, drinking water, talking, or being exposed to wind. The pain may involve a small area of the front of the face or may cover a large area. Attacks of pain rarely occur at night when the patient is sleeping.
NTN is characterized by attacks of pain that stop for a while and then return, but the disease can progress. Attacks of pain often get worse over time and pain-free periods become shorter. Eventually, pain-free intervals disappear and medications used to control pain become less effective. The disease is not fatal, but can be debilitating for the patient. Due to the intensity of the pain, some patients may avoid daily activities or social contacts because they are afraid of the sudden onset of an episode of pain.
Diagnostics
The diagnosis of trigeminal neuropathy is based primarily on the patient's medical history, symptoms, and physical and neurological examination findings. To make a diagnosis of NTN, it is necessary to exclude other diseases that may manifest as pain in the facial area. Some conditions that cause facial pain include: post-herpetic neuralgia, headaches, and temporomandibular joint disorders.
Due to the commonality of symptoms and the large number of conditions that can lead to facial pain, making a correct diagnosis is often difficult, but finding out the exact cause of the pain is very important, since treatment tactics for different types of pain may differ.
Most NTN patients will eventually need to undergo a magnetic resonance imaging (MRI) scan to rule out a tumor or multiple sclerosis as the cause of the pain. This test method can clearly show the compression of a nerve by a blood vessel. Special MRI techniques can reveal the presence and degree of compression of a nerve by a blood vessel.
The diagnosis of classic trigeminal neuropathy can also be confirmed by the positive effect of taking anticonvulsant medications for a short period of time. Diagnosis of T2 is more complex and difficult, but is usually confirmed by a positive response to low-dose tricyclic antidepressants in the same way as other neuropathic pain.
Treatment
Treatment options include medication, surgery, and multimodal treatment.
Medications
Anticonvulsants, used to block nerve stimulation, are generally effective in treating type 1 NTN but are often less effective in treating type 2 neuropathy. These drugs include carbamazepine, oxcarbazepine, topiramate, gabapentin, pregabalin, clonazepam, phenytoin, lamotrigine, and valproic acid.
Tricyclic antidepressants such as amitriptyline or nortriptyline may also be used to treat pain. Analgesics and opioids are usually not effective for treating acute, recurrent pain caused by T1, although some patients with T2 respond to opioids. Ultimately, if treatment does not relieve pain or results in significant side effects such as cognitive impairment, memory loss, excessive fatigue, bone marrow suppression, or allergies, then surgery may be recommended. Because trigeminal neuropathy is most often a progressive disease that becomes drug-resistant over time, patients often seek surgical treatment.
Surgery
Several neurosurgical techniques are generally used to treat NTN, depending on the nature of the pain, the wishes of the individual, physical health, blood pressure and the presence of previous operations. Some procedures are performed on an outpatient basis, while others, which are performed under general anesthesia, are performed in a hospital setting. After these surgical procedures, there may be some reduction in the face and it is not uncommon for NTN to recur, even if the procedure was initially successful. Several procedures will be used. These are like:
- Rhizotomy is a procedure in which nerve fibers are damaged to block pain. Rhizotomy to treat NTN always causes some degree of sensory loss and facial numbness.
- Glycerin injections are an outpatient procedure that is performed after light anesthesia. This form of rhizotomy usually results in pain relief within 1-2 years. However, this procedure can be repeated several times.
- Radiofrequency thermal ablation is most often performed in an outpatient setting.
- Stereotactic radiosurgery (using Gamma Knife or CyberKnife) uses CT scanning to deliver highly focused radiotherapy to the area where the trigeminal nerve exits the brain stem. This causes slow nerve damage, which disrupts the transmission of sensory signals to the brain. Patients who have had this procedure can go into remission for up to three years.
- Microvascular decompression is the most invasive of all surgeries for treating NTN, but it also has the best long-term results and the lowest likelihood of pain recurrence. About half of people who have this procedure will experience periodic pain for 12 to 15 years.
- A neurectomy, which involves a partial incision of the nerve, can be performed at the nerve's entry point into the brainstem while attempting microvascular decompression. A neurectomy can also be performed by cutting the superficial branches of the trigeminal nerve on the face.
Surgical management of T2 is usually more problematic than for T1, especially where vascular compression is not detected on neuroimaging.
Additional treatments
Some patients benefit from combining medications with other treatment methods. These methods have varying degrees of effectiveness. Some patients find that gentle exercise, yoga, creative visualization, aromatherapy, or meditation can help. Other treatment options include acupuncture, chiropractic care, biofeedback, vitamin therapy, and nutritional therapy. Some patients note a certain effect from the use of botulinum toxin.
The tongue is a complex organ involved in speech, chewing, swallowing, breathing, taste perception and sensitivity [3]. The innervation of the tongue is carried out by a number of cranial nerves - hypoglossal (Liegbott, 1986), glossopharyngeal, lingual (Liegbott, 1986; Zur et al., 2004), chorda tympani (Liebgott, 1986; Zur et al., 2004; Fonseca, 2005). Of particular interest are the anatomical and topographical features of the structure of the lingual nerve, since there is a high probability of its damage during the removal of the lower third molar.
Literature data indicate that the lingual nerve is located along the inferior alveolar nerve and then separates from it at the level of the auditory ganglion [23, 30]. In studies by S. Kim et al. (2003) showed that the place of bifurcation of the lingual and inferior alveolar nerves is at the level of the auditory ganglion above the mandibular notch only in 65.6% of cases; in other cases, the bifurcation site is located below the upper half of the mandible between the mandibular notch and the lingula of the mandible (25%) or in the lower half of the mandible (3.1%); in 6.3% of cases, a plexiform (complex) type of branching was observed.
According to the authors, the cross-section of the lingual nerve is different throughout its entire length; for example, it was found that in the retromolar region the cross-section was round (40.6%) or oval (40.6%), the average diameter of the lingual nerve in this region was 2.3 mm (the minimum diameter in the retromolar region was 1.5 mm , maximum - 3.5 mm); the cross-section of the lingual nerve in the region of the third lower molar is usually oval in shape (59.4%), but round (25%) and flat (18.7%) sections were also observed; in the area of the second lower molar, in most cases the band form predominated [17].
The collateral nerve branches of the lingual nerve additionally innervate the retromolar space and are of the anatomical and topographic structure of the lingual nerve [19, 23, 28, 30]; however, according to J. Garbedian (2009), the collateral nerve branches of the lingual nerve innervate not only the retromolar space, but also the region of the lower third molar (81.2%). Such a high percentage of the presence of additional nerve branches of the lingual nerve indicates that this anatomy -the topographic structure of the lingual nerve should be considered as the normal structure of the lingual nerve, and not its variations [17].
J. Kiesselbach and J. Chamberlain [16], M. Pogrel et al. [21], M. Miloro et al. [20] argue that the lingual nerve is located at or above the alveolar ridge ( crista alveolaris
) in 17.6% of cases. B. Behnia et al. [2] also noted a similar position of the lingual nerve in 10% of cases. In addition, according to some authors, the average distance from the lingual surface of the alveolar ridge to the lingual nerve is 4.45 mm in the retromolar region [21] and 2.28 mm [16] or 3.01 mm [2] in the region of the third inferior molar However, according to research by S. Kim et al., the distance between the same anatomical structures in these areas is 10.0 mm.
The position of the lingual nerve in the region of the lower third molar may vary depending on the shape of the alveolar ridge and the distance between the mandibular ramus and the third molar [9]. In most cases, the alveolar ridge in the third molar region protrudes and deviates lingually, thereby affecting the position of the lingual nerve.
The most common procedure in outpatient surgical practice is the removal of third molars [5, 27]. According to S. Quek (2003) and S.V. Shishkin (2008), a significant number of removals occur in the lower jaw. The success of the removal of third molars depends on the correct assessment of the degree of complexity, the quality of the surgical intervention and the identification of the individual characteristics of the patient; all these factors individually or in combination can lead to the development of complications.
According to the literature, the largest number of complications (43.7%) in the practice of a dental surgeon is associated with the removal of the lower third molars (C. Phillips et al., 2003). The reasons may be: anatomical and topographical features of the retromolar space; location of the third lower molar; the presence of an inflammatory or chronic process in this area; incorrectly chosen treatment tactics [12, 22]; in addition, the age of the patient is important [8, 14, 24, 26]. In some cases, after the removal of lower third molars, patients may complain of a feeling of “numbness,” burning, pain in the tongue, changes in salivary secretion on the affected side, as well as loss of taste and changes in speech [15]. These complications are often associated with damage to the lingual nerve ( n. lingvalis
) during surgery.
Damage to the lingual nerve is one of the serious complications of third molar removal surgery. According to a number of authors, it is observed in 0.06-10% of cases [1-4, 6, 7, 10, 13, 18, 29]. However, damage to the lingual nerve can also occur in a number of other cases, for example, due to careless operation of the elevator, installation of dental implants (Berberi et al., 1993), detachment of the mucoperiosteal flap on the lingual side, osteomyelitis of the mandible [15] and anesthesia (Hillerup and Jensen, 2005). Clinically, this complication is manifested by dysesthesia, hypoesthesia and paresthesia in the tongue. According to Blondo (2007), paresthesia after removal of the third lower molar was observed in 0.4-0.8% of cases. According to a retrospective analysis by Haug (2005), after the removal of 8 thousand third lower molars, the prevalence of injury to the lingual nerve was <2%. In most cases, the development of paresthesia was facilitated by the apposition of the tooth roots to the inferior alveolar nerve or dystopia of the tooth in the lingual direction. Holmes and Lam (2002) reported that approximately 75% of lingual nerve injuries result from mandibular third molar extraction.
Neurological disorders associated with nerve injury during surgery are usually long-term in their course. On average, sensitivity disorder is observed from 2 weeks to 6 months. In 0.5-1.0% of cases, the effects of nerve injury remain with the patient for life (Blackburn and Bramley, 1989; Jerjes et al., 2006). The prevalence of long-term paresthesia (over 6 months) is ≤0.9% for the inferior alveolar nerve, ≤0.5% for the lingual nerve (M. Pogrel, 2007). These disorders cause discomfort to the patient when eating, talking, and limiting his social activities. Iatrogenic damage to the lingual nerve can adversely affect the professional activity of a dental surgeon and, in some cases, cause him to be brought to legal liability [11, 25].
Knowledge of the anatomical and topographical features of the structure and location of the lingual nerve is invaluable for a practicing dental surgeon, especially when removing dystopic and impacted wisdom teeth, which will significantly reduce complications of neurogenic origin associated with possible damage to this nerve.