An abscess on the tongue can appear in a person of any age. Children often suffer from this condition. If an abscess appears on the surface of the tongue or on the side, then treatment is necessary urgently, otherwise the infection will begin to spread further, and such formations will cover the entire oral cavity. Any injury can result in the appearance of a boil due to bacteria, fungi or viruses entering the area. You can cure such a disease yourself only if the boil on the tongue has appeared recently, and the inflammation has not had time to spread to neighboring tissues.
Abscess on the tongue - what is dangerous about an abscess in the mouth and how to remove it without consequences
Tongue abscess is a serious pathological condition, which is characterized by the appearance of a purulent neoplasm against the background of rapid spread of inflammation. In this case, the patient begins to experience severe malaise, the body temperature may rise sharply, and the organ itself will become swollen, which will result in problems with diction, eating, and even breathing. As part of the diagnosis, the doctor may suggest performing a puncture to find out more about the contents of the abscess. Today we’ll talk about the reasons why a purulent process can begin to develop, what accompanying symptoms are characteristic of this condition, and what methods of treating an abscess are used today.
How to distinguish a boil from other formations in the mouth
A furuncle, as medicine defines it, cannot form in the mouth due to the absence of hair follicles in this cavity, in which the infectious process begins during furunculosis. Abscesses in these places are abscesses due to local tissue inflammation.
Abscesses occur on:
- gums;
- sky;
- tongue and in the area under it;
- cheek tissues.
The danger lies in the possible breakthrough of the boil into the oral cavity.
Differential diagnosis allows the dentist to evaluate symptoms and separate non-odontogenic processes from formations of odontogenic origin. The main difference between boils and carbuncles and odontogenic abscesses and phlegmons is the purulent-necrotic core. With sialadenitis, suppuration is noted, the presence of a stone in the duct of the major salivary glands, which is determined by palpation or x-ray. Suppurating soft tissue cysts are anamnestically preceded by a soft elastic formation. The puncture shows the presence of fluid. An odontogenic source of inflammation in the mouth cannot be detected.
Features of a purulent abscess
An abscess on the oral mucosa is a kind of abscess, which is characterized by severe inflammation and the formation of purulent masses. Gradually, it leads to the death of living tissue, and in an advanced stage it is accompanied by a general deterioration in the patient’s condition and the appearance of severe pain during talking, chewing food and even breathing. Obviously, this pathology can provoke very serious consequences for the body as a whole, so under no circumstances should an abscess in the oral cavity be ignored.
The photo shows a tongue abscess
An abscess of the root of the tongue, as, in fact, of any other part of this organ, is quite readily treatable, but requires an integrated approach to solving the problem. It is important to understand here that the sooner inflammation is detected, the easier and faster it can be eliminated. The pathology in question has a serious impact on the overall health and immunity, so do not hesitate with treatment.
Symptoms of a fistula on the gum
The main sign of the formation of a gingival fistula is the appearance of a fistula tract on the surface of the gum.
In addition, symptoms indicating the development of a pathological process include:
- the appearance of toothache of high or medium intensity and aggravated by touch, with chewing load;
- discharge of purulent masses from the fistula tract;
- excessive tooth mobility;
- inflammatory lesion of the gums in the area of the entrance opening of the fistula;
- temperature increase.
Most often, a gum fistula is diagnosed based on the results of a standard dental examination. If necessary, the dentist may invite the patient to undergo an X-ray examination, which provides the opportunity to determine the depth of gum damage, the degree of granuloma growth under the tooth and the presence of an inflammatory process in the periosteum area.
Reasons for the formation of an abscess on the tongue
Most often, the formation of a purulent focus on the body and the root of the tongue in particular becomes a consequence of mechanical or thermal effects. Damage opens a direct path for the penetration and spread of bacterial infection. As practice shows, the formation of an abscess is often preceded by injury to the mucous membrane with sharp fish bones.
“In my case, the abscess was generally the result of my passion for dried vobla! Once again I accidentally scratched the edges of my tongue, then it turned red, began to hurt, and one fine morning I discovered a small abscess on it. I was scared, of course, and immediately made an appointment with a doctor. Fortunately, everything worked out without surgical intervention. The doctor prescribed rinsing with chlorhexidine.”
Anna Semenova, 43 years old, Omsk, from correspondence on the forum www.32top.ru
Quite often, the oral mucosa is injured by sharp edges of teeth or crowns, as well as worn-out prosthetic structures and incorrectly adjusted orthodontic devices for correcting the bite. Patients suffering from periodontitis, ulcerative stomatitis, and acute tonsillitis are also at risk. In this case, pathogenic bacteria can spread from the source of chronic infection in the oral cavity. Thus, to date, experts in the field of dentistry have identified the following main reasons for the development of pathology:
- penetration of infection, staphylococci and streptococci,
- trauma to the mucous membrane,
- imbalance of oral microflora,
- dental diseases,
- glossitis,
- stomatitis,
- tonsillitis.
Trauma to the tongue can cause an abscess.
It should also be noted that quite often an abscess develops after a burn as a result of consuming too hot food or drinks. Infection can also appear through fresh scratches from hard foods or sores caused by eating spicy or salty foods.
Abscess on the gum with periodontitis -
Gum suppuration can look completely different, but in any case, the formation of an abscess on the gum always occurs in the projection of the causative tooth. If the cause of suppuration is an infection in the root canals, then you will always see an old filling or crown on the causative tooth, or the tooth will be partially destroyed. In this case, infection in the root canals gradually leads to the development of a focus of chronic inflammation at the apex of the tooth root.
In dentistry, such inflammation of the tooth is called chronic periodontitis. From time to time, an exacerbation of chronic inflammation may occur, and in this case, pus begins to form at the apex of the tooth root, which comes out through the bone tissue and penetrates under the gum, forming an abscess there. Therefore, please note that with periodontitis, an abscess on the gum most often forms not at the gingival edge, but closer to the projection of the apex of the root of the causative tooth.
Abscess on the gum with periodontitis: photo
Symptoms - an abscess with periodontitis may look like a slight swelling of the gums in the area of 1 tooth or in the area of several teeth, if a significant purulent abscess has formed - flux (Fig. 4). Typically, the appearance of gum swelling is preceded by pain when biting one of the teeth. The pain can be acute, but sometimes purulent inflammation can occur without pain. Sometimes, in the projection of gum suppuration, swelling of the soft tissues of the face appears.
The abscess formed under the mucous membrane of the gums can burst with the formation of a fistula opening (Fig. 7-8). The fistula opening is connected through a fistulous tract to the source of inflammation at the apex of the tooth root. Therefore, gradual discharge of pus may be observed from the fistula openings. As soon as the acute inflammation at the root apex subsides and the process of pus formation stops, the fistula openings can close, but only until the process worsens again.
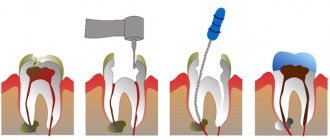
X-ray diagnostics - if you have a fistula or a purulent sac on your gum, treatment is only possible at the dentist. Before starting treatment, you need to take an x-ray to confirm the presence of inflammation at the apex of the tooth root (24stoma.ru). The image will also show the quality of root canal filling, if it was performed previously. It’s sad, but according to official statistics, dentists fill root canals poorly in as many as 60-70% of cases.
The most common mistake dentists make is not filling root canals up to the apex of the tooth root, as a result of which infection begins to multiply in the part of the root canal that is not filled with filling material. As a result, a focus of chronic inflammation develops at the apex of the tooth root, for example, in the form of a cyst or granuloma. Below you can see what cysts and granulomas look like on a diagram, an x-ray, and also on the apex of the root of an extracted tooth.
Treatment of gum suppuration during periodontitis -
If, against the background of an exacerbation of chronic periodontitis, an abscess appears on the gum, then what to do will depend on the results of examining the tooth and analyzing the x-ray. In some cases, it may turn out that the tooth can no longer be treated, and then you will be referred to a surgeon for removal. However, in most cases, it is possible to cure such a tooth, and then the doctor’s algorithm for further actions will depend on whether root canal filling was previously performed in this tooth.
1) If the root canals are not filled –
This greatly facilitates the doctor’s work, because... in this case, the dentist will not have to go through the trouble of unsealing poorly filled root canals. In this case, a standard method of treating periodontitis is used, which includes mechanical treatment of the root canals + treatment of the inflammation at the root apex. On your first visit, the dentist will remove your old filling or crown, drill out tooth tissues destroyed by caries, and perform a mechanical expansion of the root canals to allow pus to drain out through them.
After this, the dentist will prescribe you antibiotics, antiseptic rinses, and will most likely send you to a surgeon to make an incision in the gums, which is necessary to create a good outflow of pus. After 3-4 days, the dentist will make an appointment for you again to complete the mechanical treatment of the root canals and seal them. If the lesion is small at the apex of the tooth root, the doctor can immediately perform a permanent filling of the root canals with gutta-percha. But usually, the canals first have to be filled with temporary medicinal paste for a period of 1-2 months, and only after that permanent filling with gutta-percha is carried out.
How the gum incision is made - the incision is usually completely painless and is performed under local anesthesia. If the abscess is small, the size of the incision usually does not exceed 5-7 mm, but if a large purulent abscess develops (as in the video below), the incision is made up to 1.5 cm. After opening, pus comes out of the gum, then the wound is washed with antiseptics and into it a small rubber drain is inserted.
2) If the canals in the tooth are sealed poorly -
If the dentist sees on an x-ray that the cause of suppuration lies in poor-quality root canal filling performed earlier, then there are 2 possible treatment options. This is either a standard treatment of periodontitis with preliminary filling of the root canals, or a minor surgical operation (resection of the root apex)…
- Standard therapeutic treatment - on the first visit, the dentist drills out the old filling, removes the crown and tries to unfill poorly filled root canals.
Next, the canals are washed with antiseptics, the tooth is left open for several days + antibiotics are prescribed. If necessary, the patient is also sent to a surgeon for a gum incision. Thus, unlike the previous treatment option, only 1 point has been added here - unsealing the root canals. When the inflammation subsides after a few days, first, either temporary filling of the canals with medicinal paste, or immediate permanent filling with gutta-percha can be carried out. The medicinal paste is left in the canals for a period of 1 to 3 months. During this period, an x-ray will be taken to record a decrease in the size of the focus of chronic inflammation at the apex of the tooth root. When the lesion disappears or becomes small, the canals will be sealed with gutta-percha and a permanent filling or crown will be placed. - Resection of the root apex (Fig. 13) –
This method allows you not to re-treat root canals or remove the crown from the tooth.
It consists of making a small incision in the projection of the apex of the tooth root on the gum, through which the doctor uses a drill to cut off the apex of the root with the unfilled part of the root canal from the tooth. Also, a cyst or granuloma is scraped out of the wound. However, the operation can only be performed on those patients whose root canal is poorly filled only at the very apex of the root. Root resection is a very simple operation and usually takes only 25-35 minutes. It is easiest to carry out on the front teeth, much more difficult on the side teeth. Low cost of the operation + no need to spend money on replacing the crown and re-treating the tooth. The operation is performed after the acute inflammation has been relieved, which may require an incision and antibiotic therapy.
→ Root apex resection operation
Characteristic symptoms
The pathology is characterized by a fairly rapid pace of development. Based on where exactly the neoplasm is localized, experts distinguish between deep and superficial forms of abscess. Let's look at each of them in more detail.
Surface view
In this case, an abscess occurs on the back of the organ. The person experiences acute pain during swallowing, which often radiates to the ear. As part of a visual examination, noticeable swelling of the mucous membrane can be detected; when touched, a compaction can be clearly felt. Such an abscess can open without outside help, but in any case professional treatment is necessary.
Deep view
This is a more dangerous form of pathology, in which purulent processes develop in the thickness of the tissues of the organ. Experts include the following conditions as associated symptoms:
- general weakness,
- poor appetite
- restless sleep due to constant painful sensations,
- tachycardia,
- heat,
- enlarged lymph nodes,
- increased salivation,
- severe swelling of the organ, acute pain,
- blue mucous membranes, formation of gray plaque,
- the appearance of bad breath.
The main danger is that when an abscess develops, the tongue greatly increases in size. As a result, problems arise not only with speech, but also with breathing.
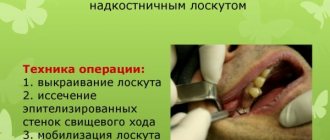
Treatment methods for boils in the mouth
Diagnosis of pathology does not cause great difficulties. The diagnosis is made by examining the mucous membrane in the dental office. Before taking, you can rinse your mouth with warmed liquid antiseptics and take analgesics. Boils in the mouth should be treated exclusively surgically (intraorally and extraorally). To prevent a widespread inflammatory process, the dental surgeon opens and drains the formation. The opened cavity is subject to mandatory antiseptic treatment. No stitches are required due to the small size of the incision. After getting rid of the yellow-white pus, the patient notes an improvement in health, minimization of pain, and subsidence of swelling. If the abscess has deformed facial features, they are restored after surgery. At the post-surgical stage, broad-spectrum antibiotics are indicated, antiallergic tablets, immunostimulants and vitamin preparations are prescribed. Physiotherapy in dentistry is rarely prescribed, but in some cases doctors prescribe fluctuarization or UHF. The current (symmetrical, asymmetrical bipolar or unipolar) at the first exposure has a strong irritating effect.
Fluctuarization is used in the acute stages of abscess formation. The procedure relieves tissue inflammation, minimizes the purulent process, promotes the rejection of necrotic masses and the evacuation of decay products. UHF can also be used when symptoms subside. A fifteen-minute effect on the affected area shows a pronounced anti-inflammatory effect, relieves pain and swelling.
As for nutrition, patients are advised to temporarily abandon solid food in favor of pureed, soft food.
How is diagnostics carried out?
At the first appointment, the doctor is obliged to ask the patient about all the symptoms that worry him. He also needs to find out the circumstances under which the mucous membrane was injured. Next, the specialist sends the patient for blood tests, since the formation of an abscess usually causes a significant increase in the level of leukocytes and ESR.
For diagnosis, a blood test is required.
In order to identify the pathogen, bacterial culture is performed. The patient may also be referred for an X-ray examination, which will help detect the source of the infection, especially if there are complications. Competent diagnosis makes it possible to distinguish between diseases such as tongue abscess and Ludwig's tonsillitis, lymph node abscess, lymphadenitis.
Causes of appearance in the oral cavity
Dental pathologies of an inflammatory or systemic nature are often complicated by abscesses - periodontitis and periodontal disease, in which destructuring of the periodontal joints occurs with the formation of certain periodontal cavities in which pathogenic microorganisms rapidly multiply. Improperly installed dentures, braces, brushing with too hard a brush, or intensively removing deposits with a toothpick can disrupt the integrity of the mucous membrane with further formation of an abscess. There are frequent cases of infection as a result of improper dental procedures. Sometimes an abscess in the mouth forms against the background of suppressed immunity due to previous (or ongoing) influenza, ARVI and other diseases. Often the cause is a boil on the face, a staphylococcal, streptococcal process in the pharynx (tonsillitis).
Common etiologic agents are bacteria:
- Staphylococcus aureus.
- Gram-negative anaerobic bacteria.
- Streptococcus.
An abscess is a limited, dense hemisphere surrounded by swollen tissue, painful when touched.
Possible complications
The pathological condition under consideration, especially if the formation of an abscess occurs at the very root of the organ, is fraught with serious consequences for the entire organism as a whole. If treatment is not started in time, the abscess may well result in serious complications. Thus, in advanced stages it is often accompanied by purulent inflammation of the tissue - the formation of phlegmon, the occurrence of sepsis and severe intoxication of the body, and this, in turn, can lead to death.
Treatment of tongue abscess
Conservative therapy involves taking antibiotics and rinsing with antiseptic agents, such as Furacilin or Chlorhexidine. However, such treatment can be effective only at the earliest stage of pathology development. If the situation is advanced, immediate surgical intervention will most likely be required. The dentist will perform an emergency opening of the abscess, thereby preventing further spread of the infection. If a purulent neoplasm has formed deep at the base of the organ, the doctor may perform an autopsy from the outside under the chin. After removing purulent discharge, the specialist will thoroughly rinse the cavity using antibiotics and proteolytic enzymes1.
In some cases, surgery is performed to remove the pus.
In the most advanced cases, when the patient is already experiencing serious breathing difficulties, a tracheotomy is performed. The patient is prescribed antibiotics, anti-inflammatory drugs and antihistamines. To strengthen the body's defenses, it is recommended to take multivitamin complexes and regularly rinse the mouth with antiseptics, including decoctions of medicinal herbs - chamomile and sage. It is important to understand here that the use of any pharmaceutical drugs and traditional medicine must be agreed upon with the attending physician.
Prognosis and prevention
The success of treatment largely depends on how deeply the infection has spread and how quickly the person receives medical care. If an abscess is diagnosed in a timely manner, the likelihood of a favorable outcome will be at the highest level - the disease can be cured in just a couple of weeks. If the problem is neglected, the situation may result in the development of phlegmon and sepsis. To prevent the appearance of an abscess on the tongue, including relapses, it is enough to follow the recommendations of doctors:
- pay close attention to oral hygiene, brush your teeth and tongue twice a day,
- minimize the consumption of too spicy and salty foods,
- take care of the condition of the oral cavity, try not to injure the mucous membrane with foreign objects,
- in case of accidental damage, you should thoroughly rinse your mouth with water and an antiseptic solution, and also, just in case, consult a specialist to eliminate the risk of infection of the wound,
- strengthen the immune system - a healthy lifestyle, frequent walks in the fresh air, sports and proper nutrition,
- systematically visit the dentist for preventative care.
Preventive examinations with a dentist will help you avoid problems.
If you detect any suspicious changes in the condition or appearance of the oral cavity, you should definitely consult a doctor for advice. It is better to waste your time and go to a specialist than to undergo long and grueling treatment.
Home remedies
To speed up the wound healing process after treatment, you can resort to proven home methods. Here it should immediately be noted that their use is justified only if the attending physician has given his consent. Here are some reliable tips:
- rinsing with a light saline solution at the rate of 2 teaspoons per glass of water at room temperature,
- treating wounds with a solution of hydrogen peroxide or Chlorhexidine,
- applying a piece of ice to relieve acute inflammation.
Tongue abscess is a disease that is inevitably accompanied by very unpleasant symptoms. A general deterioration in health, high temperature, pain, problems with speech and breathing are only a small part of what the development of such a serious and dangerous phenomenon in an advanced stage entails. To prevent the situation from worsening, consult a doctor immediately when the first signs of pathology appear.
- Vernadsky Yu.I. Fundamentals of maxillofacial surgery and surgical dentistry, 2003.